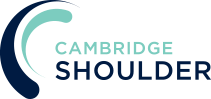
Anterior Dislocations
Anterior SCJ Dislocations
- Anterior Dislocations of the SCJ are rare
- Dislocations can either be Traumatic, as the result of a significant injury, or Atraumatic, due to a combination of tissue laxity and muscle imbalance
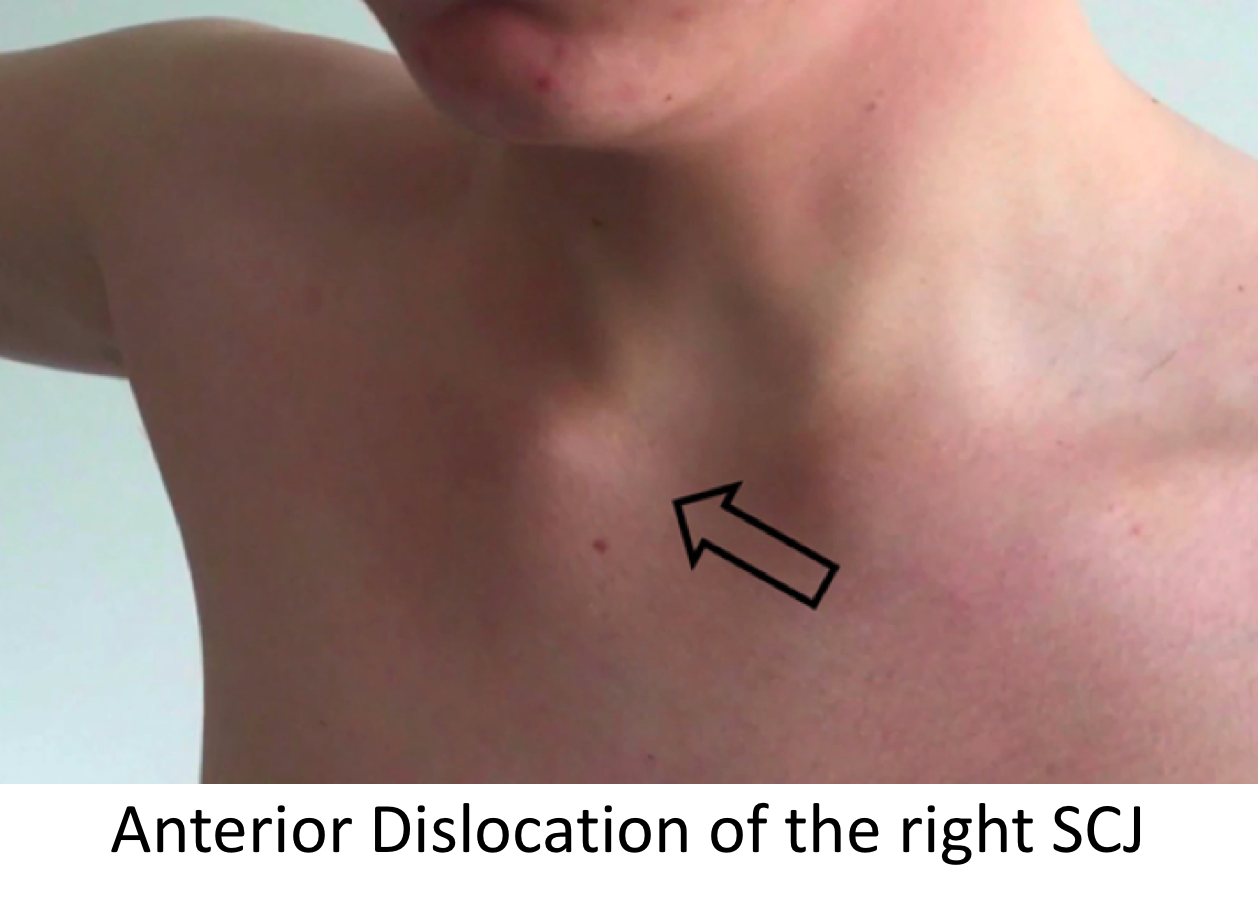
SCJ Stabilising Structures
- The SCJ is held in joint by a combination of Static and Dynamic stabilising structures that work together to create an ‘envelope’ of stability
- Static Stabilisers - these are the capsular and ligamentous structures that surround the joint and include,
- Anterior & Posterior Sternoclavicular Ligaments
- Interclavicular Ligament
- Costoclavicular Ligaments
- Dynamic Stabilisers – the various muscles that attach to the clavicle and sternum all create a certain pull on the bones. The pull of these muscles is co-ordinated to precisely balance each other out, creating a ‘dynamic equilibrium, similar to guy ropes holding up a tent. Key muscles include,
- Subclavius
- Sternocleidomastoid (SCM)
- Pectoralis Major
- Static Stabilisers - these are the capsular and ligamentous structures that surround the joint and include,
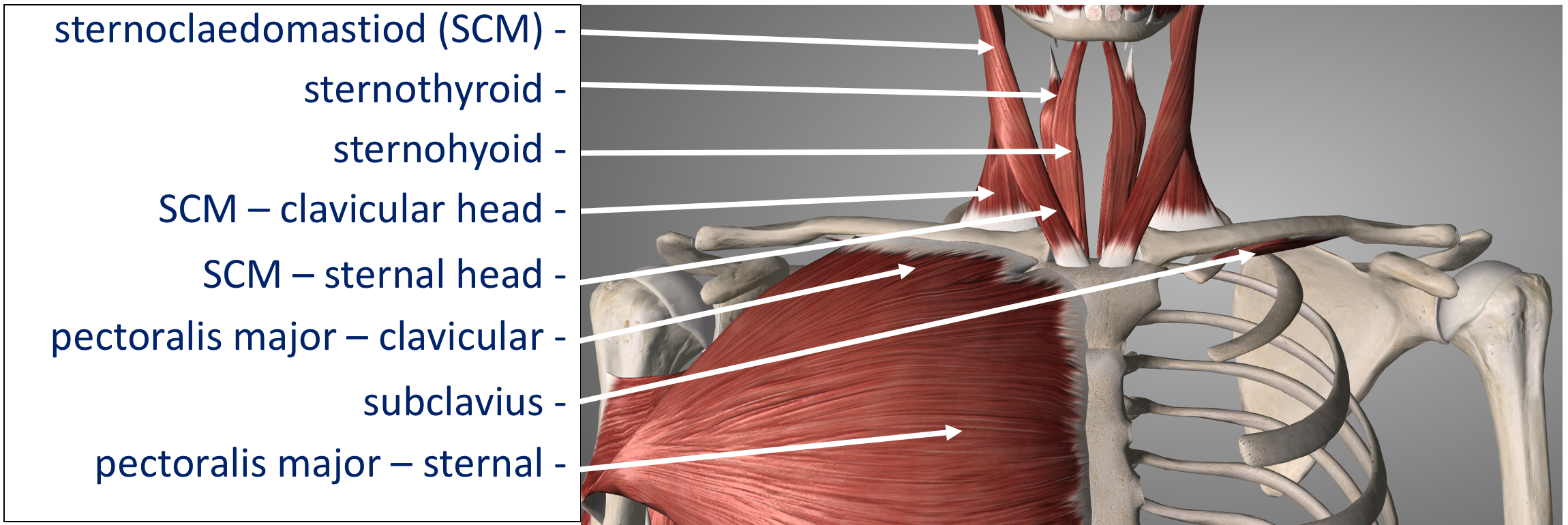
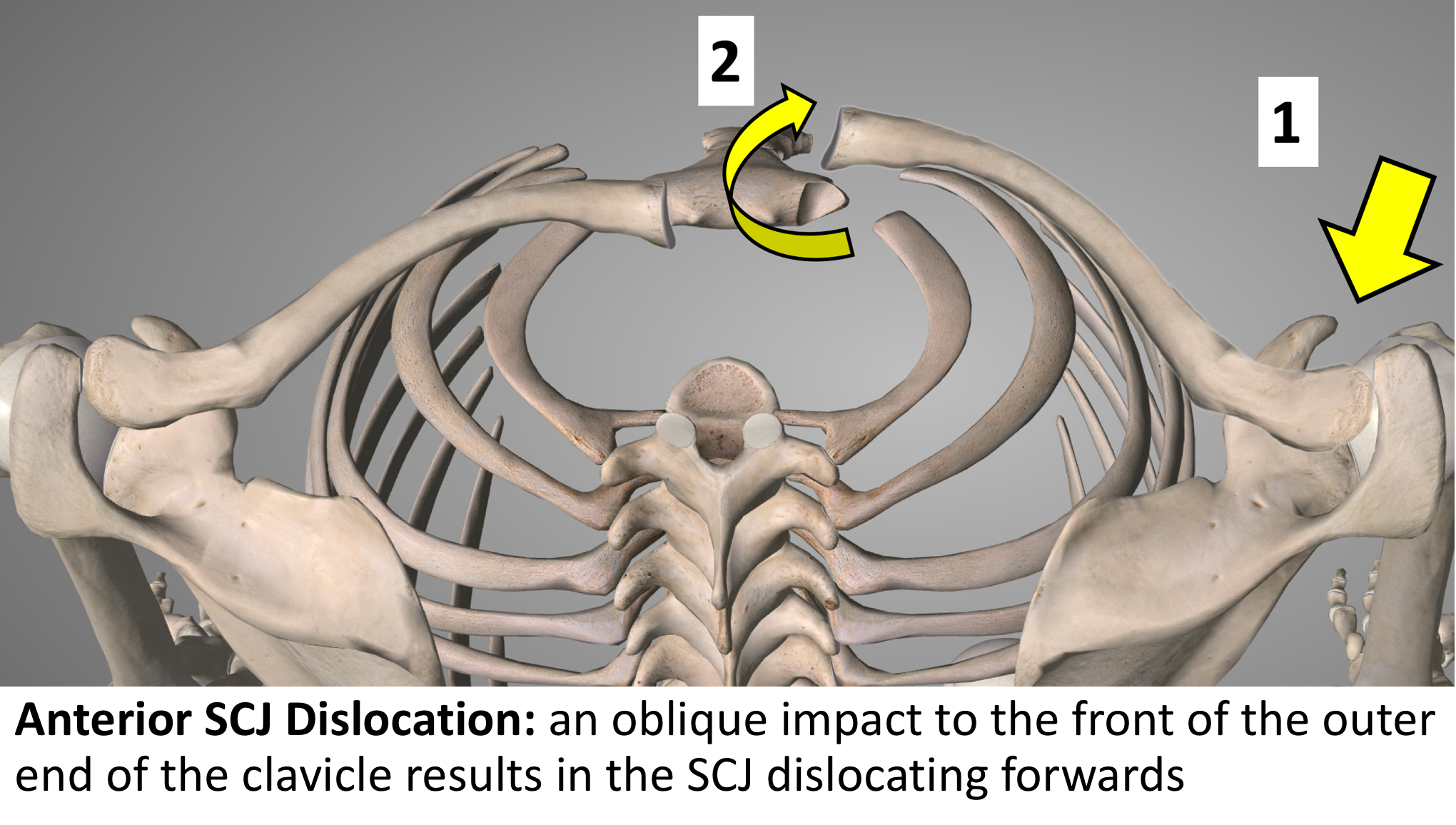
What Happens? – Mechanism of Injury
- Traumatic SCJ Dislocation
- Traumatic SCJ Dislocations occur as the result of a significant injury that results in the sternoclavicular, interclavicular and costoclavicular ligaments being torn
- The mechanism of injury is due to an indirect, oblique force aimed backwards on to the shoulder
- This force causes the lateral end of the clavicle backwards whilst rotating the medial end forwards, away from the sternum, rupturing the ligaments
- Sometimes the medial end of the clavicle spontaneously falls back into position and sometimes it remains dislocated
- Atraumatic SCJ Dislocation
- Atraumatic SCJ Dislocations tend to occur in younger patients under the age of 20 years
- Sometimes there is a relatively minor indirect force that precipitates the initial dislocation but, usually, the SCJ spontaneously begins to dislocate without an injury
- The medial end of the clavicle dislocates due to a combination of increased laxity in the stabilising ligaments and an abnormality in the sequence in which the envelope of stabilising muscles work
- Usually the clavicular part of Pectoralis Major and the sternal part of SCM do not relax in sequence, resulting in the clavicle being pulled forward and the sternum backwards
How do you Diagnose an Anterior SCJ Dislocation?
As with any condition assessment begins with a history and examination of the patient. These can be very different following an ACUTE injury when compared to a CHRONIC problem
- History -
- Patients who have Traumatic instability will usually have sustained an initial injury resulting in dislocation of the joint
- A detailed history of the initial injury, how it was treated and whether there were any other associated problems is required
- On-going symptoms of recurrent dislocations, and when they occur, pain and restriction of function are very relevant
- Patients with Atraumatic instability usually will not have had an initial precipitating injury, but will have noticed that their SCJ has become unstable
- The joint tends to come out whenever they lift their arm up or backwards but relocates, back into joint, when they bring their arm down
- Examination –
- Following an ACUTE traumatic dislocation it is important to assess whether the joint has fully relocated and for any other injuries, including neurovascular injuries, around the shoulder girdle
- In the more chronic case it is initially important to assess the contour of the joint for any abnormality, when compared to the un-injured side. In some cases the joint can have remained dislocated
- Any pain or discomfort around the joint is important
- On moving the joint through a full range, including protraction and retraction, any instability can be detected
- For patients with Atraumatic instability it is important to assess for any generalised joint laxity
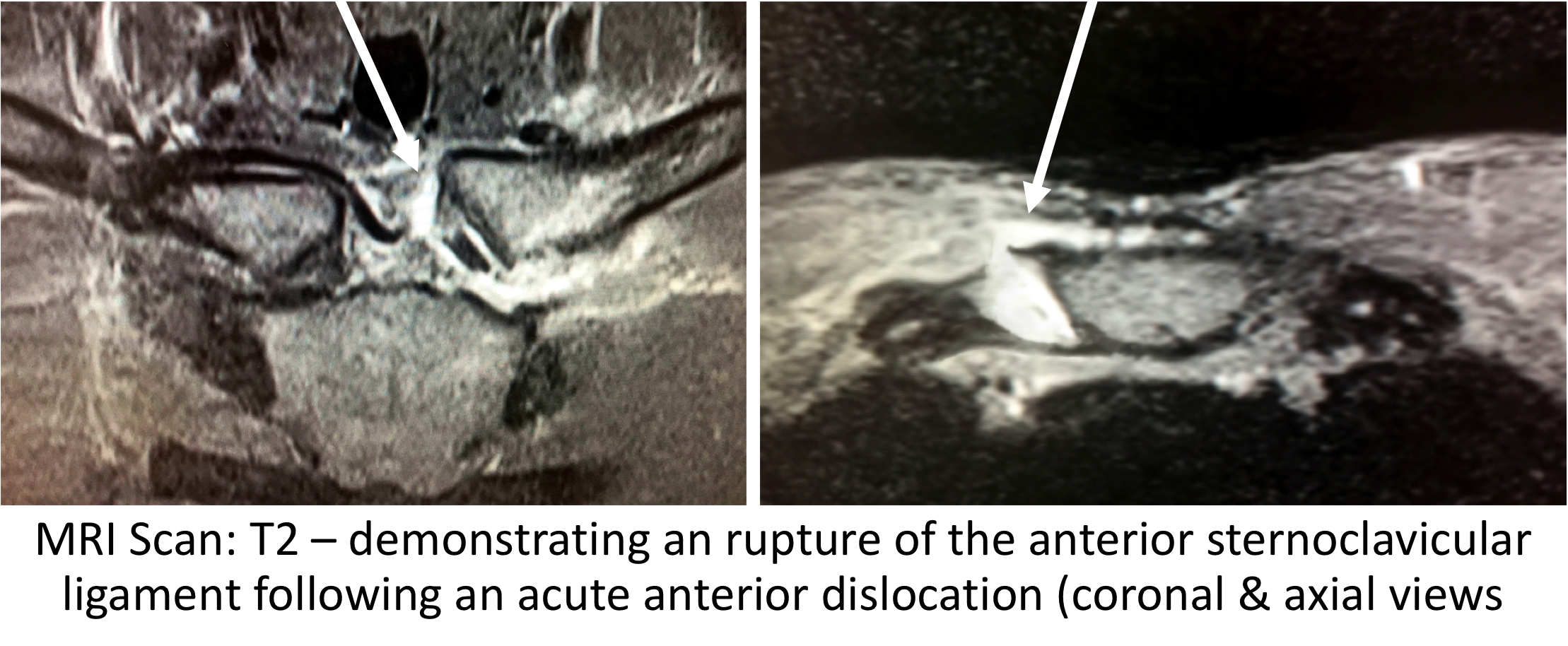
- Investigations
- X-Ray - due to the central position of the SCJs and the spinal column that lies behind it, routine x-rays are very difficult to interpret and are not usually undertaken
- CT Scan - a CT Scan is a very useful investigation to look at the 3-D bony anatomy of the SCJ. However, in a lot of cases of instability the joint is reduced, and so, the scan may not detect any obvious problem
- MRI Scan - an MRI scan is the best investigation to assess SCJ instability. As well as being able to look at the bones it is also able to show any damage to the soft-tissue ligamentous structures and the intra-articular disk
Management of Anterior SCJ Dislocations / Instability
The management of an Anterior SCJ Dislocation can differ depending on whether there has been an Acute First-Time injury or whether it is a Recurrent problem.
Acute/First-Time Anterior SCJ Dislocation
- Following an Acute SCJ Dislocation the most important initial assessment is whether the joint is still dislocated or has spontaneously reduced. This is best assessed either with a CT Scan or a Digital Tomogram
- Whilst there is one ‘school of thought’ that if the SCJ has been dislocated for more than 48hrs to leave it dislocated. This is something that I, personally, do not adhere to
- My recommendation is to anatomically reduce the joint, no matter how long it has been dislocated for
- The ‘natural history’, following a first-time Anterior SCJ Dislocation, is that there is a 50% chance that the SCJ will dislocate again and a 75% chance that the joint will become unstable
- Having taken this into account, I have developed a Day-Case stabilisation procedure for suitable patients, following a first-time Anterior SCJ Dislocation
- We have recently published a study looking at the outcome of 7 patients who underwent this procedure and, at a minimum of 2 years, none of them had had a further episode of stability
Surgery for a dislocated / first-time Anterior SCJ Dislocation
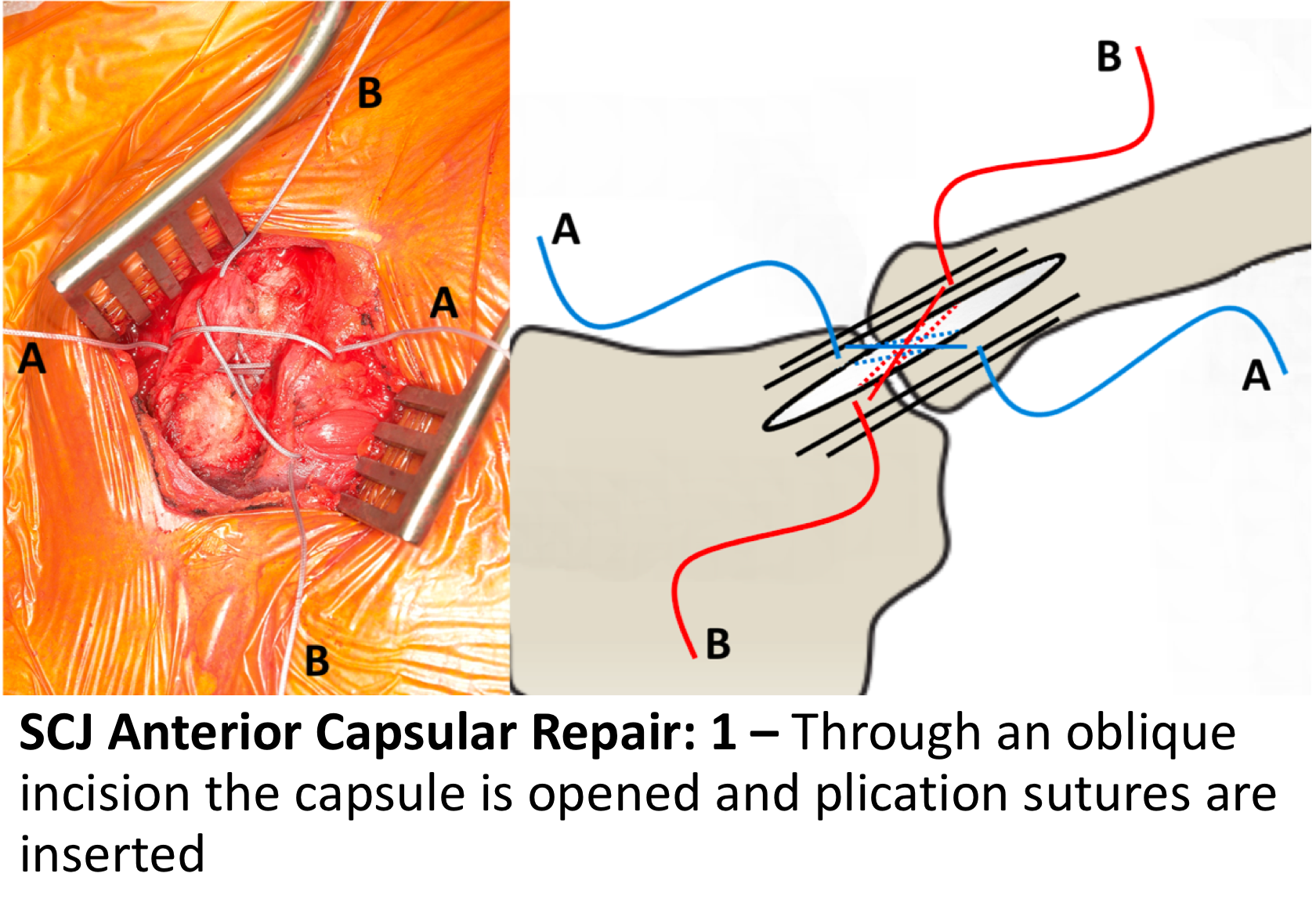
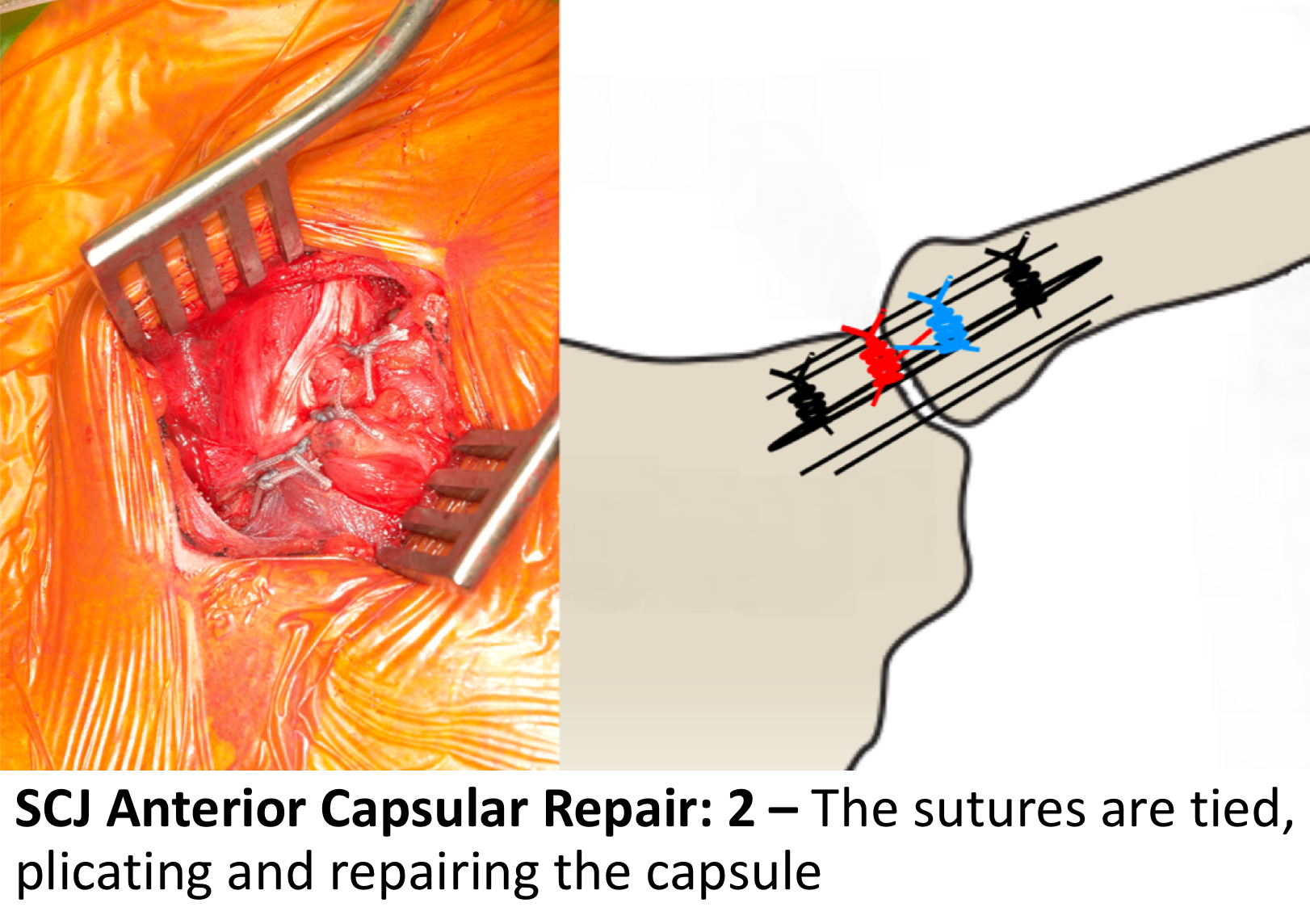
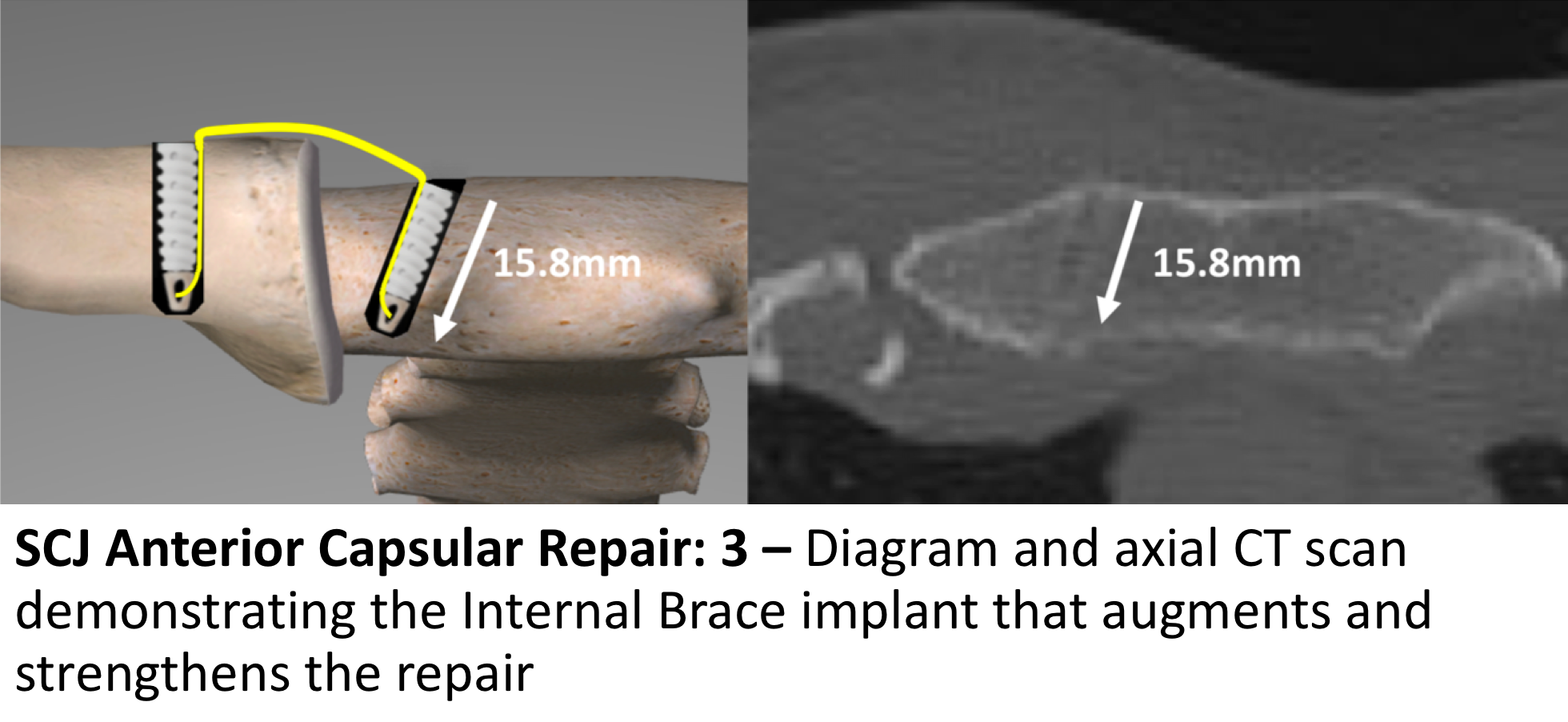
For suitable patients that have sustained a single Anterior SCJ Dislocation, confirmed by suitable imaging, an Open Anterior SCJ Capsular Repair augmented by Internal Bracing is an attractive option. The reason that this can be undertaken is that, following a single SCJ dislocation, the damaged soft-tissue capsular structures are still healthy and can be repaired. After multiple dislocations the capsular tissue is increasingly damaged beyond repair. The procedure is undertaken under a General Anaesthetic and can usually be done as a Day Case.
Using a small, oblique incision over the SCJ, the joint is reduced and the torn anterior sternoclavicular ligament is repaired and tightened using sutures. The repair is then protected using an Internal Brace which consists of 2 suture anchors being inserted into the clavicle and sternum, respectively. Between them a very strong Fibre Tape brace is secured, protecting the soft-tissue repair.
My routine Anterior SCJ Capsular Repair is described below,
- The patient is anaesthetised with a general anaesthetic and prophylactic antibiotics are given
- A 5 – 6cm incision is made over the SCJ and the damaged Anterior SCJ Ligament is opened up
- If the clavicle is dislocated, it is then reduced whilst assessing the intra-articular disk for damage
- The capsule is then repaired using a plicating suture configuration of 4 sutures
- The lateral edge of the sternum and medial end of the clavicle are then exposed
- Using an Internal Brace system, BiocompositeSwivelok Anchors are then inserted into each bone with a double FibreTape tightened between them
- The repair is then inspected, washed out and the wound closed in layers
- Local Anaesthetic is then infiltrated around the wound
After the Surgery
Post-Operative Care
Following an Anterior SCJ Capsular Repair the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
I would usually review patients in the clinic 1 month, and undertake a check CT scan, and then at 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, the SCJ is numb from the local anaesthetic. The SCJ may be painful once the local anaesthetic has worn off which is usually adequately controlled with routine oral analgesics which will be prescribed. I encourage patients to get their arm moving as quickly as possible, discomfort permitting.
After an Anterior SCJ Capsular Repair, it is initially important to ‘protect’ the repair from any significant load, and patients should restrict their arm movements to below shoulder height. Patients would usually need to have their arm in a broad-arm sling for 2 weeks and use their arm when in a safe environment.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
|
Day 1-3 Weeks |
|
| 3-6 Weeks |
|
|
Milestones |
|
|
Week 3 |
Full passive range of movement |
|
Week 6 |
Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated Overhead Activities |
|
| Lifting |
|
| Work |
|
Success of Surgery, Risks & Complications
An Anterior SCJ Capsular Repair is usually a very successful procedure but, because it takes some time for the tissues around the SCJ to recover, it usually takes between 3 – 6 months for the SCJ to be as good as it can be.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during Open SCJ Surgery is rare, but can be catastrophic < 2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
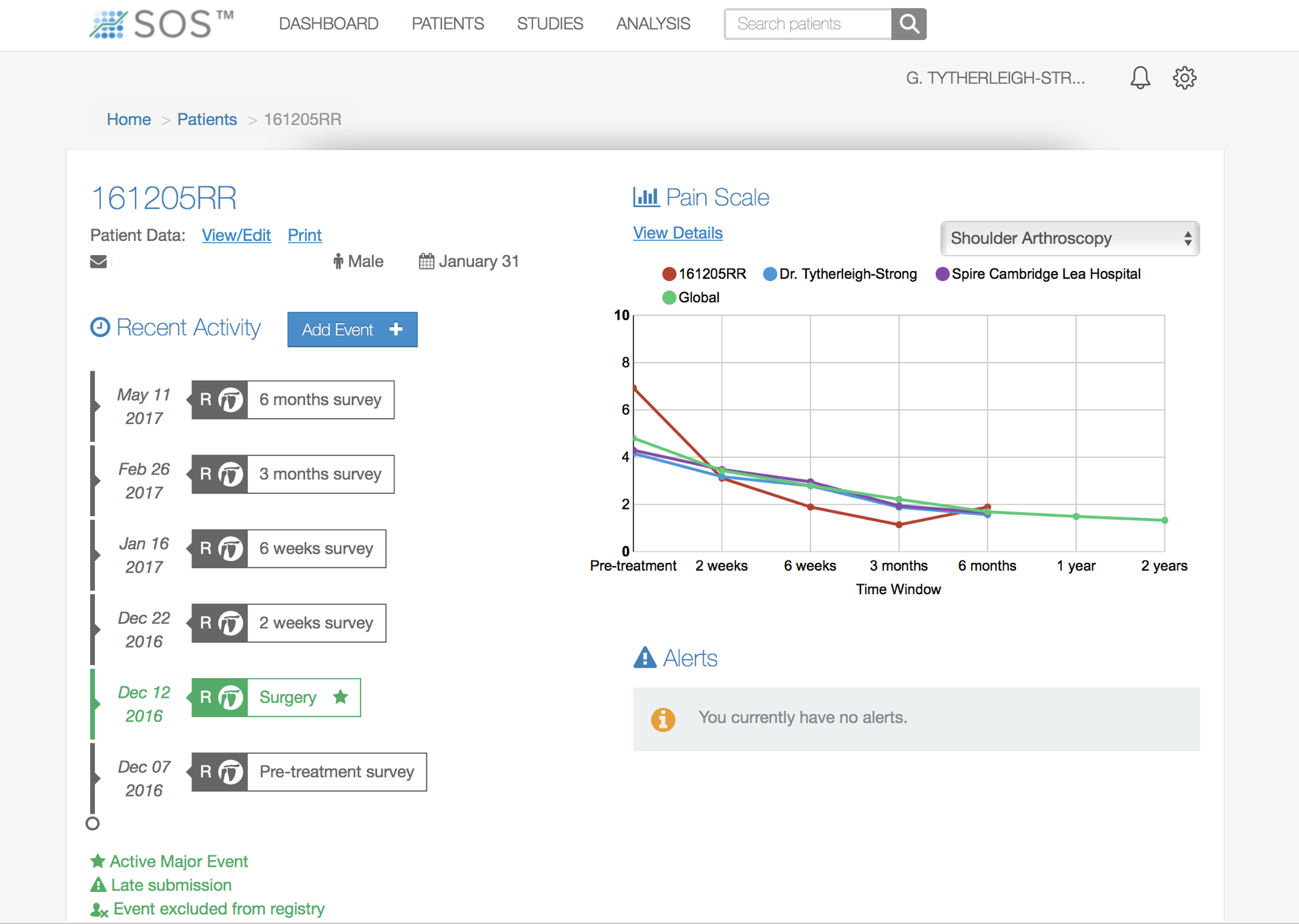
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
find out more about the SOS outcome system…
Recurrent/Chronic Anterior SCJ Dislocation.
- Once someone has developed Recurrent Anterior SCJ Instability, the only treatment that will prevent this happening, is to undertake a surgical reconstruction
- Following repeated dislocations the Anterior SCJ ligament becomes so damaged that it cannot be repaired
- For that reason, a Reconstruction Procedure using a Graft or Synthetic ligament is required to successfully stabilise the joint
Surgery for Recurrent Anterior SCJ Instability
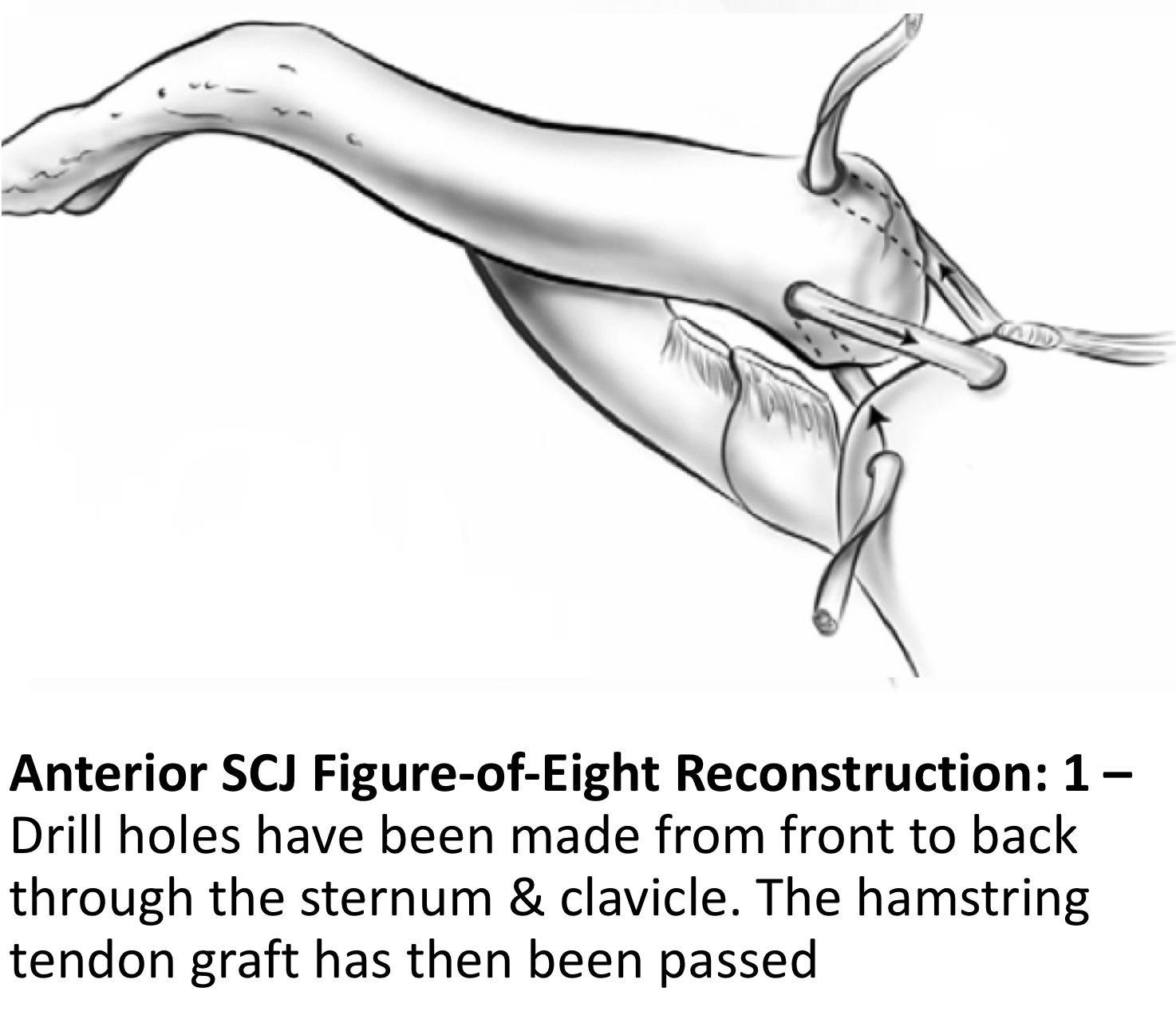
For suitable patients that have Recurrent Anterior SCJ Dislocations, confirmed by suitable imaging, an Anterior SCJ Reconstruction using a Figure-of-Eight Hamstring Tendon Autograft is my procedure of choice. The procedure is undertaken under a General Anaesthetic and usually requires an overnight stay.
Using an oblique incision over the SCJ the medial end of the clavicle and the lateral side of the sternum are exposed. Whilst protecting the retrosternal structures two, 3.5mm drill holes are made through each bone from front-to-back. The Gracilis hamstring tendon is then harvested from the patients knee and prepared. The tendon is then passed through the drill holes in the bones in a figure-of-eight fashion, tightened and sutured into position. The repair is then protected with an Internal Brace. In certain situations, where a patient has previously had a hamstring tendon graft for another procedure or where there might be concerns with regards to the suitability of the patient’s own tendons, a donor allograft hamstring tendon may be used.
My routine Anterior SCJ Reconstruction is described below,
- The patient is anaesthetised with a general anaesthetic and prophylactic antibiotics are given
- A 10 cm incision is made over the SCJ and the damaged and the medial end of the clavicle and lateral end of the sternum exposed
- Dissection is taken posteriorly, protecting the retrosternal structures
- Guide wires are carefully drilled through the bones from front-to-back and then overdrilled with a 3.5cm drill to create 2 drill holes in each bone
- Through a 5cm incision, just below the knee, the Gracilis hamstring tendon is harvested and prepared with a full length FibreWire whip stitch
- The prepared tendon is then passed between the drill holes in the clavicle and sternum in a figure-of-eight fashion
- The tendon is then tightened and its ends securely sutured in position
- Using an Internal Brace system, BiocompositeSwivelok Anchors are then inserted into each bone with a double FibreTape tightened between them
- The repair is then inspected, washed out and the wound closed in layers
- Local Anaesthetic is then infiltrated around the wound
After the Surgery
Post-Operative Care
Following an Anterior SCJ Reconstruction the patient will usually stay in the hospital overnight.Either a CT Scan or Digital Tomogram will be taken the next morning to assess the repair. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, the SCJ is numb from the local anaesthetic. The SCJ may be painful once the local anaesthetic has worn off which is usually adequately controlled with routine oral analgesics which will be prescribed. I encourage patients to get their arm moving as quickly as possible, discomfort permitting.
After an Anterior SCJ Reconstruction, it is initially important to ‘protect’ the repair from any significant load, and patients should restrict their arm movements to below shoulder height. Patients would usually need to have their arm in a broad-arm sling for 4 weeks and use their arm when in a safe environment.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
|
Day 1-4 Weeks |
|
| 4-8 Weeks |
|
|
Milestones |
|
|
Week 4 |
Full passive range of movement |
|
Week 8 |
Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated Overhead Activities |
|
| Lifting |
|
| Work |
|
Success of Surgery, Risks & Complications
An Anterior SCJ Reconstruction is usually a very successful procedure but, because it takes some time for the reconstructed tissues around the SCJ to recover, it usually takes between 6 months for the SCJ to be as good as it can be.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during open Anterior SCJ surgery is rare, but can be catastrophic < 1%
CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
find out more about the SOS outcome system…