Shoulder Arthritis (Osteo-Arthritis)
Shoulder Osteo-Arthritis – What is it?
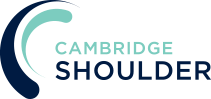
- Osteo-arthritis is a progressive ‘wear and tear’/degenerative process of the shoulder joint
- Normal, healthy articular cartilage allows smooth movement between joint surfaces and is particularly good at dissipating load
- As part of the degenerative process the specialised ‘articular’ cartilage, that covers both sides of the shoulder joint, is progressively thinned and ultimately wears away
- As this occurs joint movement becomes more difficult resulting in stiffness and pain
- Over time the adjacent bones remodel as the joint becomes more abnormal
- Shoulder osteoarthritis is less common than arthritis of the hips and knees but it can be a very debilitating problem and have a significant impact on a patient’s quality of life
Why does it happen & Who gets it?
- Fundamentally Osteoarthritis is due to wear and tear of the joint
- However, there are a number of contributing factors that can make people more susceptible and include,
- Previous fractures to the shoulder
- Previous dislocation to the shoulder
- Overuse of the shoulder
- Inflammatory arthritis (mainly Rheumatoid arthritis)
- Genetic predisposition to osteoarthritis
- Individuals particularly at risk are heavy manual workers, weight-lifters and individuals involved in high energy overhead activities
What are the symptoms of Shoulder Arthritis?
- The main symptoms of Shoulder Arthritis are pain and stiffness with a restriction of movement
- The pain tends to get worse through the day and with activity
- Patients often describe an intermittent catching sensation and a ‘creaking’ noise as they move the shoulder
Could it be something else?
There are a few of other common conditions that affect the shoulder that can present with similar symptoms to Shoulder Arthritis
- Frozen Shoulder – a Frozen shoulder can present with severe pain and restriction of movement. Symptoms tend to progress more quickly than with shoulder arthritis and the restriction of movement tends to be in every direction
find out more about Frozen Shoulder ….
- Massive Rotator Cuff Tear – a massive rotator cuff tear can present with pain and a restriction of movement. In certain circumstances a massive rotator cuff tear can lead to a special type of shoulder arthritis known as a Rotator Cuff Arthropathy
find out more about massive rotator cuff tears ….
How do you diagnose Shoulder Arthritis?
To diagnose and treat Shoulder Arthritis, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. Rotator Cuff and ACJ osteoarthritis are also common shoulder problems and it is not unusual for patients with Shoulder Arthritis to also have an element of these conditions contributing to their symptoms.
History
- Shoulder Arthritis usually develops with a gradual onset and deterioration of symptoms over time, which can often be over months and years
- Occasionally symptoms can develop rapidly, particularly when precipitated by a minor incident or injury
- Initially pain and stiffness develop around the joint after activity. As things progress a constant background ache may be present with increasingly severe pain on certain movements, particularly when the shoulder is suddenly jarred
- The shoulder is often painful at night and when lying on it
- Shoulder movement begins to decrease, particularly external rotation and elevation, which may be accompanied by a ‘creaking’ or ‘grinding’ sensation
Examination
- Usually there is no visible swelling or inflammation associated with Shoulder Arthritis
- Sometimes there is pain on deep palpation of the front and back joint line
- Restriction of certain movements, when compared to the normal shoulder, are usually present. External and Internal Rotation and forward elevation are most commonly affected.
- There is usually a definite mechanical block at the end of movement although the patient usually has normal power
- ‘crepitus’, a crunching / grinding sensation may be felt over the joint as it is moved
- it is not uncommon for patients with Shoulder Arthritis to also have an element of concomitant Rotator Cuff disease and so it is also important to assess Rotator Cuff function.
find out more about examination of the Shoulder ….find out more about Rotator Cuff disease ….
Investigations
- X-Ray – an adequate plain x-ray of the shoulder including an AP and axillary view are usually sufficient to diagnose Shoulder Arthritis. The characteristic findings
- narrowing of the joint space between the Humeral Head and Glenoid
- sclerosis, thickening of the bone at the joint surfaces, this is represented by increased whiteness on the x-ray
- osteophytes, these are extra bits of bone that form at the edges of the joint
- cysts, these are small fluid filled cavities that form around the joint surfaces and are represented by small, dark, spherical spots on the x-ray
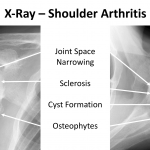
- CT Scan – a CT Scan can demonstrate the bones of the shoulder in 3-D view. This can be useful if there are marked bony changes around the shoulder and if there are concerns with regards to bone loss. A CT Scan can be very useful when planning for a Shoulder Replacement
find out more about CT Scans of the shoulder …. - USS & MRI Scan – Shoulder Arthritis only affects the bones but if there are any concerns that there might be any associated Rotator Cuff problems an USS or MRI scan may be required.
Treatment of Shoulder Arthritis
Treatment of Shoulder Arthritis(Fig 1)
As a general rule, treatment for Shoulder Arthritis is based on the level of symptoms that a patient is currently experiencing rather than the severity of the arthritis that can be seen on the x-ray.
It is impossible to predict whether a patient’s symptoms will actually continue to deteriorate, regardless of the severity of their x-ray. As a result, there is usually no indication to ’prophylactically’ undertake a joint replacement based solely on the severity of the arthritis on their x-ray rather than their symptoms.
Analgesia/Pain Relief
- pain is the major problem associated with a Shoulder Arthritis
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
- Nociceptive Analgesics –
- Nociceptive pain killers work on nerve generated pain
- Amitriptyline in lower doses works as a nociceptive pain killer. It has a useful side-effect in that it can make patients drowsy
- in cases of severe pain Amitriptyline can be prescribed at night
Physiotherapy
- Physiotherapy can be very useful in helping to maintain shoulder movement and to re-strengthen surrounding muscles
- Physiotherapy can also help with stiffness and prevent further loss of movement
Find out more about Physiotherapy for Shoulder Arthritis….
Cortisone Injection
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the Shoulder &Subacromialspace it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- a Cortisone injection can be very helpful with regards to pain associated with Shoulder Arthritis
- it can usually be injected simply in the Out-Patient Clinic
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Treatment of Shoulder Arthritis
Treatment of Shoulder Arthritis
As a general rule, treatment for Shoulder Arthritis is based on the level of symptoms that a patient is currently experiencing rather than the severity of the arthritis that can be seen on the x-ray.
It is impossible to predict whether a patient’s symptoms will actually continue to deteriorate, regardless of the severity of their x-ray. As a result, there is usually no indication to ’prophylactically’ undertake a joint replacement based solely on the severity of the arthritis on their x-ray rather than their symptoms.
Analgesia/Pain Relief
- pain is the major problem associated with a Shoulder Arthritis
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
- Nociceptive Analgesics –
- Nociceptive pain killers work on nerve generated pain
- Amitriptyline in lower doses works as a nociceptive pain killer. It has a useful side-effect in that it can make patients drowsy
- in cases of severe pain Amitriptyline can be prescribed at night
Physiotherapy
- Physiotherapy can be very useful in helping to maintain shoulder movement and to re-strengthen surrounding muscles
- Physiotherapy can also help with stiffness and prevent further loss of movement
Find out more about Physiotherapy for Shoulder Arthritis….
Cortisone Injection
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the Shoulder & Subacromial space it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- a Cortisone injection can be very helpful with regards to pain associated with Shoulder Arthritis
- it can usually be injected simply in the Out-Patient Clinic
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Hyaluronic Acid
- Hyaluronic Acid is similar to a substance that occurs naturally in joint synovial fluid and has lubricating and shock absorbing properties
- Injecting Hyaluronic Acid into an osteoarthritic joint can help relieve pain by its viscosupplementaion properties
- However, multiple studies have not shown that the pain relief obtained from Hyaluronic Acid injections is any better or lasts any longer than taking a course of NSAIDs
- The potential advantage of Hyaluronic Acid is that it does not have the side-effects of NSAIDs, but needs to be administered as an injection
Keyhole Surgery
Surgery for Shoulder Arthritis
- Shoulder Arthritis is a ‘wear and tear’ condition. The future of treating this condition is going to be either preventing it before it starts or catching it at its earliest stages, probably through Stem Cell treatment and regenerating the articular cartilage. Whilst currently there are some treatment options to help to repair and regenerate articular cartilage they are only applicable in a few situations, usually at the very earliest stages of degeneration or for an isolated small part of articular cartilage damage.
- In practice, by the time most shoulder arthritis symptoms actually appear, the ‘wear and tear’ has already advanced past the stage where any of our current regenerative treatments can help.
- As a result, surgery for shoulder arthritis is aimed at either cleaning up, smoothing the joint surfaces, removing loose fragments and releasing soft tissue contractures or undertaking a shoulder replacement. Currently it is not possible to ‘turn back time’ and convert an arthritic shoulder into a healthy 20-year old shoulder!
- The other significant factor to consider with Shoulder Arthritis is that all of the soft-tissue structures around the shoulder, and particularly the Rotator Cuff tendons, are also undergoing degenerative change at the same time. As a result, it is not uncommon for patients with Shoulder Arthritis to also have Rotator Cuff problems. It is often important to also take any Rotator Cuff problems into consideration to successfully treat Shoulder Arthritis.
Arthroscopic Surgery (Keyhole) for Shoulder Arthritis
- Arthroscopic Surgery for Shoulder Arthritis is primarily a temporary measure to ‘tidy-up’ the joint removing any loose or damaged fragments, smoothing off the joint, releasing any soft-tissue contractures and addressing any associated Rotator Cuff problems.
- The advantage of Arthroscopic Surgery is that it can usually be done as a Day Case procedure without requiring any post-operative immobilisation and there is usually a swift recovery.
- Arthroscopic Surgery does not have any effect on the actual ‘wear and tear’ that is present. As a result, its main benefits are likely to be with pain relief and less so with regards to an improvement in range of motion.
- Arthroscopic Shoulder Surgery is a minimal surgical procedure and will not have any detrimental effect if a subsequent Shoulder Replacement is undertaken
- Occasionally, patients with advanced arthritis, who do not want a joint replacement or who are not medically well enough to undergo a shoulder replacement can gain good pain relief from arthroscopic surgery.
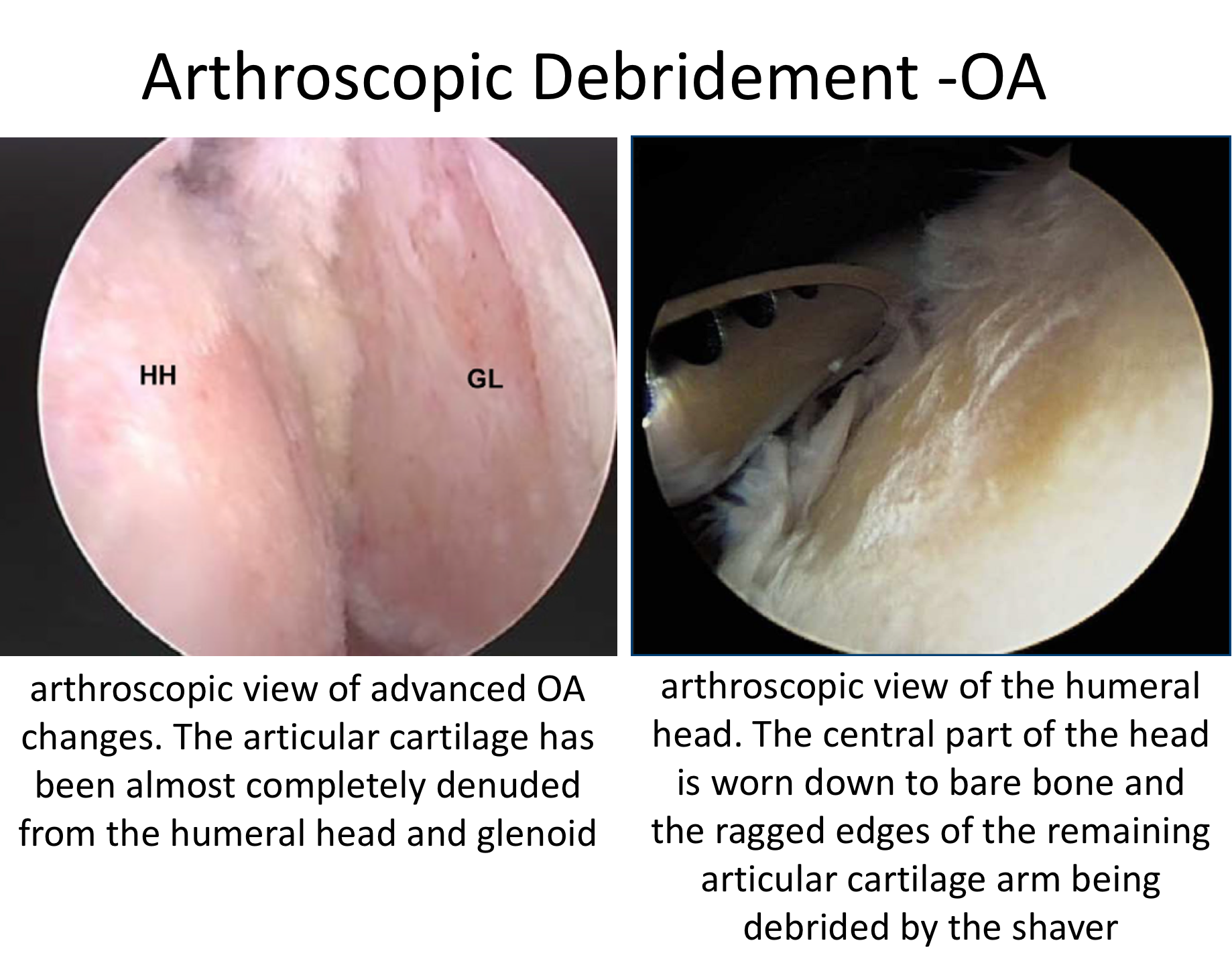
Arthroscopic Debridement of the Shoulder
The best operation for someone with early Shoulder Arthritis, that is refractory to treatment, is an Arthroscopic Debridement of the Shoulder. This is an operation where an Arthroscopic camera is positioned inside the Shoulder Joint and, by using specialized instruments, loose fragments are removed, the joint surface can be smoothed off and any soft-tissue contractures can be released. Some patients with Shoulder Arthritis have associated Rotator Cuff problems in the form of Supraspinatus Tendonitis and Long Head of Biceps Tendonitis. In this situation, it is also possible to address these problems with Arthroscopic Subacromial Decompression and Biceps Tenotomy, at the same time.
find out more about an Arthroscopic Subacromial Decompression ….
An Arthroscopic Debridement of the Shoulder can usually be done as a Day Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to remove any loose fragments, smooth off the joint surface and release any contractures.
After the surgery, it is important to get the shoulder moving as quickly as possible to try and regain and maintain as much mobility as possible. It usually takes between 6 – 12 months to gain the best benefits of the procedure with regards to pain relief and movement. The exact extent of the pain relief and improvement in movement for any individual patient is very difficult to predict but almost all patients gain some benefit that can last over 2 years. My routine Arthroscopic Debridement of the Shoulder Procedure is described below,
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
- A posterior, an anterior portal and a single lateral portal are used for to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- The Glenohumeral Joint is initially assessed for the extent of the arthritis, loose fragments present and any contractures. Any other associated with the Rotator Cuff and the Long Head of Biceps are also identified
- All of the loose bone fragments are then removed using a combination of a grasper and a shaver
- Any loose flaps of articular cartilage and excess bone are then removed from the humeral head and glenoid
- Any significant contractures in the joint capsule are then released and a Long Head of Biceps Tenotomy performed, if indicated
- The Subacromial Space is then entered and the undersurface of the Acromion identified.
- A lateral portal is then created
- Using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the Subacromial Spur.
- A powered burr is then used to resect about 5mm of bone from the undersurface of the acromion
- The GlenoHumeral Joint and Subacromial Space are then washed out and the wounds closed with sub-cuticular sutures
Video – Arthroscopic Shoulder Debridement
find out more about having an operation…
After the Surgery
Post-Operative Care
Following an Arthroscopic Debridement of the Shoulder the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after a Debridement….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves out of using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Optimum passive range of movement |
| Week 6 | Optimum active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic Debridement of the Shoulder for Arthritis is usually a very safe procedure. However, the exact benefit with regards to pain relief and range of movement obtained but any patient is very unpredictable. Some patients get an almost complete resolution of their symptoms and others gain less benefit. Some patients gain a sustained benefit for over 2 years and others less so. Arthroscopic Shoulder Surgery is a minimal surgical procedure and will not have any detrimental effect if a subsequent Shoulder Replacement is required.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
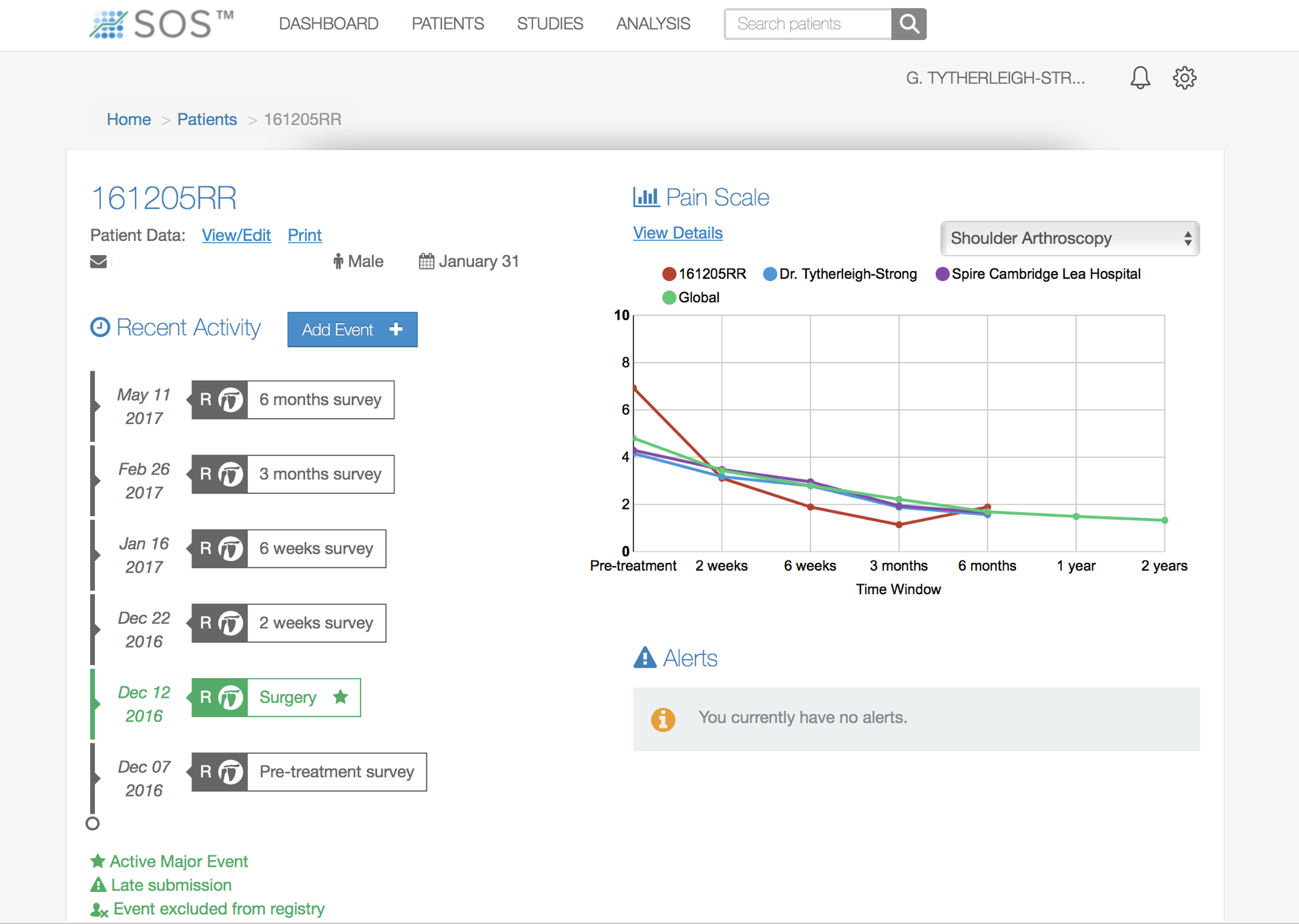
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system ….
CAM Procedure (Complete Arthroscopic Management)
Although a Shoulder Replacement is an extremely good operation with regards to pain relief and function but it is NOT particularly robust. Undertaking any repetitive medium or heavy manual work, such as hammering, pounding and lifting heavy weight, can significantly affect a Shoulder Replacement leading to earlier wear, loosening and resulting in failure.
Sometimes significant shoulder osteoarthritis can occur in patients who are relatively young and are working in a physical or manual job. For these patients, undergoing a Shoulder Replacement will effectively mean changing or modifying their type of work. Whilst for some people this is possible for others, particularly in the current economic climate, that is easier said than done.
The Complete Arthroscopic Management (CAM) Procedure is designed to try and remove as much bony osteophyte (excess bone) as possible, to release all of the soft-tissues, to decompress the axillary nerve and address any concomitant rotator cuff problems, including long head of biceps tendonitis. Its aim is to try and regain as much function as possible and to relieve pain. It tends to be indicated for younger patients and is reported to have good results for at least 2 years. It is important to remember that it is considered to be a temporising procedure and not usually the definitive treatment for symptomatic osteoarthritis.
A CAM Procedure can usually be done as a Day Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to remove any loose fragments, remove as much of the osteophytes as possible, to smooth off the joint surface, release any contractures, to decompress the axillary nerve and address any associated rotator cuff problems.
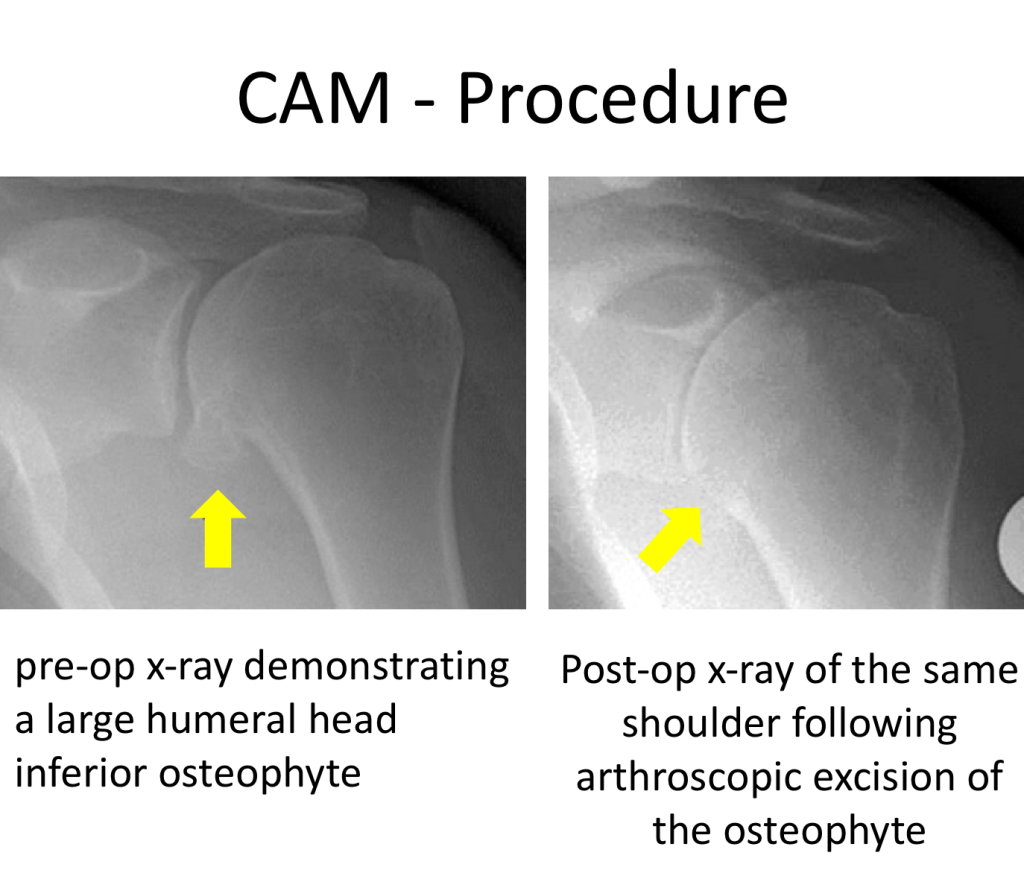
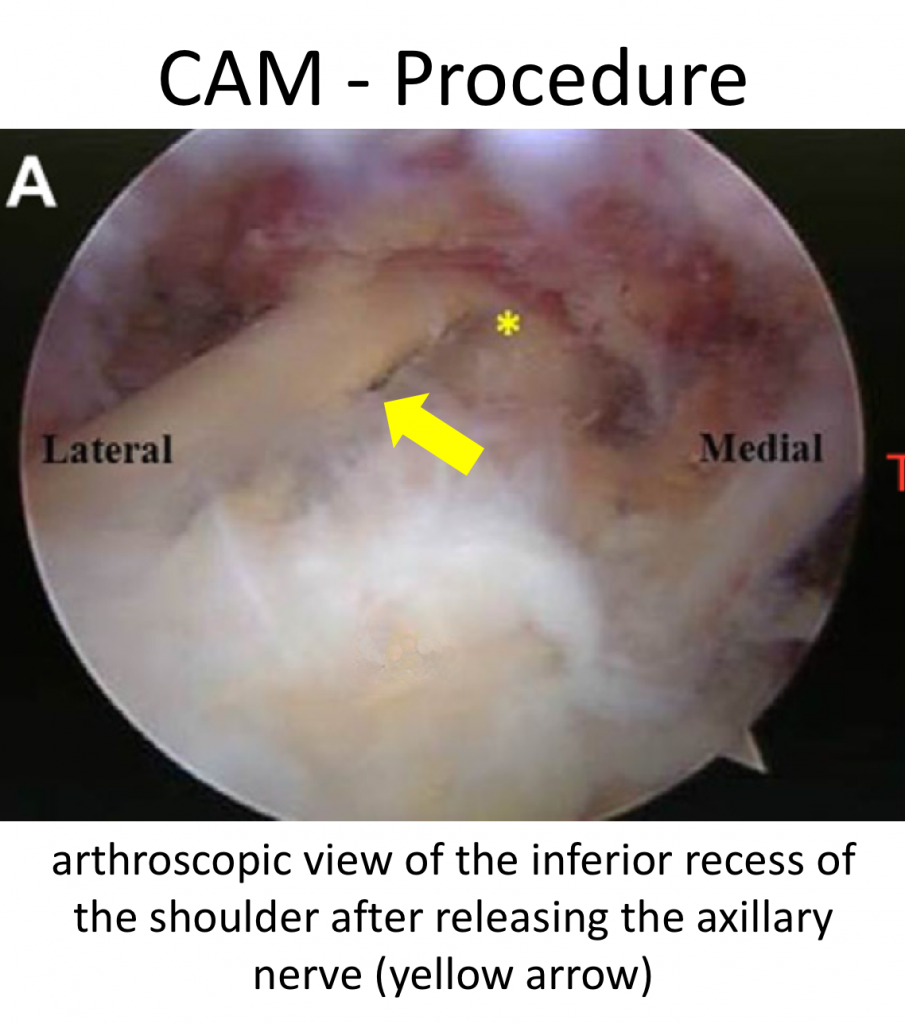
Fig 5 & 6
After the surgery, it is important to get the shoulder moving as quickly as possible to try and regain and maintain as much mobility as possible. It usually takes between 3 – 6 months to gain the best benefits of the procedure with regards to pain relief and movement. The exact extent of the pain relief and improvement in movement for any individual patient is very difficult to predict but almost all patients gain some benefit that can last over 2 years. My routine CAM Procedure is described below,
Watch a video of a CAM Procedure….
Find out more about Arthroscopic Surgery….
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Inter scalene Nerve Block….
- A posterior, low posterior, an anterior portal and a single lateral portal are used for to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- The Glenohumeral Joint is initially assessed for the extent of the arthritis, loose fragments present and any contractures. Any other associated problems with the Rotator Cuff and the Long Head of Biceps are also identified
- All of the loose bone fragments are then removed using a combination of a grasper and a shaver
- Any loose flaps of articular cartilage and excess bone are then removed from the humeral head
- Vieiwing from the posterior portal the large inferior osteophyte, which is always present at the base of the humeral head, is resected using a combination of a shaver and burr introduced through the low inferior portal
- Any other significant circumferential osteophytes are also removed from around the edge of the humeral head
- Again, viewing from the posterior portal, the inferior capsule is carefully released exposing and decompressing the axillary nerve
- Any significant contractures around the rest of the joint capsule are then released and
- A Long Head of Biceps Tenotomy or Tenodesis is also undertaken, if indicated
- The Subacromial Space is then entered and the undersurface of the Acromion identified.
- A lateral portal is then created
- Using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the Subacromial Spur.
- A powered burr is then used to resect about 5mm of bone from the undersurface of the acromion
- The GlenoHumeral Joint and Subacromial Space are then washed out and the wounds closed with sub-cuticular sutures
find out more about having an operation….
After the Surgery
Post-Operative Care
Following a CAM Procedure the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after a CAM Procedure….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves out of using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Optimum passive range of movement |
| Week 6 | Optimum active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
A CAM Procedure for Arthritis is usually a very safe procedure. However, the exact benefit with regards to pain relief and range of movement obtained but any patient is very unpredictable. Some patients get an almost complete resolution of their symptoms and others gain less benefit. Most patients gain a sustained benefit for over 2 years and others less so. Arthroscopic Shoulder Surgery is a minimal surgical procedure and will not have any detrimental effect if a subsequent Shoulder Replacement is required.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Success of Surgery, Risks & Complications
An Arthroscopic Debridement of the Shoulder for Arthritis is usually a very safe procedure. However, the exact benefit with regards to pain relief and range of movement obtained but any patient is very unpredictable. Some patients get an almost complete resolution of their symptoms and others gain less benefit. Some patients gain a sustained benefit for over 2 years and others less so. Arthroscopic Shoulder Surgery is a minimal surgical procedure and will not have any detrimental effect if a subsequent Shoulder Replacement is required.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
CAM Procedure (Complete Arthroscopic Management)
Although a Shoulder Replacement is an extremely good operation with regards to pain relief and function but it is NOT particularly robust. Undertaking any repetitive medium or heavy manual work, such as hammering, pounding and lifting heavy weight, can significantly affect a Shoulder Replacement leading to earlier wear, loosening and resulting in failure.
Sometimes significant shoulder osteoarthritis can occur in patients who are relatively young and are working in a physical or manual job. For these patients, undergoing a Shoulder Replacement will effectively mean changing or modifying their type of work. Whilst for some people this is possible for others, particularly in the current economic climate, that is easier said than done.
The Complete Arthroscopic Management (CAM) Procedure is designed to try and remove as much bony osteophyte (excess bone) as possible, to release all of the soft-tissues, to decompress the axillary nerve and address any concomitant rotator cuff problems, including long head of biceps tendonitis. Its aim is to try and regain as much function as possible and to relieve pain. It tends to be indicated for younger patients and is reported to have good results for at least 2 years. It is important to remember that it is considered to be a temporising procedure and not usually the definitive treatment for symptomatic osteoarthritis.
A CAM Procedure can usually be done as a Day Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to remove any loose fragments, remove as much of the osteophytes as possible, to smooth off the joint surface, release any contractures, to decompress the axillary nerve and address any associated rotator cuff problems. After the surgery, it is important to get the shoulder moving as quickly as possible to try and regain and maintain as much mobility as possible. It usually takes between 3 – 6 months to gain the best benefits of the procedure with regards to pain relief and movement. The exact extent of the pain relief and improvement in movement for any individual patient is very difficult to predict but almost all patients gain some benefit that can last over 2 years. My routine CAM Procedure is described below
Watch a video of a CAM Procedure….
Find out more about Arthroscopic Surgery….
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Inter scalene Nerve Block….
- A posterior, low posterior, an anterior portal and a single lateral portal are used for to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- The Glenohumeral Joint is initially assessed for the extent of the arthritis, loose fragments present and any contractures. Any other associated problems with the Rotator Cuff and the Long Head of Biceps are also identified
- All of the loose bone fragments are then removed using a combination of a grasper and a shaver
- Any loose flaps of articular cartilage and excess bone are then removed from the humeral head
- Vieiwing from the posterior portal the large inferior osteophyte, which is always present at the base of the humeral head, is resected using a combination of a shaver and burr introduced through the low inferior portal
- Any other significant circumferential osteophytes are also removed from around the edge of the humeral head
- Again, viewing from the posterior portal, the inferior capsule is carefully released exposing and decompressing the axillary nerve
- Any significant contractures around the rest of the joint capsule are then released and
- A Long Head of Biceps Tenotomy or Tenodesis is also undertaken, if indicated
- The Subacromial Space is then entered and the undersurface of the Acromion identified.
- A lateral portal is then created
- Using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the Subacromial Spur.
- A powered burr is then used to resect about 5mm of bone from the undersurface of the acromion
- The GlenoHumeral Joint and Subacromial Space are then washed out and the wounds closed with sub-cuticular sutures.
After the Surgery
Post-Operative Care
Following a CAM Procedure the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after a CAM Procedure….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves out of using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Optimum passive range of movement |
| Week 6 | Optimum active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
A CAM Procedure for Arthritis is usually a very safe procedure. However, the exact benefit with regards to pain relief and range of movement obtained but any patient is very unpredictable. Some patients get an almost complete resolution of their symptoms and others gain less benefit. Most patients gain a sustained benefit for over 2 years and others less so. Arthroscopic Shoulder Surgery is a minimal surgical procedure and will not have any detrimental effect if a subsequent Shoulder Replacement is required.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Shoulder Replacement
Shoulder Replacement (Arthroplasty)
- Ultimately in cases of severe arthritis, that cannot be adequately managed by conservative measures or have not been adequately resolved following other treatments, a shoulder replacement (arthroplasty) is indicated. There are a number of variations of shoulder replacements available and the choice of replacement depends on a number of criteria which include: patient age and activity level, the type of arthritis, the amount of bone loss and the surgeon’s preference.
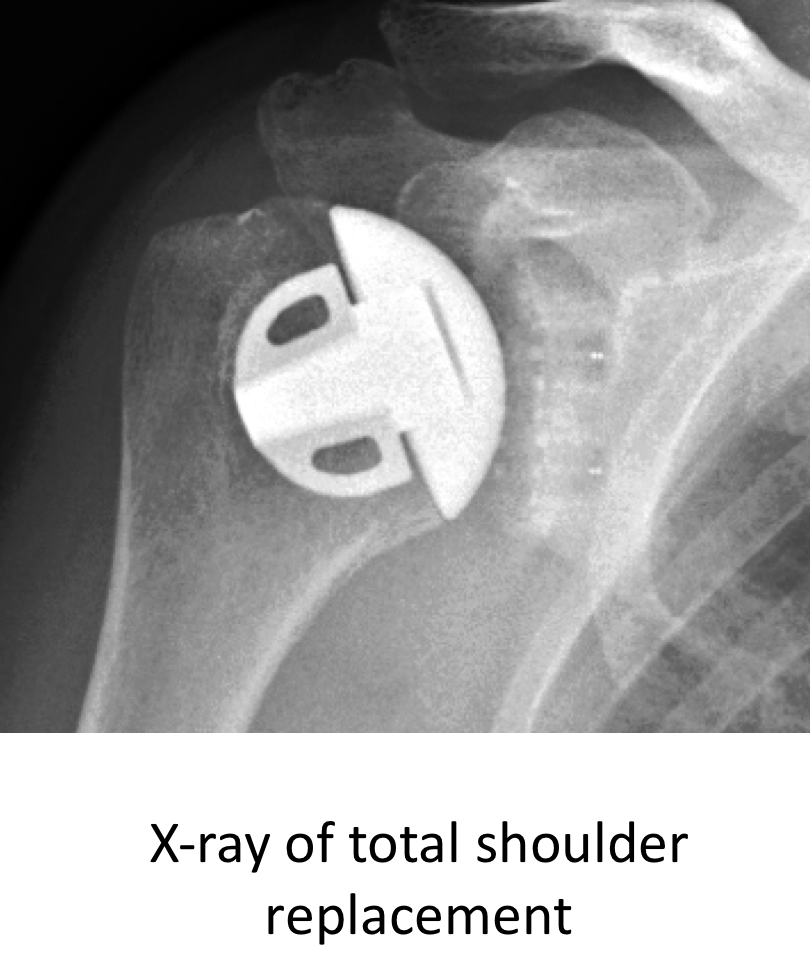
- Traditionally two type of shoulder replacement have been used a hemiarthroplasty and a total shoulder replacement. A hemiarthroplasty involves just replacing the Humeral head, usually with a metal prosthetic implant. And a total shoulder involves replacing both the humeral head and the glenoid socket, usually with a plastic implant.
- Previously it was felt that there wasn’t really much difference with regards to the results of having a hemiarthroplasty or a total shoulder replacement. However, more recent studies have shown that a total shoulder replacement gives better results with regards to pain relief and function. I prefer to undertake a total shoulder replacement wherever possible.
- There are a few situations where a total shoulder replacement is not suitable and a hemiarthroplasty is indicated. These include;
- Young patients, generally under the age of 30, who are having their surgery as the result of trauma or AVN (Avascular Necrosis). In these cases the glenoid side of the joint is relatively well preserved and this, coupled with the fact that the glenoid component of a shoulder replacement is the part that wears, means that a hemiarthroplasty is usually more suitable
- Patients with significant bone loss or deformity of the glenoid part of the shoulder. The bone-stock in a normal glenoid is relatively small, if there is a significant loss of bone or deformity of the glenoid there may not be sufficient bone to firmly implant a glenoid component.
What are the Indications for a Shoulder Replacement?
- The main indication for a shoulder replacement is severe pain that has not responded to other treatment. Joint replacements, in general, are particularly good at relieving pain. Whilst they usually improve function and range of motion, this should not be the primary for undergoing surgery.
What are the Likely Benefits of a Shoulder Replacement?
- Pain relief is the primary benefit of having a shoulder replacement. Most patients should expect their shoulder to be almost or completely pain free following recovery and to rarely require taking any analgesia.
- The shoulder is a complex joint and its function is heavily reliant on a complex arrangement of muscles, ligaments and tendons. Degenerative changes are occurring in everyone’s’ rotator cuff muscles and tendons over time, regardless as to whether they have arthritis or not. This, coupled with the fact that the shoulder has not been moving properly due to the arthritis, means that following a shoulder replacement, although there is a ‘new’ ball and socket, the rest of the shoulder will take time to recover and is not brand new!
- As a result, patients rarely get a complete 100% functional recovery of their shoulder following a shoulder replacement. In reality, most patients regain 75% of their actual shoulder function. However, as the shoulder has such a large functional reserve of movement (we don’t usually have to use our shoulders to the extreme of their movements) most patients are able to regain all of the function that they require for day to day activity
What Implants are Used for a Shoulder Replacement?
An implant is the prosthetic component that is used to replace the joint. Implants are made of various types of inert materials such as metal alloys, high molecular weight polyethylene and ceramic. They are designed and manufactured to an incredibly high standard. The articulating surfaces on the humeral and glenoid sides of a joint replacement are incredibly smooth and are designed to have minimum friction on movement with minimal wear.
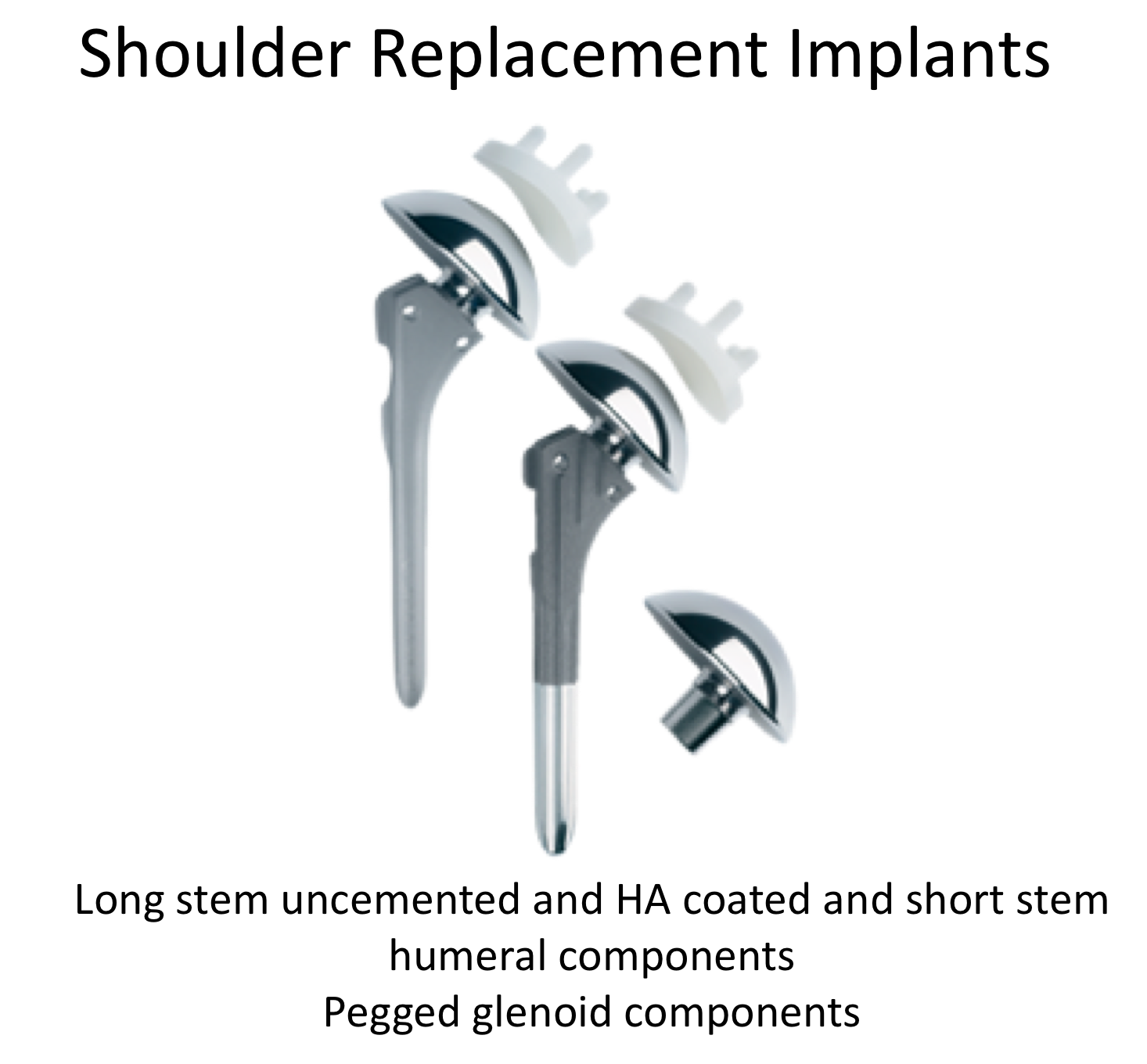
Humeral Component
- Most humeral components are modular. This means that they come in 2 parts. There is usually a stem, which is securely fixed into the bone, and head component which is attached to the stem and articulates with the glenoid
- A modular system allows components of different sizes to be used to more accurately recreate the patient’s anatomy
Stem
- Traditionally the stem has been about 14 cm long and has been implanted down the shaft of the humerus
- More recently short stems have been introduced. These are 3 to 4cm in length and are fixed into the flared top of the humerus. They do not go down into the shaft of the humerus
- The potential advantage of a short stem is that it leaves the option of being able to undertake a stemmed implant replacement if a revision operation is required
- A resurfacing component is a shell like domed, component that is fixed directly onto the remnant of the patient’s humeral head after about 3mm of the articular surface and underlying bone has been removed
- The potential advantage of a resurfacing component is that it removes a minimal amount of the patient’s bone
- However, it does not allow easy access to the glenoid and is often undertaken as a hemiarthroplasty. Also, it has to be made of metal
Humeral Head
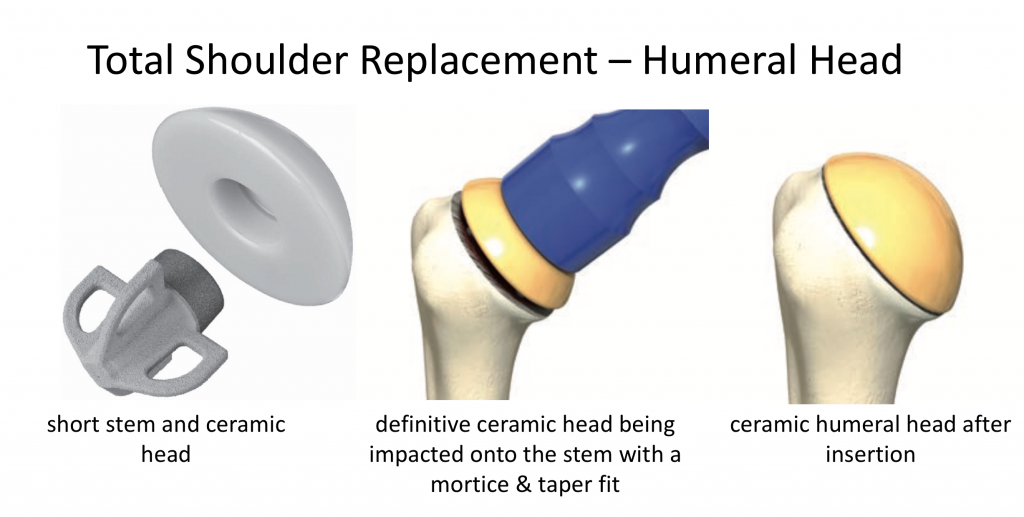
- The humeral head component is attached to the stem using a mortice and taper system
- Humeral heads come in various sizes and can be matched to the size of the patient and the glenoid component that is being used
- Traditionally the humeral head has been made of a metal alloy with a highly polished articulating surface
- Recently ceramic humeral heads have been developed. Ceramic is a very hard material and can be polished to an incredibly high finish
- The potential advantage of a ceramic humeral head is that it hard and has a lower coefficient of friction so that it creates less wear on the glenoid component
Glenoid Component
- The articulating part of the glenoid component is always made of high molecular weight polyethylene. This is a very tough and smooth plastic
- Glenoid components are either all plastic or modular with a metal base that is fixed into the bone with a plastic articulating component that clicks into it
- The advantage of a metal-backed glenoid component is that it can be fixed into the bone directly, without cement
- However, the disadvantage of a metal-backed component is that the plastic articulating insert is necessarily thinner than an all plastic component. This potentially means that it can wear out more quickly
Component Fixation
- All components have to be fixed securely into the patient’s bone
- Traditionally this has been done using methyl methacrylate bone cement. This provides an instant and secure fixation
- However, there are potential issues with bone cement with regards to removing it and wear particle reactions
- Calcium Hydroxyapatite is the main inorganic constituent of bone and can be bonded by a process of sintering onto the metal component of a joint replacement
- The surface of a calcium hydroxyapatite coated joint component allows the patient’s bone to ‘grow’ onto it. This provides a very secure fixation without the need for cement
- The disadvantage of a calcium hydroxyapatite coated component is that it takes some time for the bone to ‘grow’ on to it. As a result the component is not as securely fixed as it is going to be at the time of surgery
- This can have some issues with regards to being immediately able to weight bear following a hip or knee replacement
- However, because the shoulder is not ‘load-bearing’ the initial fixation of a calcium hydroxyapatite coated component is more than sufficient to allow the joint to be moved and used immediately
My Choice of Shoulder Replacement
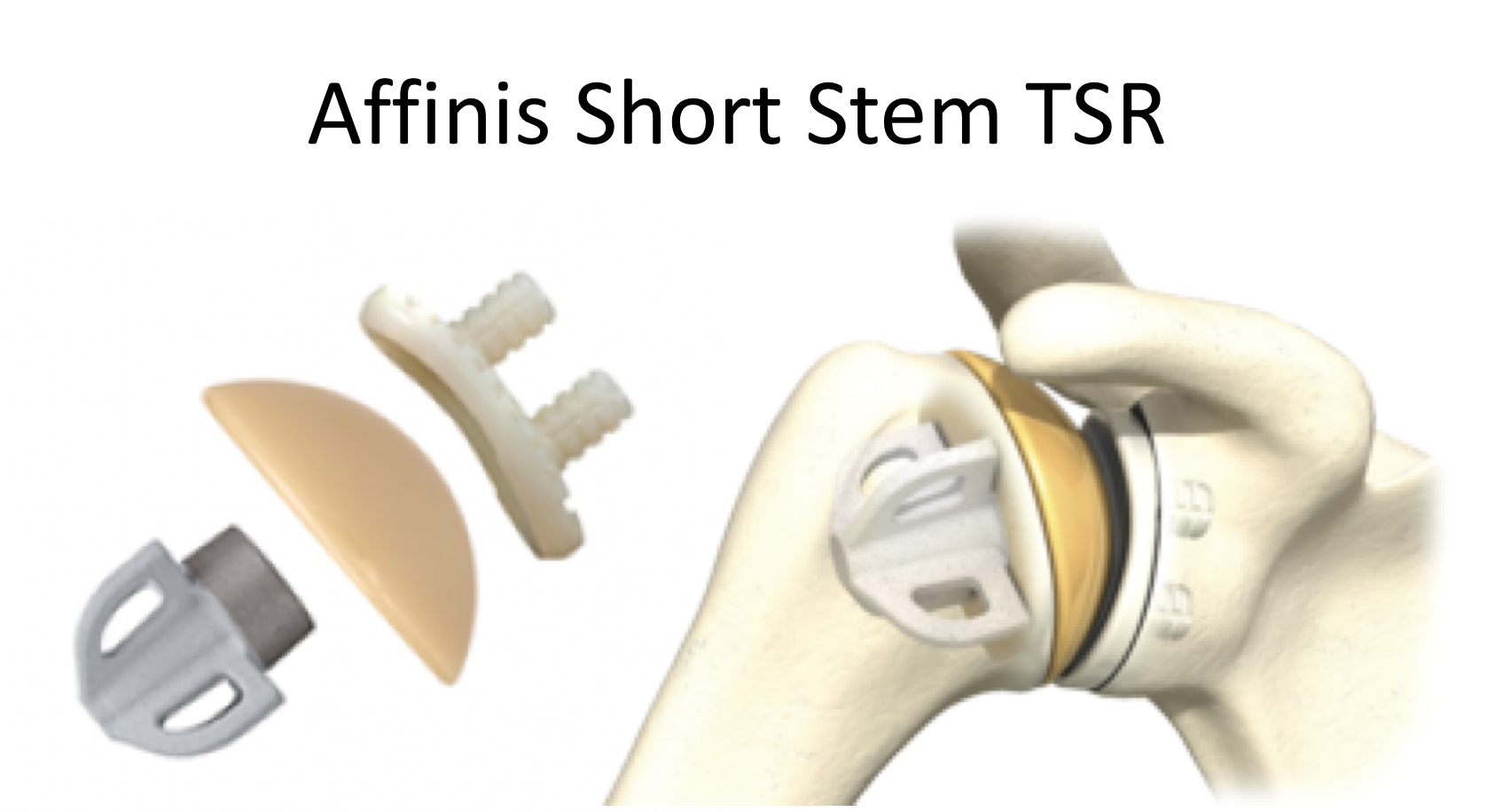
Wherever possible I prefer to undertake a Total Shoulder Replacement. I feel that the results with regards to pain relief, movement and function are better than a Hemiarthroplasty. I use the Affinis modular shoulder replacement system that is made by Mathys, which is a Swiss orthopaedic implant company.
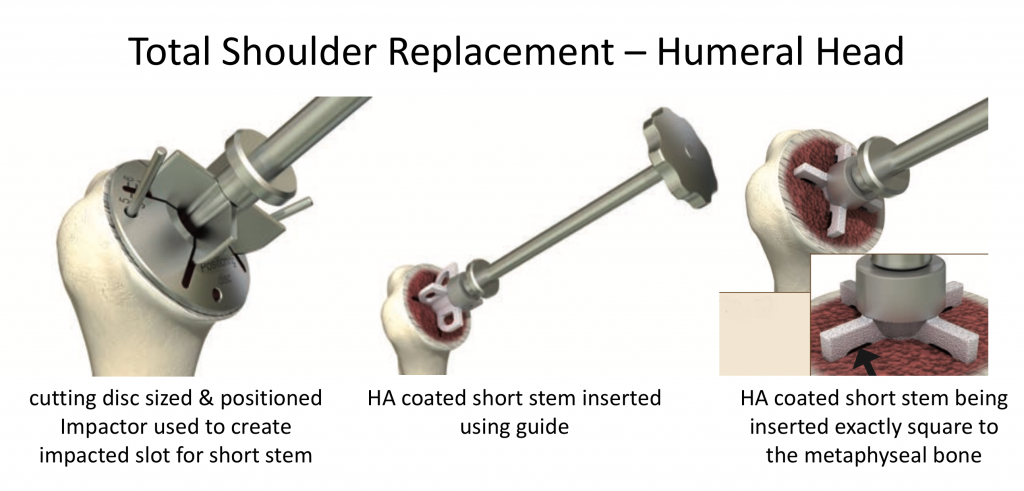
Humeral Stem – I use a Hydroxyapatite coated, short stem component. The short stem provides very good fixation and allows the option of using a long stemmed component if a revision is required. It also provides much better access to the glenoid and soft tissues at the time of surgery than a resurfacing component
Humeral Head - I use a ceramic humeral head. This has a lower coefficient of friction and is harder than a metal head. This results in less wear of the glenoid component
Glenoid Component – I use a pegged all plastic glenoid component made of highly cross-linked polyethylene enriched with Vitamin E. Vitamin E is an anti-oxidant which preserves the mechanical properties and increases the aging resistance of the polyethylene
The Affinis system has a long stem option, should this be required, and is part of a Platform System. A Platform System allows inter-changeability of the components with the Mathys Revision Shoulder and Shoulder Trauma systems, should the situation arise.
Having a Shoulder Replacement
A shoulder replacement is undertaken as an in-patient procedure. The patient is usually admitted to hospital on the day of their operation and usually stay in hospital for 2 or 3 nights. After the operation, the patient requires intensive physiotherapy. Their arm is in a sling for 3 to 4 weeks but is taken out regularly several times a day to undertake specific exercises as instructed by the physiotherapist.
Most patients can take their arm out of the sling at 4 weeks and use their arm for normal day to day activities by 6 weeks. Fully recovery usually takes 6 months and requires regular physiotherapy and exercises to stretch out and strengthen the rotator cuff muscles over this time.
My routine Total Shoulder Procedure and Rehabilitation protocol is described below,
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Inter scalene Nerve Block….
- Prophylactic antibiotics are then given
- A 10cm Delto-Pectoral incision (in the crease between the Deltoid and Pectoralis Major muscle is then made
- Dissection is then taken down to expose the shoulder
- The Subscapularis tendon is divided and retracted medially
- The Humeral Head is then dislocated and fully exposed
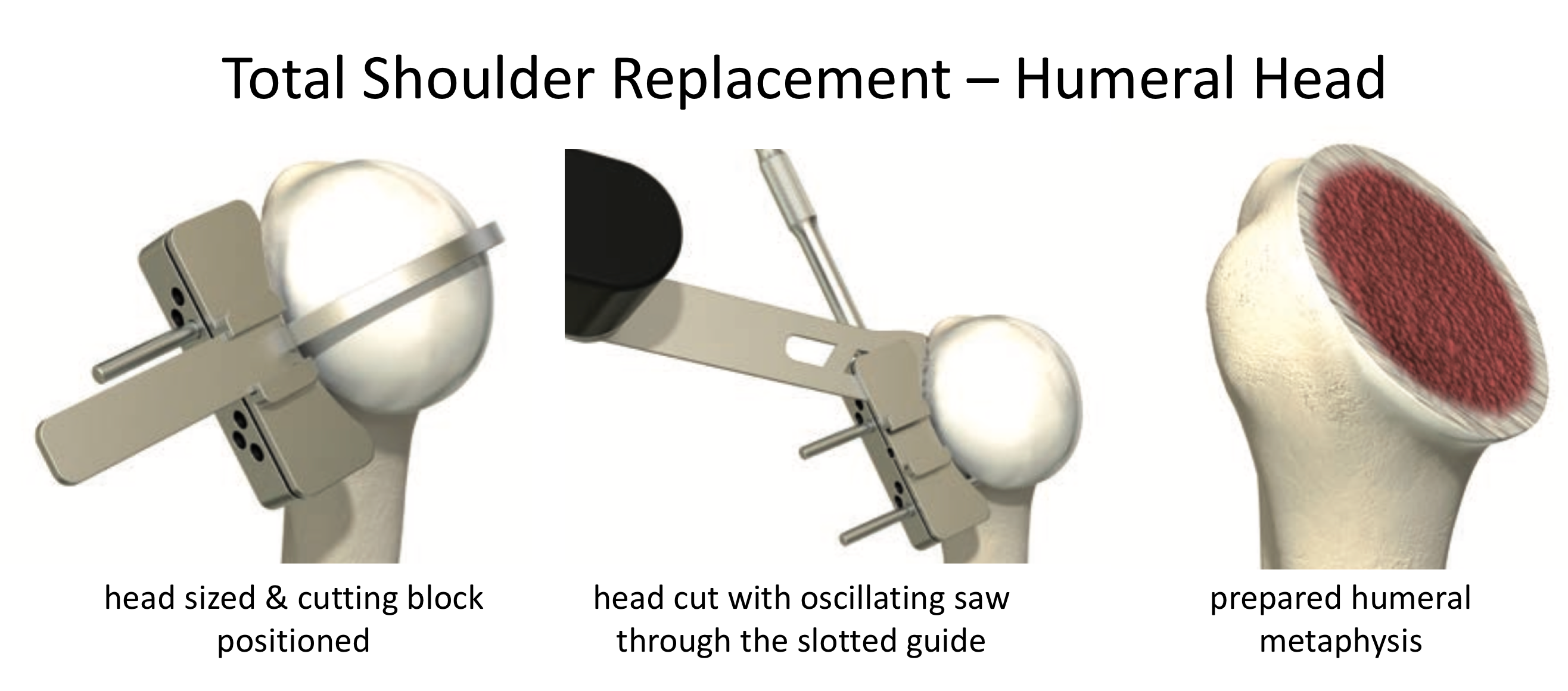
- The Humeral Head is then inspected and any osteophytes resected
- The Humeral Head is then resected using a cutting block
- The exposed bone is then sized and a jig used to punch out and then insert a trial short stem
- Having prepared the Humerus, a circumferential release of the capsule and soft-tissues is undertaken to fully expose the Glenoid
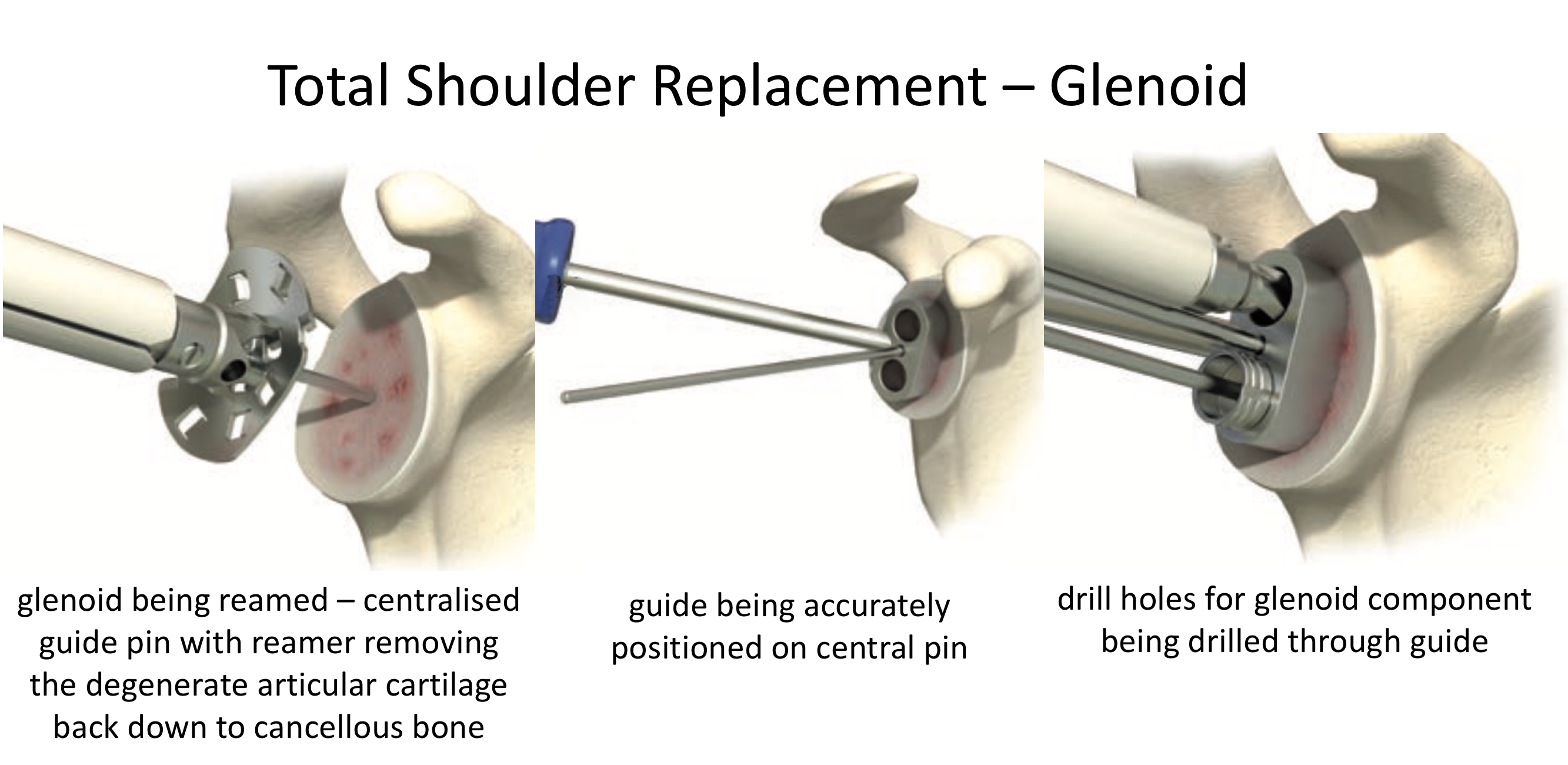
- The Glenoid bone is then reamed down to cancellous bone and sized for the glenoid component
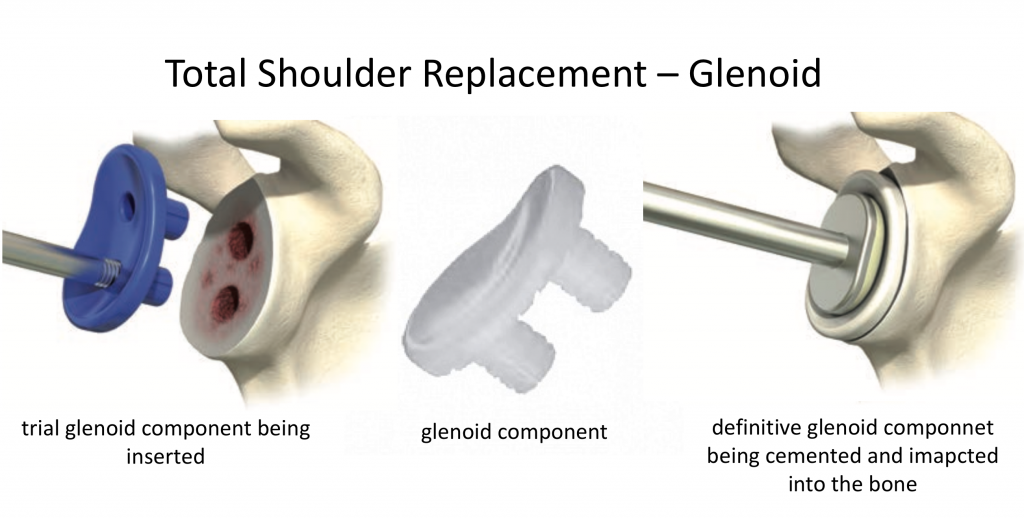
- Drill holes are then made and a trial Glenoid component inserted
- The trial component is then removed and the definitive component cemented into the bone using low viscosity methyl methacrylate cement
- The definitive Hydroxy Apatite coated Humeral Short stem is then implanted into the Humerus Fig
- A trial Humeral Head is then attached to the stem and the shoulder reduced
- Once the shoulder appears balanced the definitive ceramic Humeral Head is attached to the stem by a mortice and taper
- The joint is then reduced
- The joint has been repetitively washed out through the procedure and, after a thorough final washout the joint is then reduced and the Subscapularis Tendon repaired using interrupted sutures, incorporating a biceps tenodesis
- The wound is then closed in layers and the skin sutured using a subcuticular technique
After the Surgery
Post-Operative Care
Following a Total Shoulder Replacement, the patient is usually in hospital for 2 or 3 nights. Two further doses of prophylactic antibiotics will be administered over the next 16 hours and a check x-ray taken the next day. I would see the patient after the surgery to discuss how the procedure has gone and then see them each day to check on their progress and arrange for further Follow-Up.
The In-Patient Physiotherapy team will see the patient several times a day and will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after a Shoulder Replacement….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling.
Initially, following a Shoulder Replacement, it is very important to protect the Subscapularis Tendon repair. This is the tendon that is cut to gain access to the shoulder joint for the replacement, and is then repaired at the end of the operation. The movement that puts particular strain on the repair is External Rotation so, over the first month after surgery, it is important to avoid externally rotating the shoulder more than 100-150 degrees.
My standard rehabilitation protocol times are outlined below.
find out more about the specific rehabilitation exercises following a shoulder replacement….
information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Weeks 1 - 4
Weeks |
|
| Weeks 5 - 12 |
|
| Milestones | |
| Week 6 | Normal day to day activities out of sling |
| Month 3 | Improving day to day function and essentially pain free |
| Month 6 | Near optimum range of motion and strength |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | 4 – 6 weeks Below shoulder height |
| Work | 4 – 6 weeksSedentary - As able |
| Manual - 3 months, but activity may need to be reviewed | |
Success of Surgery, Risks & Complications
A Shoulder Replacement is usually a very successful procedure for pain relief and, following the recovery period, most patients are very happy with the result. However, shoulder replacements are not perfect and may ache a little when the weather changes or when someone has been too active.
As with any joint replacement operation there are always risks and complications associated with surgery.
General Risks
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Specific Risks
- Prosthesis Complications – Problems with modern day implants are very rare at the time of surgery. However, there is the potential risk of the bone fracturing around the implant. The main problems with implants is due to wear & tear over time. We do not know exactly how long implants of the latest design and of the current materials actually made last, as they have not been used for that long, but in normal circumstances they should last for at least 15 years before there are any issues with loosening or wear and tear.
- Infection – Infection is a possibility after any type of surgery. Every attempt is made to minimise this during a shoulder replacement by using prophylactic antibiotics, laminar flow operating theatres and strict surgical technique. However, infections do still occur in < 2.5% of cases.
- Nerve Injury - Damage tosignificant neurovascular structures during shoulder replacement surgery is rare < 0.5%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.