The Acromioclavicular Joint (ACJ)
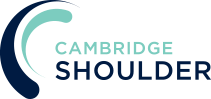
- the Acromioclavicular Joint is formed by the lateral (outer) end of the clavicle (collar-bone) and the Acromion
- is a plain synovial joint and the ends of the bone are covered by articular hyaline cartilage
- a partial fibrocartilaginous articular disk is present in some joints
- it is surrounded by a synovial lined joint capsule
- thickenings within the joint capsule form the Acromioclavicular Ligaments
- the ACJ allows a degree of axial rotation and anterior-posterior movement
Ligaments
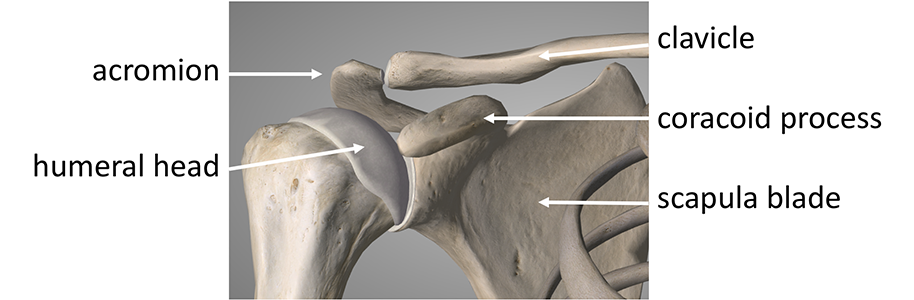
The ACJ is stabilized by 3 main ligaments
- Superior, Anterior & Posterior Acromioclavicular Ligts – these ligaments are formed as thickenings of the joint capsule and stabilize the joint against superior, anterior and posterior movement
- CoracoclavicularLigts – the 2 short but very strong coracoclavicular ligaments run from the top of the coracoid process to the undersurface of the clavicle. They stabilize the lateral end of the clavicle from superior forces.
- Conoid Ligament – the Conoid ligament is a short cylindrical ligament that runs from the posterior medial part of the hook of the coracoid and inserts into the conoid tubercle on the undersurface of the clavicle
- Trapezoid Ligament – the Trapezoid ligament is a broader fan shaped ligament, in 2 parts, that runs from the anterior lateral part of the hook of the coracoid to the trapezoid line on the undersurface of the clavicle
Acromioclavicular Joint Problems
- the main job of the Clavicle is to ‘strutt’ the shoulder girdle out to allow it to work in a more advantageous mechanical position
- the ACJ is a focal point for all of the load taken by the upper limb to be ‘passed’ through to the Sternum (breast bone) and so to the axial skeleton
- the main problems that affect the ACJ are ligamentous injuries & dislocations (which usually result from a fall onto the point of the shoulder) and Osteoarthritis, developed by the load that passes through it.
Acromioclavicular Joint Injury – (ACJ Separation, ACJ Dislocation)
- the Acromioclavicular Joint (ACJ) plays a very important role in connecting the Clavicle to the Scapula, essentially connecting the shoulder complex to the rest of the axial skeleton
find out more about the Scapula and its parts….
- due to its position, it is vulnerable to injury particularly when someone falls on the ‘point’ of their shoulder
- when someone falls on the ACJ the Acromion is forced downwards putting a massive force on the ACJ and its stabilising ligaments leading to injury
- depending on the severity of this force the Acromioclavicular Ligaments, the Coracoclavicular ligaments and the supporting muscle attachments of the clavicle can be injured and torn, in this sequence
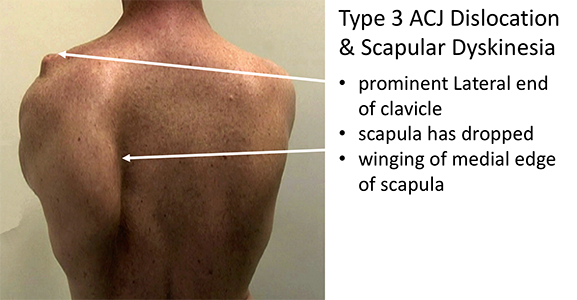
- the effect of an ACJ injury not only result in the displacement of the clavicle upwards with associated dysfunction & pain around the ACJ but can also have a varying effect on the way that the rest of the shoulder complex moves and works resulting in an element of Scapula Dyskinesia
find out more about Scapula Dyskinesia….
- the essence of successful management and treatment of an ACJ injury is not the cosmetic appearance of the end of the clavicle but trying to regain normal shoulder function
Mechanism of Injury
- most ACJ injuries occur when someone falls on to the point of their shoulder forcing the Acromion downwards
- this is a common sporting injury (cycling, rugby, horse-riding, skiing etc) but can occur after anytime type of fall
- the extent of the injury depends on the magnitude of force
- Injury can range from a sprain of the Acromioclavicular (AC) ligaments to complete disruption of the AC ligaments, Coracoclavicular (CC) ligaments and the surrounding muscle envelope
Classification of ACJ Injuries / Dislocations
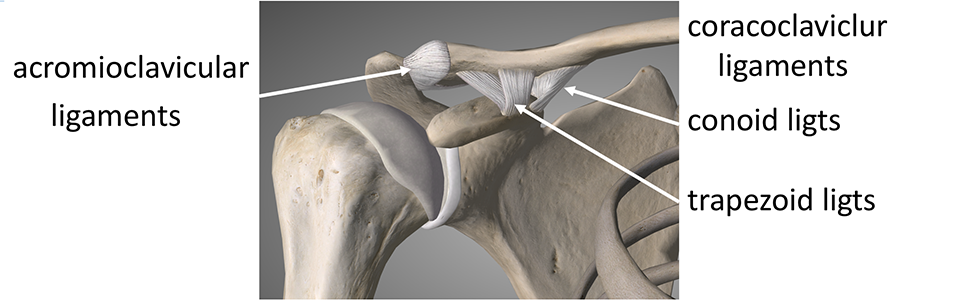
- ACJ injuries are usually classified by the x-ray findings
- the classification is useful to indicate the severity of the injury and can be a useful guide to treatment
- Type 1 – the Superior AC ligament is sprained with minimal displacement of the clavicle
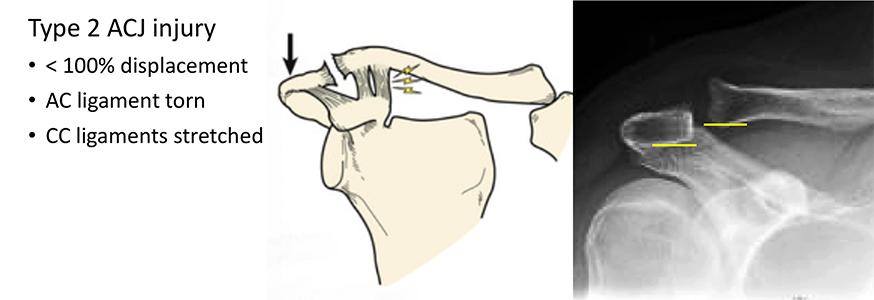
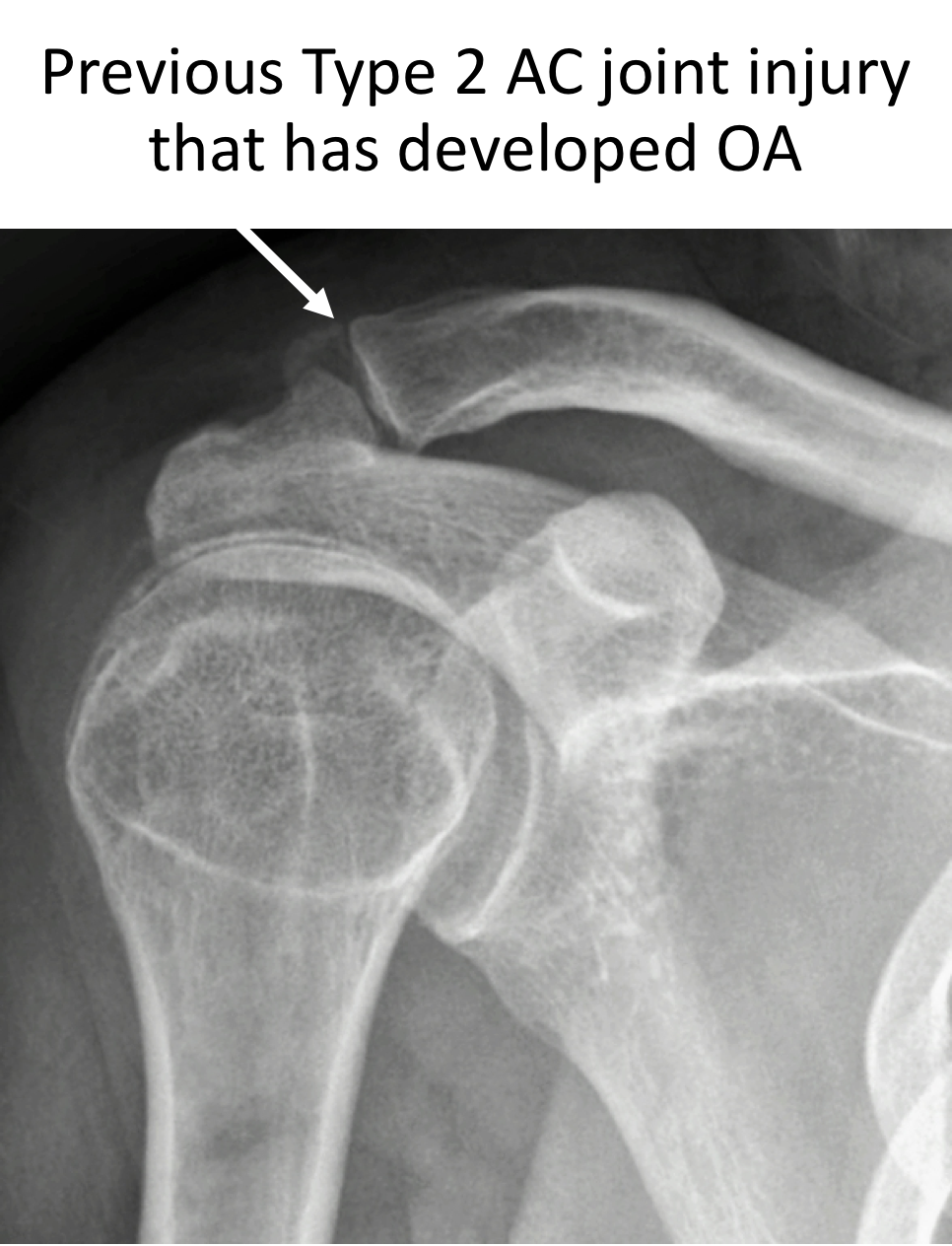
- Type 2 – the AC ligaments are completely torn with an associated sprain/stretching of the CC ligaments. The clavicle is displaced upwards, but less than the height of the acromion
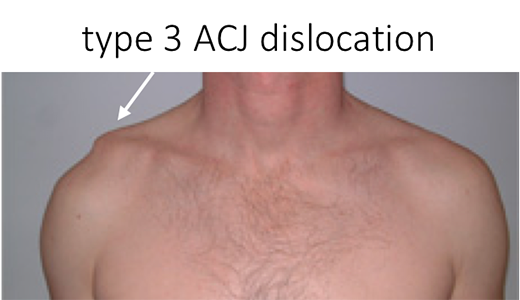
- Type 3 – the AC & CC ligaments are completely torn with the clavicle displaced more than 100% of the height of the acromion
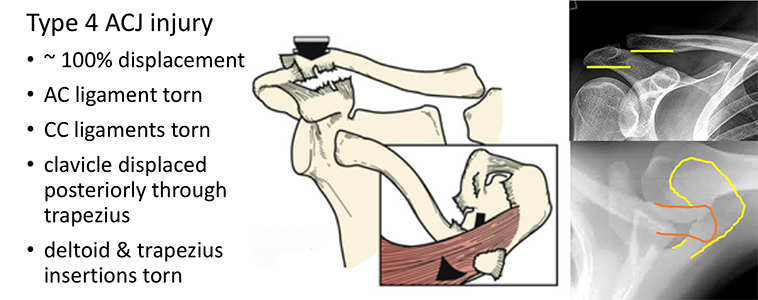
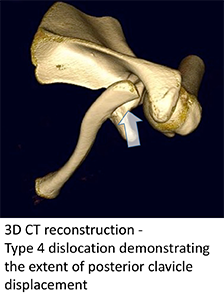
- Type 4 – In this type of injury, the sustained force, as well as pushing the acromion downwards has also had a component force pushing the clavicle backwards. The AC & CC ligaments are completely torn and the end of the clavicle has been forced backwards and has ‘button-holed’ through the trapezius muscle. This is best appreciated on the axillary view x-ray
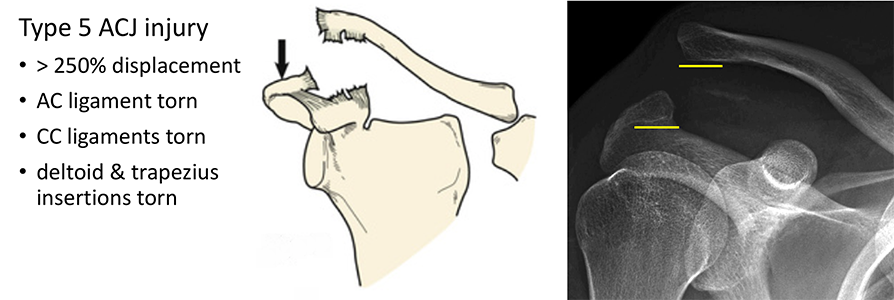
- Type 5 – the AC & CC ligaments have been completely torn and the insertions of deltoid and trapezius have been pulled off. There is significant displacement of the clavicle more than 250% of the height of the acromion
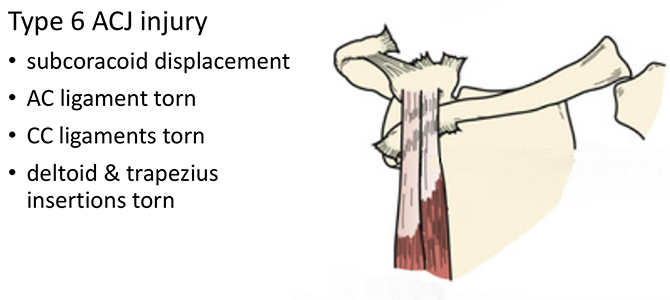
- Type 6 – the AC & CC ligaments have been completely torn and the insertions of deltoid and trapezius have been pulled off. The clavicle has been displaced into a sub-coracoid position (this type of injury has almost never been reported!)
- however, the x-ray findings do not always tell the whole story and particularly the exact extent of the soft-tissue injury
- the best treatment and management for an individual patient is dependent on the clinical findings as well as the x-ray
Diagnosis of an Acromioclavicular Joint Injuries/Dislocations
To diagnose & treat an Acromioclavicular Joint Dislocation, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. When an ACJ Dislocation has occurred as part of a major accident the priority is to treat any life-threatening or more major injuries first. The best treatment for a particular patient with an ACJ dislocation can depend on the severity of their symptoms and other associated shoulder conditions.
History
- in most cases of ACJ OA there has been a significant injury where the patient has either landed or been hit on the point of their shoulder
- following an acute injury, it is initially important to check for any other more significant associated injuries which includes neurological symptoms related to possible damage to the Brachial Plexus
- the main symptom is of pain with an associated prominence of the lateral end of the clavicle
- in more chronic cases there may also be associated problems with shoulder and scapula (shoulder blade) function due to pain and weakness
Examination
- on inspection there is usually an obvious superior displacement of the lateral end of the clavicle, this may initially be accentuated by associated swelling
- in acute cases, there may be associated grazing or even a laceration to the overlying skin, bruising tends to appear several days after the injury
- it is important to ascertain the position of the lateral end of the clavicle with relation to the acromion, including
- the amount of superior displacement
- whether the clavicle has translated posteriorly into the trapezius
- whether the clavicle can be ‘reduced’ back into normal alignment
- in acute cases, it may be difficult to assess shoulder and scapula function due to pain
- in chronic cases shoulder function is the most important determinant of treatment
- despite significant displacement and movement of the clavicle, shoulder function may be completely normal and pain free
- pain may continue to be a feature despite minimal displacement of the clavicle
- assessment of Scapulo-Humeral rhythm and movement with any associated Scapular Dyskinesia is important and is assessed by looking at the patient from behind and comparing the movement between the injured and non-injured shoulders
find out more about scapulo-humeral rhythm and scapula dyskinesia ….
find out more about examination of the shoulder …..
Investigations
- X-Ray – a plain, good quality AP & Axillary x-ray of the shoulder will normally provide sufficient information to diagnose and classify an ACJ dislocation
- an x-ray may identify any other boney injuries or associated fractures
- in chronic cases there may be evidence of developing ACJ osteoarthritis
- sometimes calcification of the torn CC ligaments may be present underneath the clavicle
- CT Scan – a CT scan can sometimes be of use to more clearly see the position of the displaced clavicle when planning surgery
Find out more about CT Scans of the shoulder ….
- MRI Scan – an MRI scan may be indicated to assess whether there are any other associated soft tissue injuries, particularly to the rotator cuff muscles and tendons
- specific MRI scan cuts can demonstrate CC ligament injury and disruption
Treatment of Acromioclavicular Joint Injuries/Dislocations
The most appropriate management of an ACJ dislocation can, on the face of it, sometimes appear to be a bit counter-intuitive. It is very common for someone with a Grade 3 ACJ dislocation to regain complete, pain free shoulder function with the end of the clavicle still remaining in its elevated position. In fact, there is a danger, that operating on an asymptomatic pain free dislocated ACJ, in an attempt to improve its position, can result in the joint ending up being more painful. An ACJ stabilization operation rarely makes the joint 100% better for all activities but, when undertaken on someone with significant symptoms, it can make a massive improvement to their pre-operative symptoms.
Traditionally the Grade/Type of the ACJ dislocation determines the treatment. However, the evidence for this is poor. We therefore treat ACJ injuries according to their symptoms (pain & function) and speed of recovery, rather than Grade.
- most people with an ACJ dislocation will recover fully without surgery
- people who do a lot of high-demand overhead activities or are high-demand athletes may benefit from surgery
- the long-term outcome is usually the same whether someone has had surgery or not
- a patient is likely to recover more quickly if their shoulder settles without surgery than if they have an operation
- surgery has a failure rate of up to 20%
- the success of surgery is usually independent of time, in that an operation done months or years after an injury is likely to be just as successful as one done within a week of injury
Treatment Algorithm
Acute Injury (Week 1)
- rest & analgesia – review at 3 weeks
- initial rest in a sling, an ice pack and Non-Steroidal Anti-inflammatories
- there is no benefit from any type of strapping or compression dressing to try and push the clavicle back down into position
- as soon as the shoulder is comfortable it is most appropriate to begin to gently mobilise the glenohumeral joint and shoulder blade as pain permits
- supervision by a physiotherapist is of benefit
- surgery
- indicated if, - open injury, neurological injury or obvious severe button-holing (Type 4 or 5)
3 Week Review
- once the shoulder is more comfortable active range of motion and mobilization exercises can begin working towards a strengthening program
- the patient should be aiming to gradually re-introduce sports and manual-activities over this time
- surgery
- indicated if patient is failing to progress and not coping
- patient developing significant Scapular Dyskinesia
3 Month Review
- patient should have returned to full activities and sports with little symptoms
- surgery
- indicated if a patient’s recovery has plateaued or failed to progress
Management of Delayed Recovery & Failure of Non-Operative Treatment
Type 1 & Type 2 ACJ Injuries
- following a Type 1 & Type 2 ACJ injury the Coracoclavicular (CC) ligaments will usually fully recover
- as a result, long term problems following a Type 1 or Type 2 injury are usually due to pain at the ACJ without problems related to displacement of the lateral end of the clavicle or instability
Diagnosis
- X-Ray – a plain, good quality AP & Axillary x-ray of the shoulder will normally provide sufficient information to investigate the cause of on-going ACJ pain
- An x-ray can check for any changes, particularly in the position of the clavicle following the initial injury
- an x-ray may identify any other boney injuries or associated fractures
- in chronic cases there may be evidence of a developing ACJ osteoarthritis
- MRI Scan – an MRI scan may be indicated to assess whether there are any other associated soft tissue injuries, particularly to the rotator cuff muscles and tendons
Find out more about MRI scans of the shoulder…..
Treatment
Cortisone Injection
- a simple Cortisone injection may be sufficient to settle on-going inflammation following an ACJ injury
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the ACJ it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- it can usually be injected simply in the Out-Patient Clinic or under Ultrasound Guidance
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Surgery for Type 1 & Type 2 ACJ Injuries
- Surgical Excision of the ACJ is the most appropriate operation for someone with on-going pain following a Type 1 or Type 2 ACJ injury
- this is also the case for patients who have failed or have only had a transient response to a Cortisone injection
- surgical excision of the ACJ is a relatively simple and very successful procedure with a quick recovery time
- an ACJ excision can be done as an Open or Arthroscopic procedure. I prefer to undertake an arthroscopic procedure as it allows for a far more rapid recovery
- this is exactly the same procedure as is used for ACJ Osteoarthritis and Distal Clavicular Osteolysis (“Weight-Lifter’s Shoulder”)
Arthroscopic Acromioclavicular Joint Excision
-(ACJ Excision, ACJ Excision arthroplasty) …
Type 3, 4 & 5 ACJ Injuries
- during a Type 3,4 or 5 ACJ dislocation the Coracoclavicular (CC) ligaments are completely torn
- the CC ligaments do not heal
- if stability returns it is due to fibrous scar tissue that forms around the clavicle during the healing process
- problems related to a Type 3,4 & 5 ACJ dislocation are due to instability or malposition of the end of the clavicle leading to pain, loss of function and Scapular Dyskinesia
- surgical treatment involves,
- reducing the clavicle back into position
- stabilising the clavicle by reconstructing the CC ligaments
Surgery for Acromioclavicular Joint Dislocations
Type 3, 4 & 5 ACJ Injuries
- during a Type 3,4 or 5 ACJ dislocation the Coracoclavicular (CC) ligaments are completely torn
- the CC ligaments do not heal
- if stability returns it is due to fibrous scar tissue that forms around the clavicle during the healing process
- problems related to a Type 3,4 & 5 ACJ dislocation are due to instability or malposition of the end of the clavicle leading to pain, loss of function and Scapular Dyskinesia
- surgical treatment involves,
- reducing the clavicle back into position
- stabilising the clavicle by reconstructing the CC ligaments
Surgery for Type 3,4 & 5 ACJ Injuries
Many different types of surgical procedures have been described to treat ACJ dislocations with varying success. However, regardless of the procedure the key components are reducing the clavicle, reconstructing the CC ligaments and holding the construct in position whilst the soft-tissues heal and strengthen.
The main goal of surgery is to improve function and pain. Whilst the position of the displaced clavicle is corrected, the contour of the shoulder may not return exactly. There may always be some residual asymmetry between the contour of the operated shoulder and the non-injured side.
The procedures that I prefer to use are,
- open synthetic ligament reconstruction +/- hamstring tendon
(used for Acute & Chronic dislocations)
- arthroscopic tight-rope reconstruction +/- hamstring tendon
(used for Acute dislocations)
- hook-plate reconstruction
(used in exceptional revision situations)
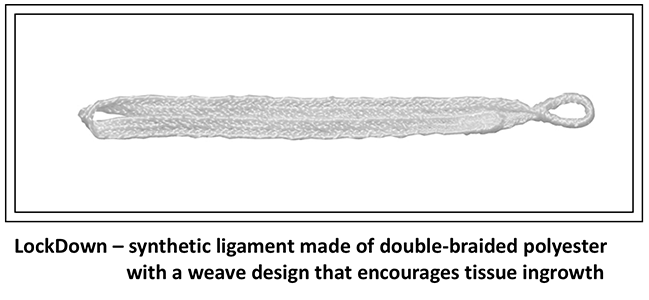
Acromioclavicular Joint Reconstruction – Synthetic Ligament
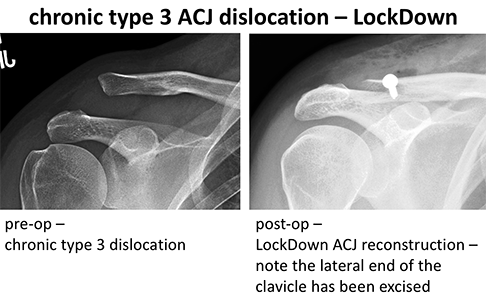
My preferred ACJ reconstruction procedure is an open stabilisation using a LockDownTM synthetic ligament. This is made of double-braided polyester with a weave-design that acts as a scaffold that encourages tissue in-growth. It provides immediate superior-inferior stability and significant anterior-posterior stability. Eventually a fibrous neo-ligament forms around and within the weaved implant recreating the CC ligaments. (Figs 21 & 22)
My routine Open Acromioclavicular Joint Reconstruction using a LockDown synthetic ligament is described below,
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic…
Find out more about an Interscalene Nerve Block…
- A single prophylactic dose of broad-spectrum anti-biotics is administered
- An 8 – 10 cm sabre incision is made from the posterior edge of the clavicle to just above the coracoid tip
- The Platysma is divided and the Deltoid & Trapezius are split and elevated off of the clavicle, ACJ and medial acromion
- The lateral end of the clavicle id then fully exposed
- In an Acute Case the joint disk and soft-tissues are cleared to allow for reduction of the clavicle. In a Chronic Case, and if there was any evidence of any pre-existing OA, the lateral 1 cm of the clavicle is resected angling the cut from posterior-lateral to anterior-medial
- The end of the clavicle is then elevated up to allow access to the Coracoid
- Part of coracoacromial ligament and the pec minor insertions are then elevated off of the coracoid to allow access to its under surface
- Taking care that the neurovascular structures are protected, a curved introduce is passed under the coracoid from the medial to lateral side
- The LockDown length-gauge is then passed around the clavicle, looped through itself, passed behind the clavicle and then pulled over the anterior edge of the clavicle, which is held in the reduced position. The length of the required implant is then read-off
- The length-gauge is then removed and replaced by the definitive LockDown implant. This is secured to the anterior edge of the clavicle using a 3.5mm cortical screw and washer angled medially
- If it is felt that the repair needs to be augmented a hamstring tendon autograft can be looped around the reconstruction for further support
- Haemostasis is achieved and the deltoid and trapezius muscles are imbricated over the clavicle and the wound closed in layers
Find out more about having an operation
After the Surgery
Post-Operative Care
Following an Open Acromioclavicular Joint Reconstruction, the patient requires a check x-ray and maybe able to go home on the same day as their surgery or may need to stay in the hospital over-night. (Figs 24) This decision would depend on various associated factors.
I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder and how to use their Sling. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following Shoulder Surgery…
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. After the nerve block has worn off the arm can come out of the sling for washing and dressing and for certain controlled movements, as directed by the physiotherapists.
After an Acromioclavicular Joint Reconstruction, it is initially important to ‘protect’ the repair from any significant load, and patients should restrict their arm movements to below shoulder height. Patients would usually need to have their arm in a broad-arm sling for 2 weeks and use their arm when in a safe environment. Part of the recovery, especially for chronic dislocations, is re-establishing normal scapulothoracic movements, this may take several months.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Post op | |
| Immediate |
|
|
Day 1-3 Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
| Milestones | |
| Week 6 | 75% of full ROM, comfortable out of sling |
| Week 12 | Full ROM, 90% to full strength |
|
Return to Functional Activities |
|
| Driving |
|
|
Swimming |
|
| Lifting |
|
| Work |
|
| Manual |
|
Success of Surgery, Risks & Complications
An Acromioclavicular Joint Reconstruction using a LockDown is usually a very successful procedure with regards to alleviating pain and restoring good function. However, in can take between 3 – 6 months or longer to achieve. The surgery is aimed at improving pain and function and less so at cosmesis, as a result, most patients still have an element of asymmetry between their shoulders after successful surgery.
At 6 months after an Acromioclavicular Joint Reconstruction using a LockDown over 80% of patients are happy with their shoulder and have returned to all recreational, work and sport activities. About 10-15% of patients still have occasional problems with certain shoulder activities, but are pleased that they have had surgery and about 5% of patients do not feel that their shoulder has significantly improved, although it is no worse than before.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken
- Failure – About 20% of ACJ reconstructions stretch-out. However, this does NOT always lead to a recurrence of the symptoms
- Infection – Infection following open shoulder surgery is rare and occurs in about 1% of cases
- Neurovascular Injury – Damage tosignificant neurovascular structures during subcoracoid shoulder surgery is rare < 0.5%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
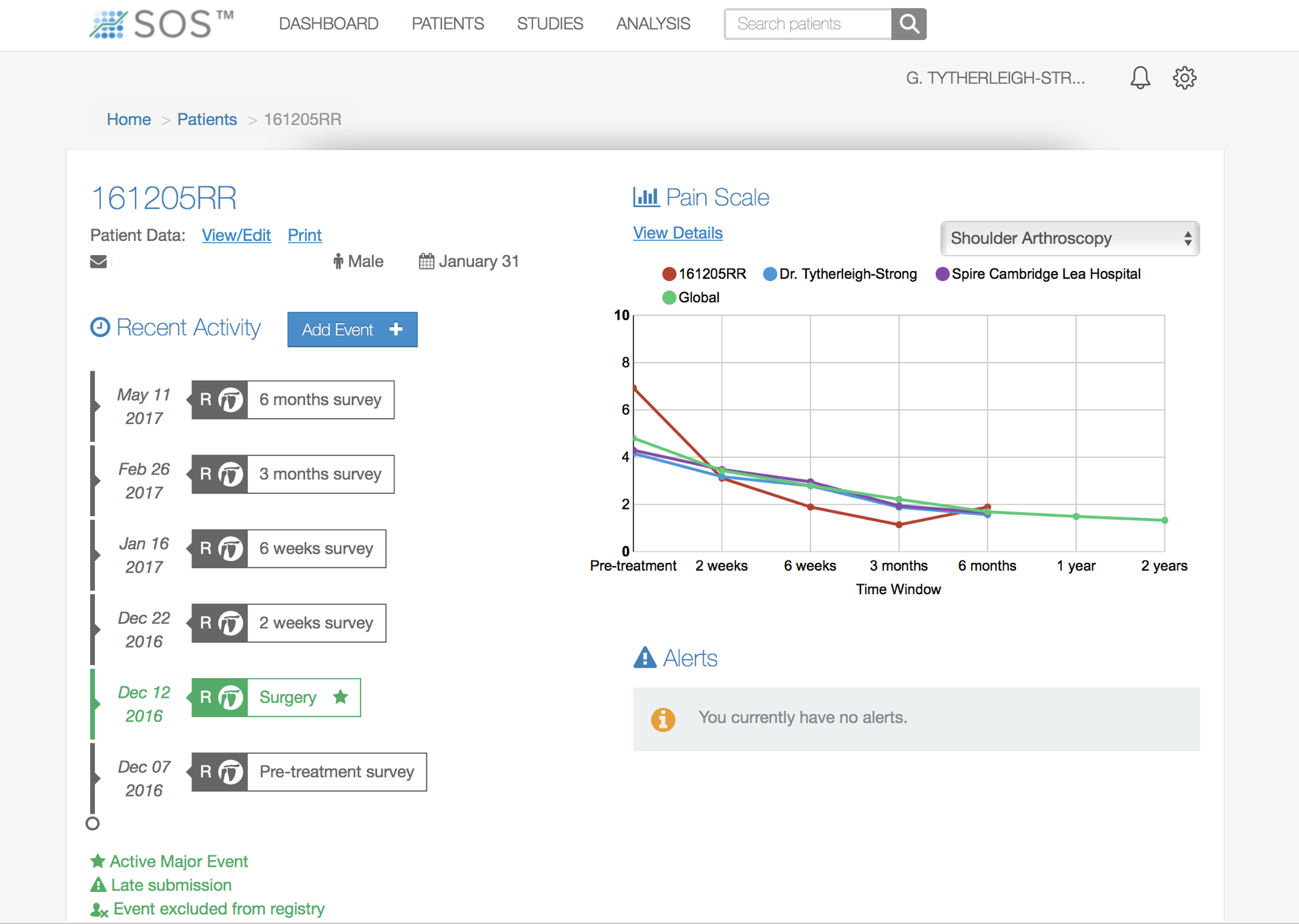
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
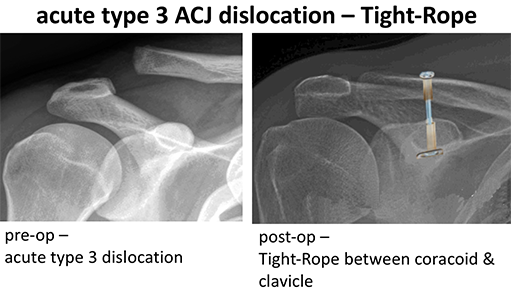
Acromioclavicular Joint Reconstruction – Arthroscopic Tight-Rope Procedure
Another technique for stabilising the clavicle and reconstructing the Acromioclavicular Joint is a Tight-Rope procedure. This involves passing a quadruple strand single-core suture between holes in the coracoid and the reduced clavicle and then fixing either end of the sutures in place with specialised metal buttons. This is a procedure that can be done arthroscopically. This has the advantage of a potentially better cosmetic appearance as a much smaller sabre incision is required with only a couple of additional arthroscopic portal incisions. (Fig 24 & 25)
I tend to reserve the use of a Tight-Rope Procedure for Acute ACJ Injuries only (within 3 weeks of injury). Following an Acute injury there will be a lot of inflamed and healing tissue around the damaged CC ligaments. If the clavicle is reduced and stabilised at this time, the healing tissue is likely to form a strong, fibrous neo-ligament between the coracoid and clavicle.
Following a Chronic injury established scar tissue sits between the coracoid and displaced clavicle. There is some concern, that by reducing and stabilising the clavicle using an arthroscopic Tight-Rope technique in the Chronic situation, insufficient new scar tissue will form to create an adequate neo-ligament. As a result, if I were to contemplate using a Tight-Rope technique in a Chronic Injury I would consider using an additional Hamstring Graft to augment the repair. (Fig 26)
My standard post-operative and rehabilitation protocol is the same for all types of Acromioclavicular Joint Reconstructions, regardless of which technique has been used.
Find out more about arthroscopic shoulder surgery….
Find out more about ACJ Reconstruction – Post-Operative & Rehabilitation protocol….
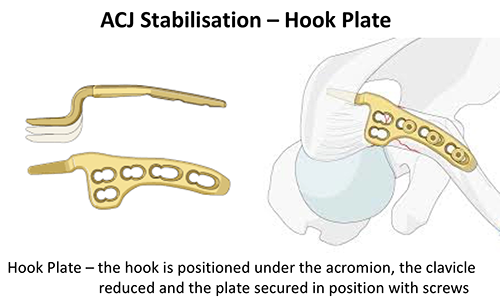
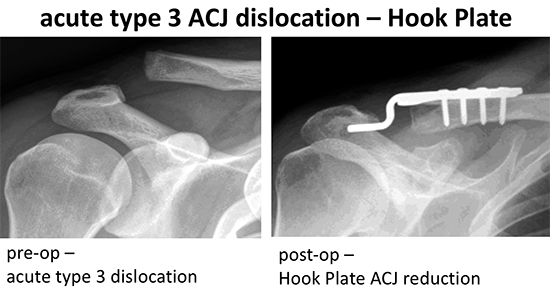
Acromioclavicular Joint Reconstruction – Hook-Plate
The basis of both the LockDown and Tight-Rope Acromioclavicular Joint Reconstruction procedures is that the attempt to re-create the CC ligaments to hold the clavicle in position. A Hook Plate works differently, in that hooked end of the plate is positioned under the acromion and just holds the clavicle in position without attempting to reconstruct the CC ligaments. (Fig 29)
The advantage of the Hook Plate is that it is easy to use and is a very powerful way to hold the clavicle in a reduced position. However, it almost always needs a second operation to be removed, due to pain and impingement that is caused by the hook underneath the acromion. The hook under the acromion can also limit movements of the arm above shoulder height. Also, as with the Tight-Rope procedure, there are some concerns in using a Hook Plate for a Chronic ACJ dislocation and, if it were to be considered, a Hamstring Graft may be required to augment the repair. (Fig 30)
My standard post-operative and rehabilitation protocol is the same for all types of Acromioclavicular Joint Reconstructions, regardless of which technique has been used.
Find out more about ACJ Reconstruction – Post-Operative & Rehabilitation protocol….
Acromioclavicular Joint Osteoarthritis (ACJ arthritis)
- Osteoarthritis (‘wear & tear’ arthritis) changes are very common in the ACJ due to the constant load that passes through it
- Osteoarthritis can be seen on MRI scans of most people over 35 years of age but it is usually asymptomatic and most people do not have any symptoms
- you only need to treat ACJ osteoarthritis when it is causing a problem
Who gets symptomatic ACJ OA?
- most of the time people who develop ACJ OA symptoms do so gradually over time
- sometimes an injury to the shoulder can ‘spark off’ symptoms
- people who do a lot of heavy manual work are more prone to developing symptoms at an earlier age
- people who have had a previous injury or fracture to their ACJ are more prone to developing symptoms
- ‘weight-lifters shoulder’ is a variant of ACJ OA
Find out more about ‘weight-lifters shoulder’….
What has happened?
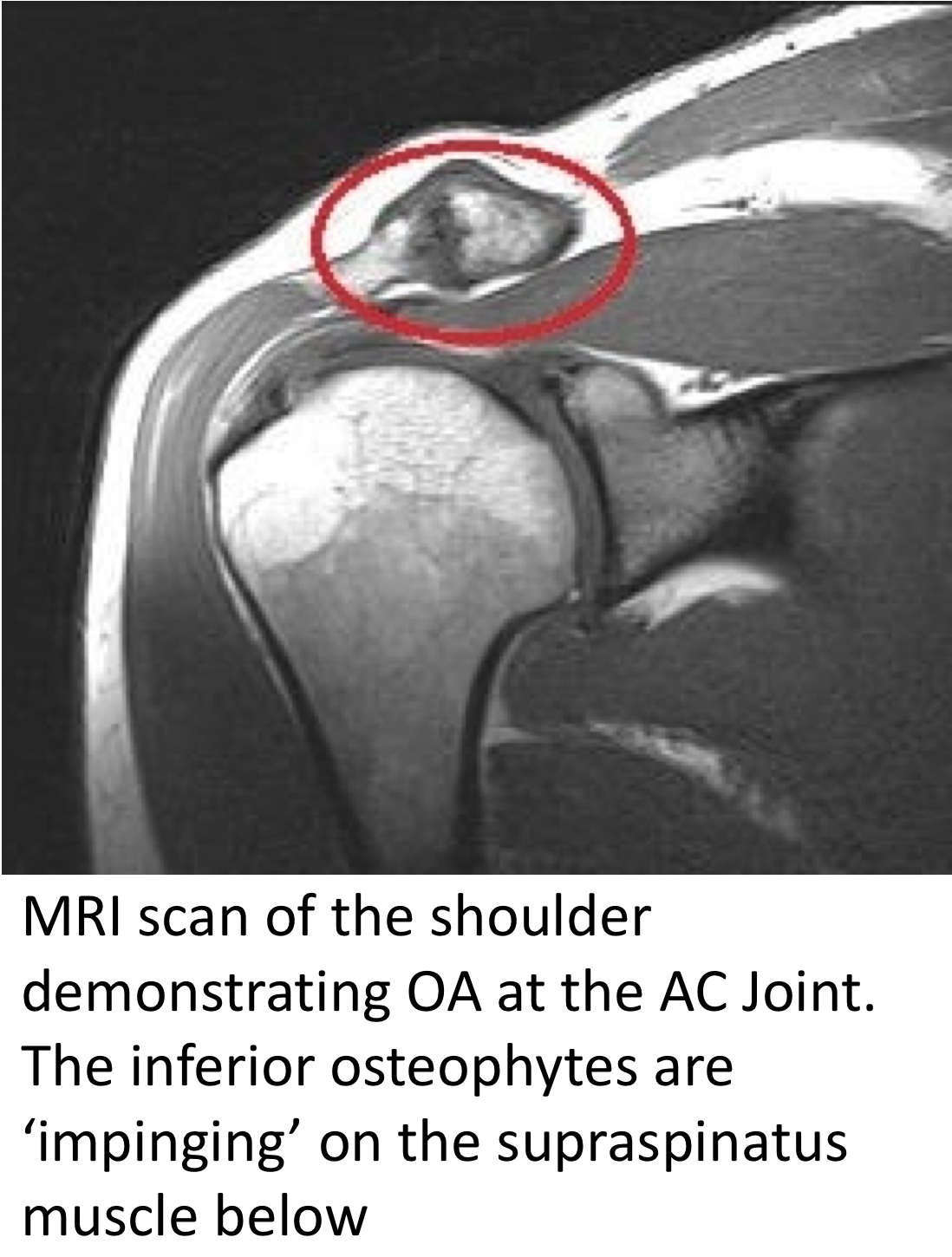
- osteoarthritis is mainly a ‘wear and tear’ process (Fig 3)
- over time the articular cartilage on the end of the clavicle and acromion degenerates and wears away
- this can lead to a collapsing of the joint and the exposed ends of the bone rubbing causing pain, stiffness and discomfort
- in response to a loss of the articular cartilage the body often produces extra bits of bone at the edge of the joint surface to help to dissipate the load, these extra bits of bone are known as Osteophytes
- the ACJ is very close to the skin and osteophytes can be responsible for the increased prominence of an ACJ with OA
- as well as the osteophytes protruding at the top and front of the joint they can also protrude inferiorly (underneath). This can lead to ‘impingement’ of the underlying Supraspinatus tendon, leading to additional rotator cuff symptoms
find out more about Supraspinatus Impingement….
What are the symptoms of ACJ OA?
- pain over and around the ACJ is the main symptom of ACJ OA
- the pain is often worse on cross-body ADduction (bringing the arm across the body at shoulder height) and towards the extreme of forward elevation
- the ACJ is tender on palpation and may appear swollen & more prominent than the opposite side (a combination of inflammation and osteophyte formation)
- some people can have associated rotator cuff symptoms
find out more about Rotator Cuff problems….
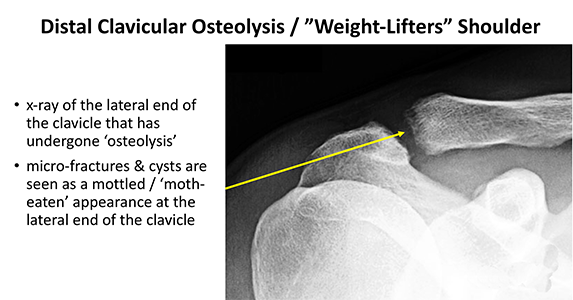
Distal Clavicular Osteolysis (“weight lifter’s shoulder”, ACJ Osteolysis)
- Distal Clavicular Osteolysis or ACJ Osteolysis / ‘weight lifter’s shoulder’ is a very similar condition to ACJ Osteoarthritis and presents in a similar way
- it is an ‘overuse’ phenomenon that causes multiple tiny fractures to the distal end of the clavicle which leads to a breakdown of the bone (osteolysis)
- it presents with identical symptoms to ACJ Osteoarthritis
- it not only occurs in weight lifters but can also affect younger people who are taking a lot of load through their shoulders (rowers, hand-ball players, builders, soldiers etc)
- the diagnosis, treatment and management of Distal Clavicular Osteolysis is the same as that for ACJ Osteoarthrits (Fig 4)
How do you diagnose & treat Acromioclavicular Osteoarthritis
To diagnose & treat Acromioclavicular Osteoarthritis, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. The best treatment for someone with ACJ OA can depend on the severity of their symptoms and any other associated shoulder conditions.
History
- in most cases of ACJ OA the wear and tear changes have usually been present for a number of years before the symptoms appear
- symptoms usually come on gradually over time but, in certain cases, a specific injury or incident may precipitate the onset of symptoms
- Rotator Cuff problems are very commonly associated with ACJ OA and a patient may also have additional Rotator Cuff type symptoms
- the ACJ is often swollen and tender to touch
- patients may experience pain over the ACJ when reaching across themselves or reaching up for a high object
Examination
- on inspection some patients have a markedly swollen and enlarged ACJ on the affected side
- the joint is often painful on palpation
- most patients with isolated ACJ OA normally have a full range of motion with occasional discomfort at the top of elevation
- as ACJ OA is often associated with Rotator Cuff problems patients may have an additional limitation or pain on movement with some weakness
- the Scarf Test or Cross-Body ADduction Test involves wrapping the patients affected arm over the front of their body at shoulder height (similar to wrapping a Scarf around the neck). This puts a direct load across the ACJ and is often painful
find out more about examination of the shoulder …..
Investigations
- X-Ray – a plain, good quality AP & Axillary x-ray of the shoulder will normally demonstrate the presence of ACJ OA
- the characteristic findings are of loss/collapse of the joint space, scelorsis (thickening of the bone), bone cysts & osteophytes
- osteophytes are boney protrusions at the edge of the joint and can be present both on the top and the bottom of the joint
- inferior osteophytes (at the bottom) can sometimes protrude significantly and lead to impingement of the underlying rotator cuff tendons (supraspinatus tendon)
Find out more about X-Rays of the shoulder ….
- MRI Scan – an MRI scan is a very sensitive investigation for ACJ OA and can show early signs of OA before they can be picked up on an x-ray
- the benefit of an MRI scan is that it can also demonstrate the soft-tissue structures around the ACJ and in particular the rotator cuff tendons
Find out more about MRI scans of the shoulder…..
- the benefit of an MRI scan is that it can also demonstrate the soft-tissue structures around the ACJ and in particular the rotator cuff tendons
Treatment for Acromioclavicular Osteoarthritis
- there are a number of treatments for symptomatic ACJ OA
- the most appropriate treatment for a particular patient depends on a number of factors including severity, other co-existing shoulder problems & the expectations and requirements of a particular patient
Analgesia/Pain Relief
- pain is one of the major problems associated with a ACJ OA
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
Physiotherapy
- physiotherapy can be very helpful in ACJ OA, particularly in the recovery phase once the pain is under control
- the main aim of physiotherapy is to improve the general function and movement of the shoulder, and particularly the Rotator Cuff function
Find out more about Shoulder Physiotherapy….
Cortisone Injection
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the ACJ it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- it can usually be injected simply in the Out-Patient Clinic or under Ultrasound Guidance
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Surgery for Acromioclavicular Joint Osteoarthritis
- some cases of ACJ OA can be resistant to non-operative treatment and continue to cause significant problems
- in other situations, ACJ OA can be contributing to on-going Rotator Cuff problems that require surgical intervention
- in these cases, surgical excision of the ACJ is a relatively simple and very successful procedure with a quick recovery time
- an ACJ excision can be done as an Open or Arthroscopic procedure. I prefer to undertake an arthroscopic procedure as it allows for a far more rapid recovery
Surgery for Arthritis
Surgery for Acromioclavicular Joint Osteoarthritis
- some cases of ACJ OA can be resistant to non-operative treatment and continue to cause significant problems
- in other situations, ACJ OA can be contributing to on-going Rotator Cuff problems that require surgical intervention
- in these cases, surgical excision of the ACJ is a relatively simple and very successful procedure with a quick recovery time
- an ACJ excision can be done as an Open or Arthroscopic procedure. I prefer to undertake an arthroscopic procedure as it allows for a far more rapid recovery
Arthroscopic Acromioclavicular Joint Excision
-(ACJ Excision, ACJ Excision arthroplasty)
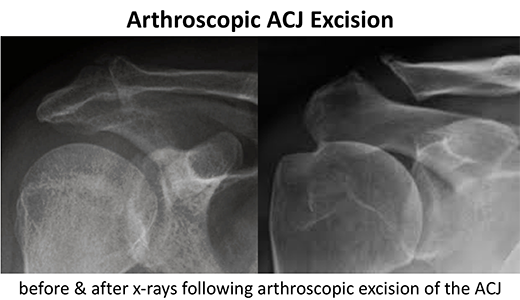
An isolated Arthroscopic Acromioclavicular Joint Excision can usually be done as a Day-Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. When an ACJ Excision is done as part of another procedure (i.e. Arthroscopic Rotator Cuff repair) the post-operative immobilization and recovery may be dictated by the that procedure.
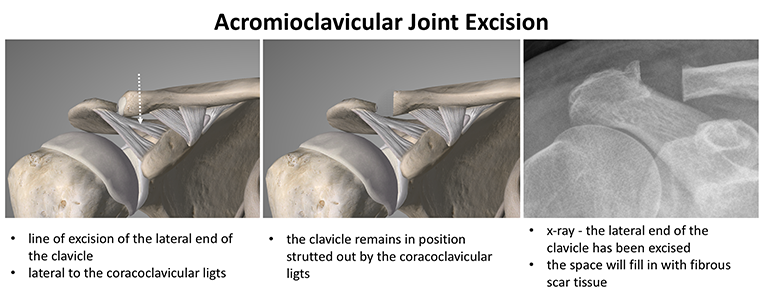
ACJ is in a unique position in that the acromion and clavicle are both held in a stable position. The corococlavicular ligaments hold the clavicle in a stable position, so that removing the outer 1cm of the clavicle and articular surface just leaves a gap without the clavicle collapsing into it. This gap fills up with fibrous scar tissue resulting in a pain free ‘pseudo’ joint. After the surgery the shoulder is kept as mobile as possible to prevent stiffness.
The procedure is undertaken using a general anaesthetic and an interscaelane nerve block. After the procedure the Physiotherapists take the patient through a set of rehabilitation exercises to help maintain range of motion and to regain strength. My routine Arthroscopic Acromioclavicular Excision Procedure is described below,
Watch a video of an arthroscopic ASD & Acromioclavicular Joint Excisison….
-
- the patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
- the patient is anaesthetised with a general anaesthetic and interscaelane nerve block
- a posterior, lateral and anterior portal are used to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- the Glenohumeral Joint is initially assessed to look for any other problems that might be associated with a ACJ Osteoarthritis and, in particular, the Rotator Cuff and the Long Head of Biceps
- the Subacromial Space is then entered and the undersurface of the Acromion identified.
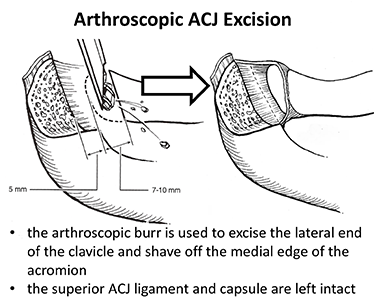
- using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the undersurface of the acromion and the degenerate ACJ
- a powered burr is then used to resect about 5mm of bone from the undersurface of the acromion to allow better access to the ACJ
- viewing from the lateral portal the distal end of the clavicle and the degenerate ACJ are viewed
- using a combination of a powered shaver and radiofrequency probe the ACJ is exposed paying careful attention to preserve the superior and posterior AC capsular ligaments
- using a powered burr the distal 10mm of the clavicle is excised and the medial end of the acromion flattened, it is very important that the resection is not taken to medially to avoid compromising the coracoclavicular ligaments (Fig7)
- at the end of the procedure the resection is assessed and the Rotator Cuff is examined to check for any hidden fraying or damage
- the Subacromial Space and Distal Clavicle are then washed out and the wounds closed with sub-cuticular sutures
Find out more about having an operation…
After the Surgery
Post-Operative Care
Following an Open Acromioclavicular Joint Reconstruction, the patient requires a check x-ray and maybe able to go home on the same day as their surgery or may need to stay in the hospital over-night. This decision would depend on various associated factors.
I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves off of using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic ACJ Excision is usually a very successful procedure but, because the surgery is only aimed at removing the degenerate bone ends, it usually takes between 3 – 6 months for all of the symptoms to settle down.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system …..