Arthritis
Arthritis of the Sternoclavicular Joint(SCJ Osteoarthritis, SCJ OA)
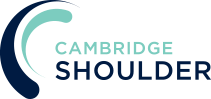
- due to its central position and role of connecting the upper limb to the rest of the body, the SCJ is constantly taking a massive load across it
- as a result, osteoarthritis (‘wear & tear’ arthritis) of the SCJ is very common as people get older. However, in the vast majority of people SCJ OA does not give them any symptoms (asympytomatic)
- We have recently published a study looking at SCJ CT scans of nearly 250 asymptomatic people of all ages and found,
- no one under the age of 35 years had OA changes
- nearly 90% of people over the age of 50 years did have OA changes
What are the symptoms of SCJ OA?
- the main symptom of SCJ OA is pain,
- pain is usually centered on the SCJ
- this can sometimes radiate up into the neck and down into chest and shoulder
- pain is often worse on protraction and retraction of the joint (shrugging forwards & backwards) and on elevating the shoulder on the affected side
- the SCJ is often swollen & can sometimes seem enlarged
- swelling with pain to touch is very common
- the medial end (inner end) of the clavicle can sometimes be enlarged, this is due to osteophyte formation
- the SCJ is enlarged with little pain
- most patients with OA of the SCJ are asymptomatic
- sometimes the joint can become enlarged due to OA osteophyte formation without pain
- sometimes the SCJ enlargement seems to appear quickly, however, the OA changes have often been going on in the background unnoticed for sometime
Could it be something else?
- SCJ OA is by far the most common cause of a painful swollen joint, however there are some other very unusual causes
- an unnoticed / forgotten previous injury
- infection
- inflammatory arthritis (such as rheumatoid or psoraitic arthritis)
- very rare syndromes (such a SAPHO or Condensing Osteitis)
- a secondary metastatic deposit
- if there is any concern that a painful, swollen and enlarged SCJ is not due to OA it should be investigated thoroughly
How do you diagnose SCJ OA?
- History –
- most people notice a gradual onset of pain and discomfort over the SCJ and chest wall
- occasionally a specific injury, incident or activity can spark this off
- the pain is often worse on elevating their arm and shrugging the shoulders forwards and backwards
- some people notice an associated swelling or enlargement of the joint, particularly over the end of the clavicle
- sometimes this asymmetry can actual develop over quite a long time and it may be worth patients looking at a photograph of themselves from 6 – 12 months before to see if anything was present then
- Examination –
- the joint is often enlarged and swollen and even may be red due to inflammation
- pain is often present on protraction and retraction of the shoulders, on internal and external rotation and on elevation of the arm
- there may be some clicking and grinding present with some subluxation/movement of the medial end of the clavicle
- Investigations –
- X-Ray – a standard x-ray of the SCJ is often difficult to interpret due to the presence of the vertebral column and ribs superimposed behind it
-
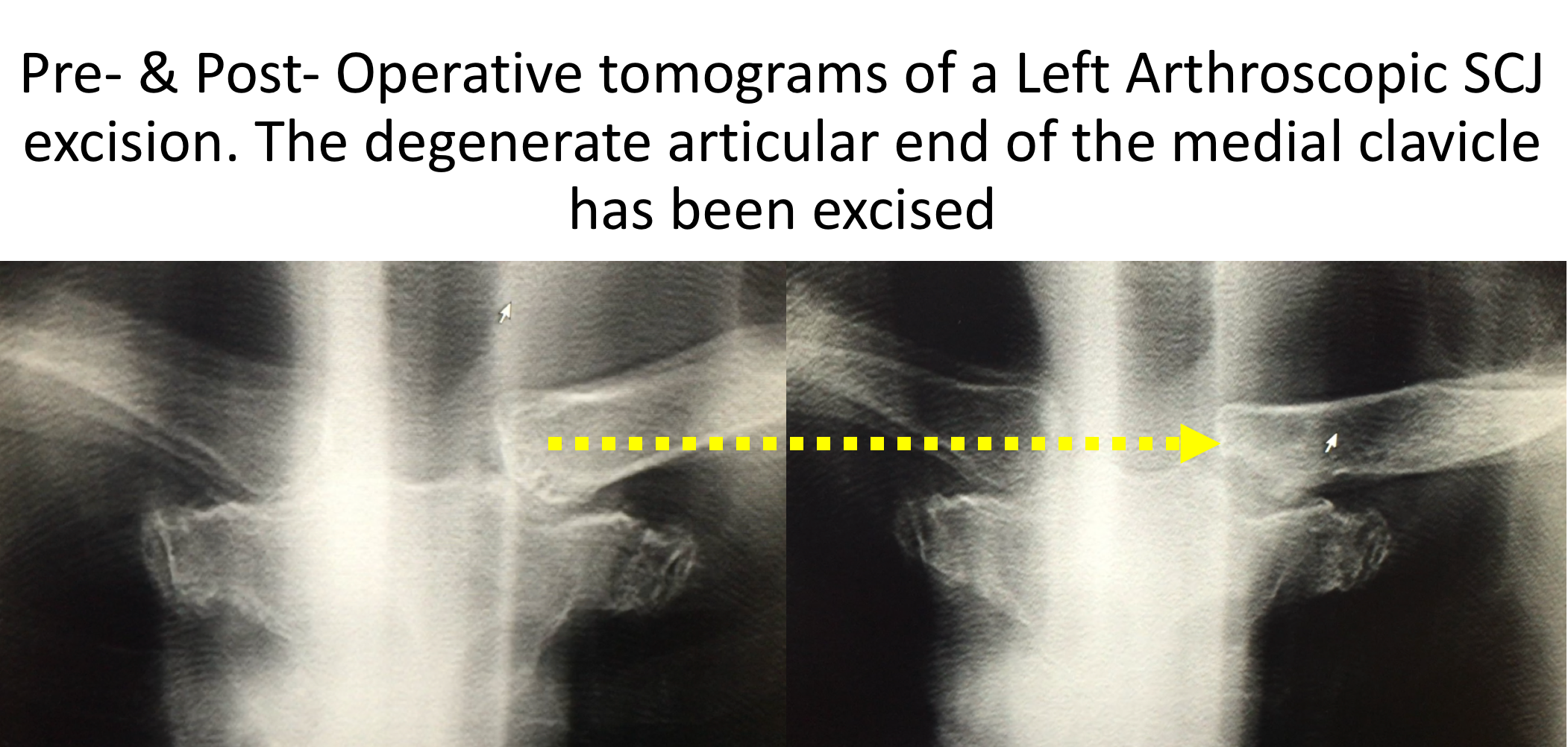
- Plain Tomogram – a tomogram is a sequence of 20 or 30 rapid x-rays each taken at a slightly different angle. This can be done by any modern digital x-ray machine in the same time that it takes for a standard single x-ray. This is a technique that we have recently described and gives as much information to diagnose osteoarthritis, a boney abnormality or a subluxation/dislocation as a CT scan
find out more about SCJ tomograms …
-
- CT Scan – a CT scan is a very useful investigation to look at the 3-D anatomy of the SCJ. This is often of use if surgery is being planned
- MRI Scan – an MRI scan gives the added information about the soft-tissue structures in and around the SCJ. It can give an indication as to whether there is an associated tear to the intra-articular disk, an inflammatory arthropathy, infection or any abnormalities within the bones
Management of SCJ OA
The vast majority of patients with symptomatic SCJ OA can be treated successfully by non-operative measures. The initial stage is to control the pain and settle the inflammation and then to re-establish function.
Analgesia/Pain Relief & Anti-Inflammatories
- pain is the major problem associated with a SCJ OA,
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response, they can be taken regularly as a prescribed course or as symptoms require
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
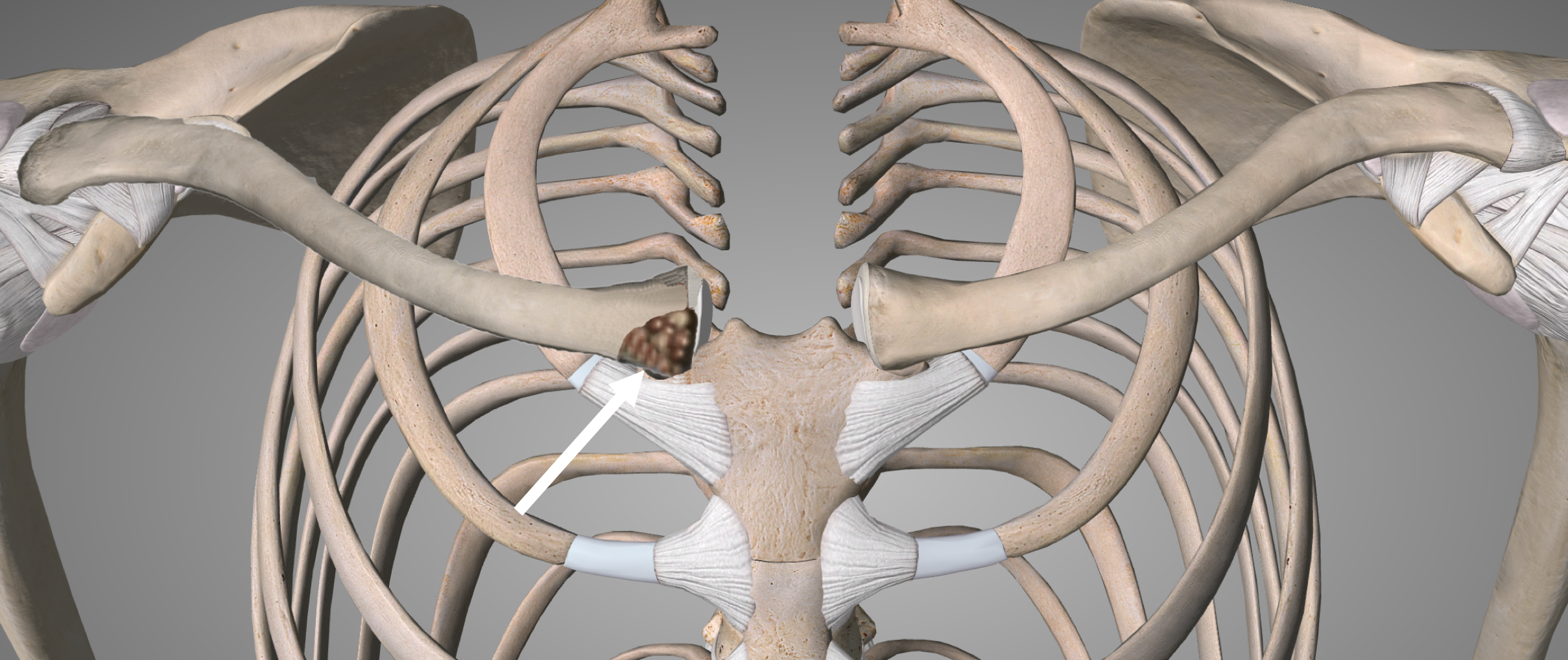
- Cortisone Injection
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the SCJ it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- a Cortisone injection can be very helpful for resistant SCJ OA
- due to the small size of the SCJ and the important other structures around it a Cortisone injection needs to be administered under Ultrasound guidance
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Physiotherapy
- if someone has had longstanding problems with their SCJ the often subconsciously develop compensatory movements and mechanisms to maintain function whilst working around the pain. This can sometimes lead to other problems elsewhere around the shoulder girdle
- physiotherapy can be very useful in regaining normal SCJ and shoulder function once the pain and discomfort has settled and to ‘un-learn’ the compensatory ‘bad-habits’
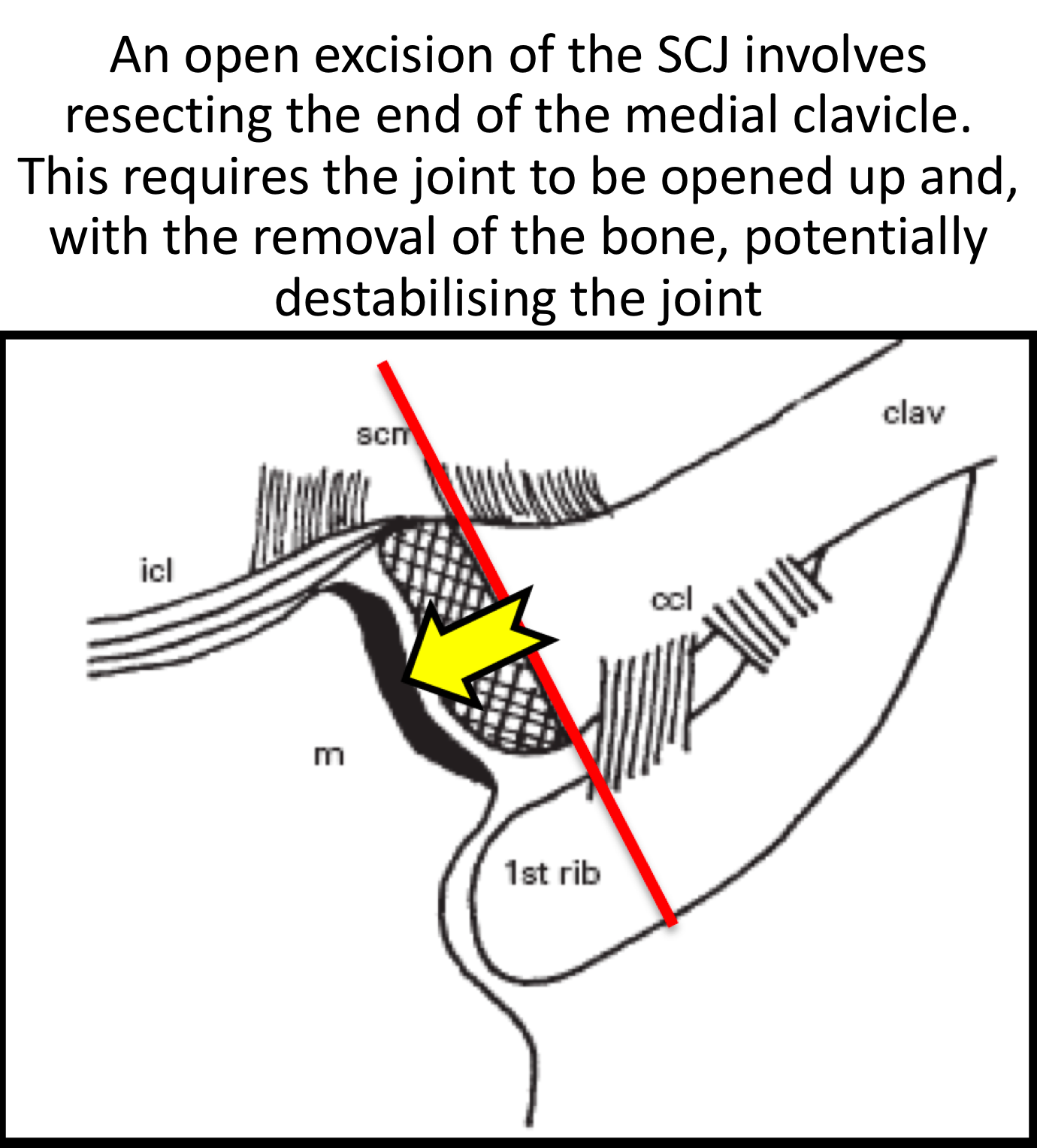
Surgery for SCJ OA
Until recently surgery for symptomatic SCJ OA was very rarely considered or undertaken. It was thought that the risks and potential complications of Open surgery, coupled with the protracted recovery time, were very significant. As a result, except in exceptional cases, it was felt that it was better and safer for a patient to put up with the symptoms rather than to have an operation. However, in Cambridge, we have described, developed and pioneered various arthroscopic (keyhole) surgical techniques to safely undertake SCJ surgery, often as a day-case procedure, with minimal morbidity and time to recovery.
Find out more about the development of SCJ arthroscopy….
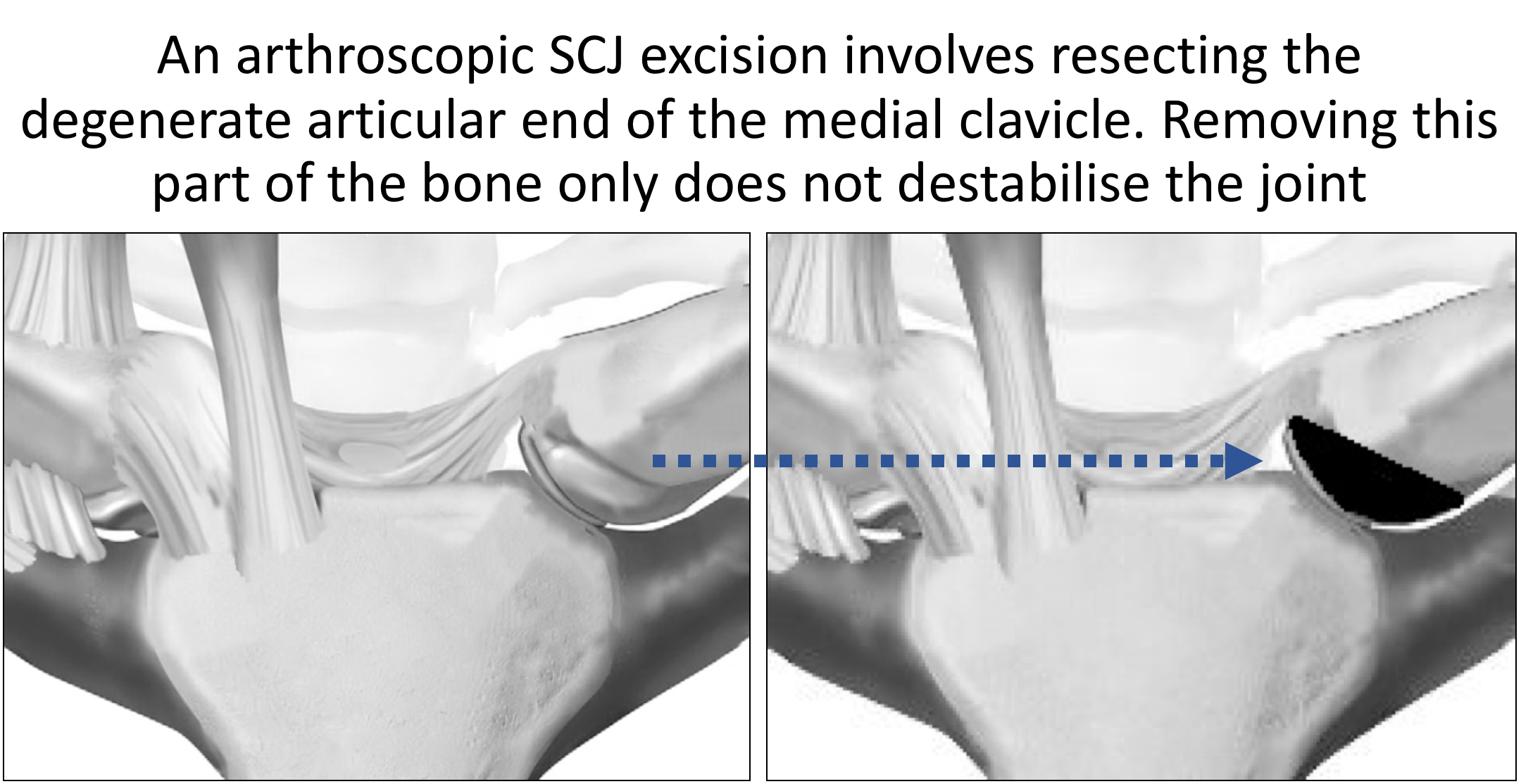
Arthroscopic SCJ Excision Arthroplasty
- the main source of symptoms and pain in SCJ OA is due to the articular cartilage, particularly on the clavicular side, having been damaged and worn away. As a result, the exposed bone ends rubbing on each other leads to pain and stiffness
- an Excision Arthroplasty involves removing the damaged bone ends and the associated soft-tissue damage. Fibrocartilage and fibrous tissue will form over the exposed bone ends alleviating the pain and returning some joint movement
- before specific joint replacements were developed Excision Arthroplasty was the treatment for severe osteoarthritis for every joint in the body. Whilst it relieved the pain it often left a significant functional deficit for the larger joints of the body (hip, knee & shoulder)
- fortunately, the normal SCJ only has a limited range of motion which can be completely recovered following an Excision Arthroplasty
- to undertake an SCJ Excision Arthroplasty as an Open procedure requires dividing the important stabilizing ligaments at the front of the joint and, to adequately resect sufficient damaged bone, often requires dissecting around the back of the joint, close to the important vessels and structures behind it. At the end of the procedure the ligaments need to be repaired and the patient often needs to have their shoulder immobilized for several weeks afterwards
- although an Open SCJ Excision Arthroplasty is a significant undertaking the results of the surgery, 6 months later, are usually very good
- an Arthroscopic SCJ Excision Arthroplasty can be undertaken without having to disturb any stabilizing ligaments and not needing to venture near to the important structures behind the joint
- an Arthroscopic SCJ Excision Arthroplasty, like an Open procedure, usually gives very good results without requiring any immobilization, any risks to the posterior structures and more quickly
- I undertake SCJ arthroscopies routinely and have done well over 200 cases
My routine Arthroscopic SCJ Excision Arthroplasty is described below,
- the patient is anaesthetised with a general anaesthetic
- the SCJ is carefully marked out and a 18G spinal needle inserted into the inferior part of the joint, below the anterior SC ligament
- having distended the joint with normal saline an inferior portal is established and a 2.9 mm arthroscope inserted. I use both a 300 and 700 scope during the procedure
- having assessed the joint a superior working portal is established under direct vision, above the anterior SC ligament
- the torn and degenerate SCJ intra-articular disk is completely excised
- using a combination of a shaver and radiofrequency probe the medial end of the clavicle is completely debrided
- using a burr 5 – 8 mm of the medial end of the clavicle is excised, taking particular care to remove the posterior and inferior osteophytes
- the sternal side of the joint, which is rarely affected, is assessed and any damage addressed
- haemostasis is then obtained, the joint finally assessed and the 2 wounds closed with subcuticular sutures and Steristrips
- local anaesthetic is then infiltrated around the joint
After the Surgery
Post-Operative Care
Following an Arthroscopic SCJ Excision Arthroplasty the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, the SCJ is numb from the local anaesthetic with a bulky dressing over it. The bulky dressing can be removed after a couple of hours and be replaced with small waterproof dressings. The SCJ may be painful once the local anaesthetic has worn off which is usually adequately controlled with routine oral analgesics which will be prescribed. I encourage patients to get their arm moving as quickly as possible, discomfort permitting.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
|
Milestones |
|
|
Week 3 |
Full passive range of movement |
|
Week 6 |
Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated Overhead Activities |
|
| Lifting |
|
| Work |
|
Success of Surgery, Risks & Complications
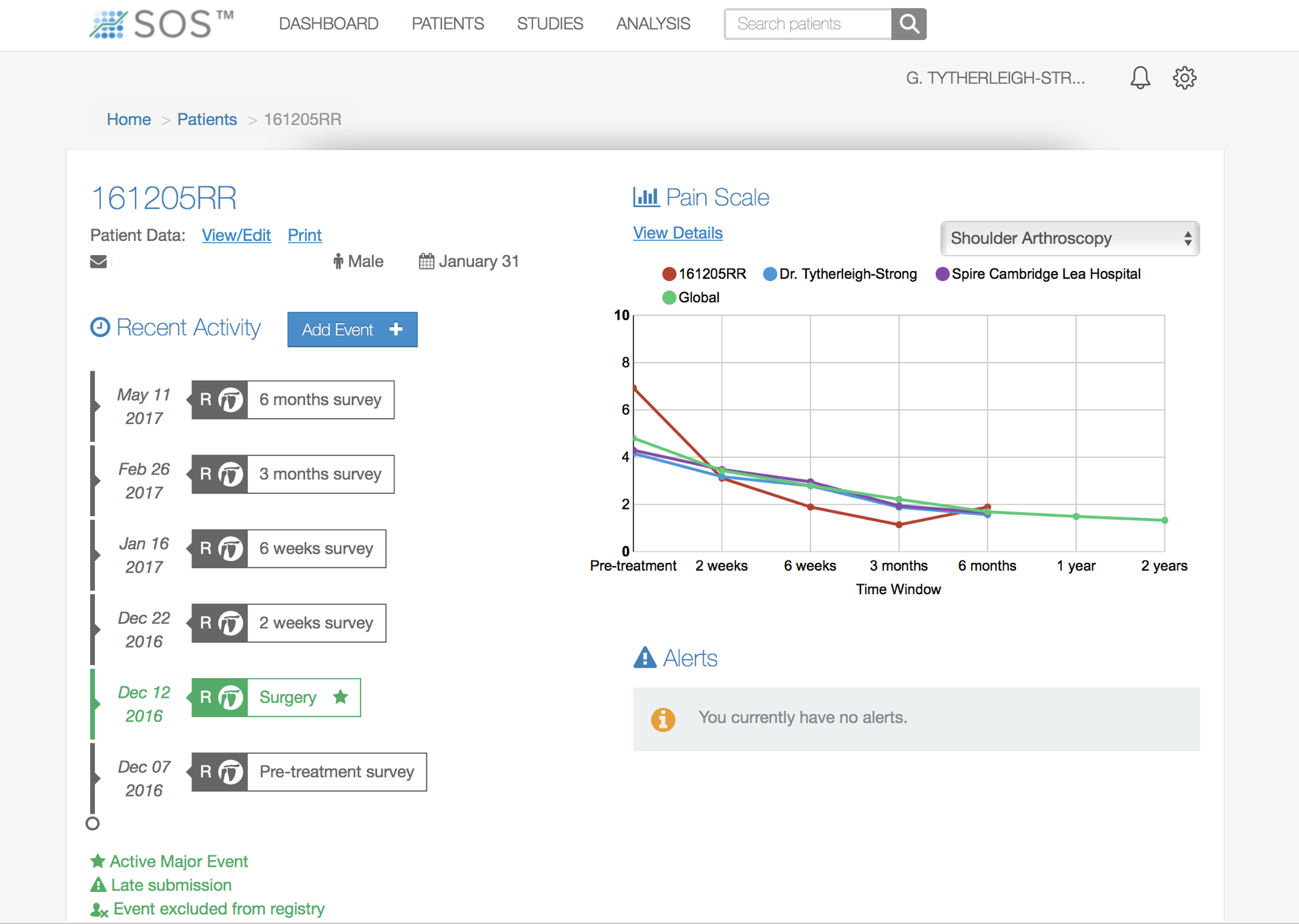
An Arthroscopic SCJ Excision Arthroplasty is usually a very successful procedure but, because it takes some time for the tissues around the SCJ to recover and for the fibrocartilage to form, it usually takes between 3 – 6 months for the SCJ to be as good as it can be. Our published results found that 90% of patients were happy with their SCJ after 6 months.
find out more about the results of SCJ Intra-Articular Disk Surgery…
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
find out more about the SOS outcome system…