What is Shoulder Instability?
Shoulder Instability is a general term for any type of problem that results in the Humeral Head (Ball) not being centred firmly into the glenoid (Socket). It can range from,
-
Dislocation - complete dislocation of the head
-
Subluxation - an incomplete dislocation where the Humeral Head slips to the edge of the Glenoid socket and almost dislocates, but is ‘caught’ just before this happens.
-
Micro-Instability – A situation where the Humeral Head does not feel completely stable in certain positions of movement.
Shoulder Stabilisers
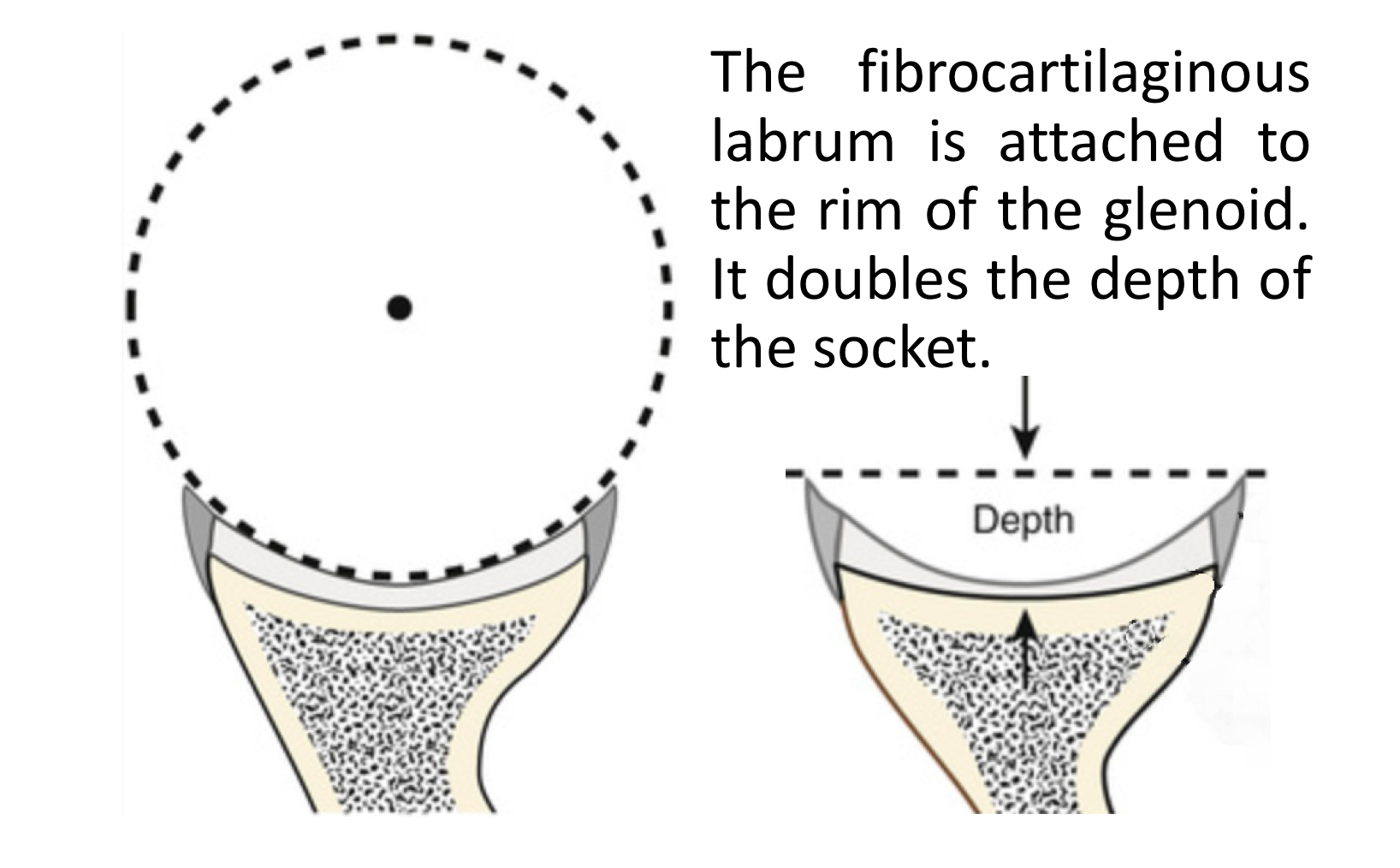
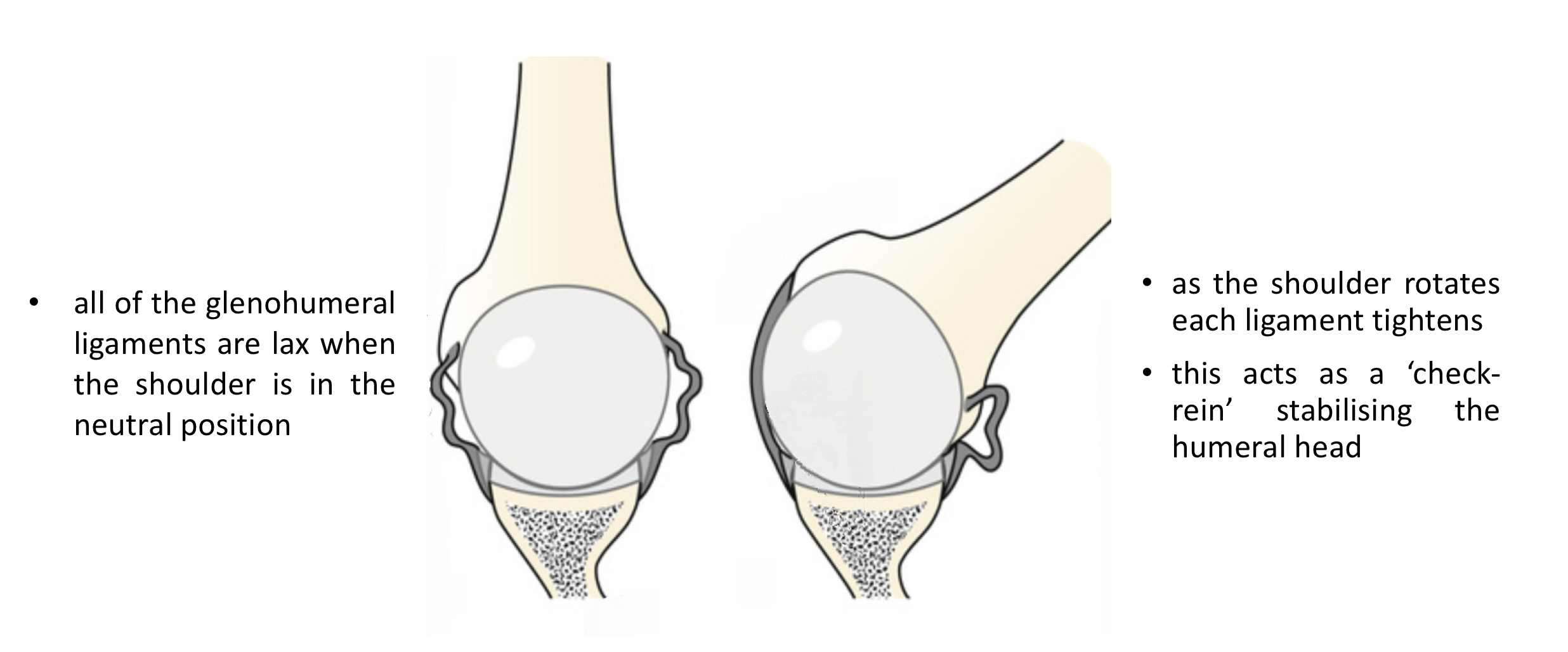
The shoulder is the most mobile joint in the body with a relatively small socket (gelnoid) and large head (humeral head). This configuration means that it is potentially unstable and it is the most frequently dislocated joint in the body. Fortunately, this still occurs relatively rarely and is because there are a number of mechanisms that help to keep it in joint. These are divided into 2 groups,
-
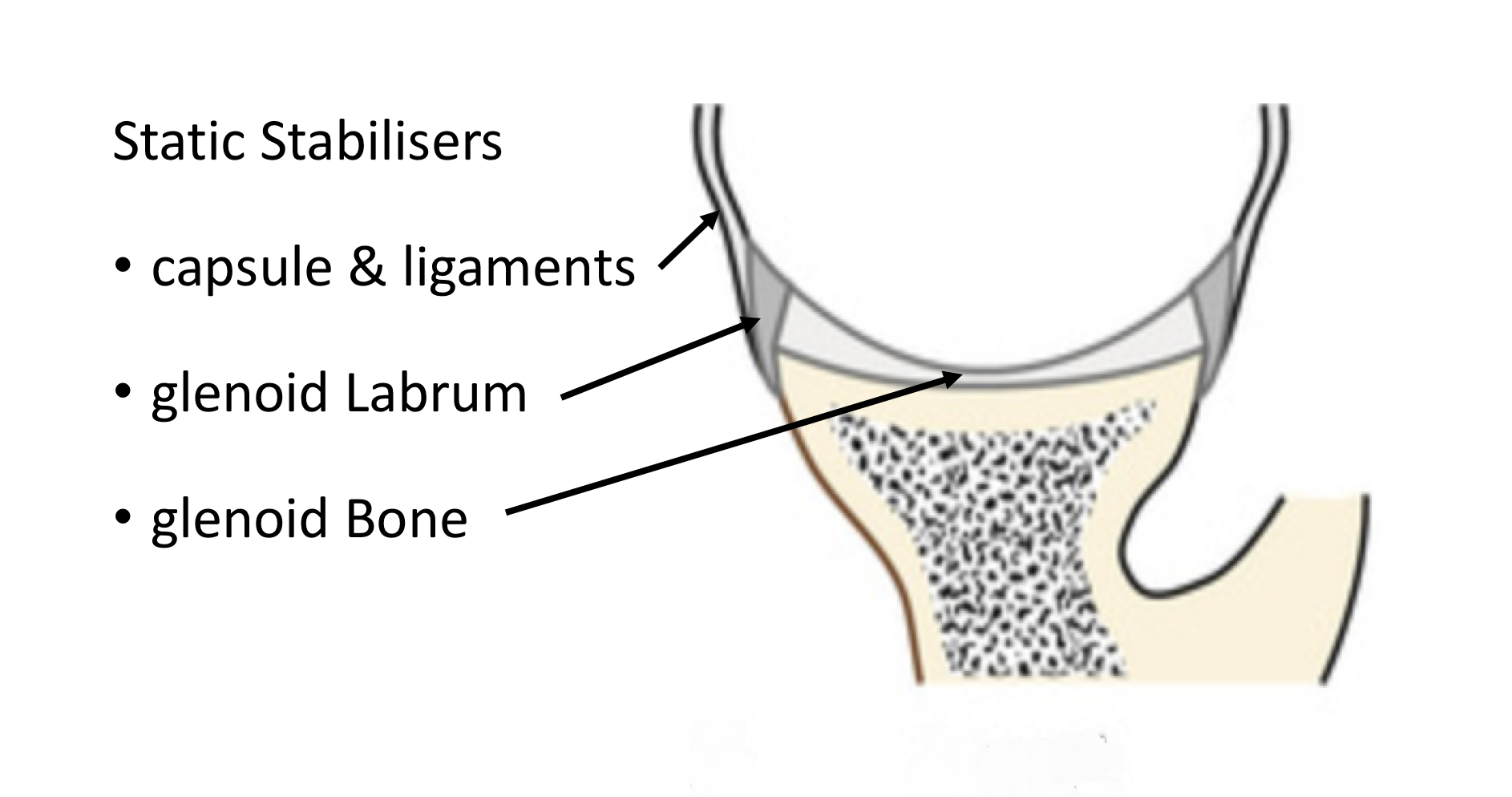
Static Stabilisers – these are the socket (glenoid) with its convex shape, the glenoid labrum (that deepens the socket) and the ligaments that connect the ball to the socket.
-
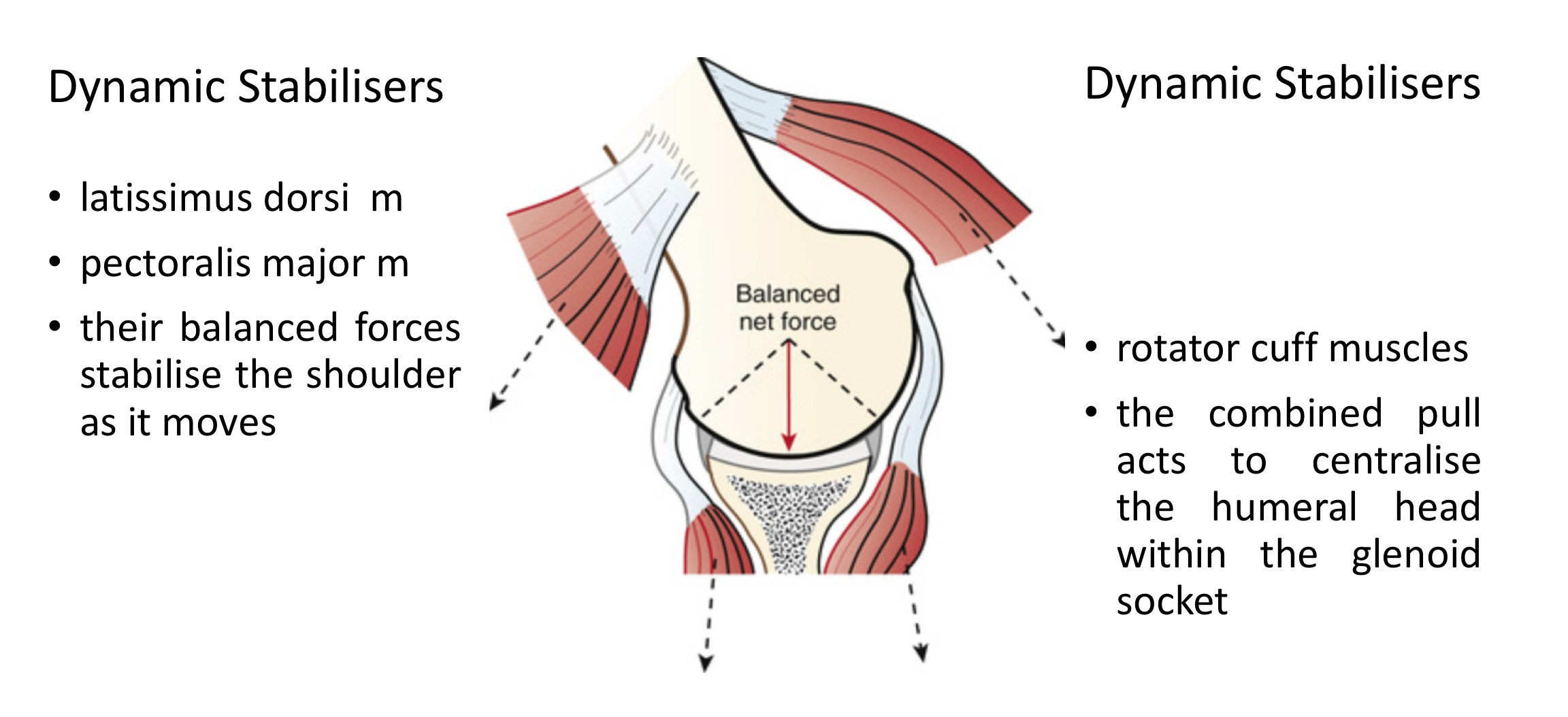
Dynamic Stabilisers – these are the multiple groups of muscles that surround the shoulder girdle and work in a complex rhythm to move the shoulder whilst keeping it in joint.
Find out more about the Anatomy of the Shoulder…
Types of Dislocations
This section covers shoulder dislocations. Labral Tears/SLAP tears cause a specific type of instability which is covered in its own section.
Find out more about SLAP tears....
When the shoulder dislocates or subluxes it will be due to an injury or failure of either the dynamic or static stabilisers or both. There are 3 ways in which shoulder stability fails,
-
Traumatic Injury – this is the commonest cause for shoulder dislocations. Usually the patient sustains a significant injury where they fall forwards with the arm elevated, the elbow bent and the hand facing forwards (being tackled playing rugby, falling skiing or from a horse etc). The humeral head is then forced forward tearing the ligaments at the front of the shoulder and sometimes damaging the bone at the front of the socket and the back of the head. Patients usually are unable to relocate their shoulder and need this to be done at a medical centre. Occasionally the labrum and ligaments can be damaged by repeated smaller injuries to the shoulder until they eventually fail.
-
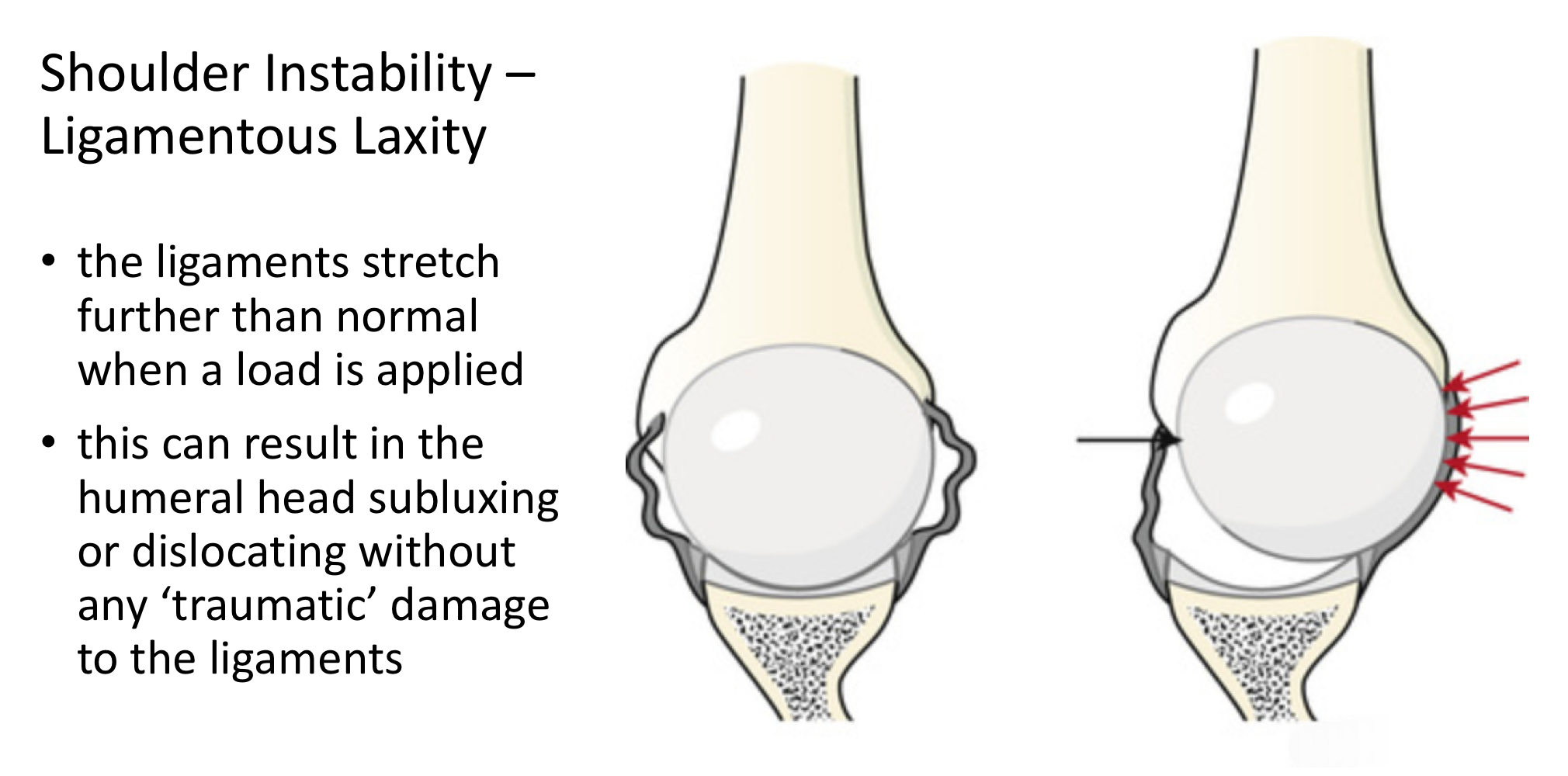
Ligamentous Laxity - some peoples’ tissues are more lax/stretchy than others. This tends to occur more often in females than males and in younger people. In certain cases the ligaments around the shoulder are so lax that they are unable to completely restrain the ball within the socket. This can result in subluxation or dislocation of the shoulder without a significant injury. When this does occur the ball can dislocate in any direction leading to mult-directional instability.
-
Muscle Patterning Disorder – occasionally the complex sequence in which the groups of muscles work to stabilise the ball into the socket as the shoulder moves become disrupted. In this situation muscles that should be contracting, relax or aren’t strong enough whilst other muscles that should be relaxing, contract. This can result in the shoulder being ‘pulled’ out of the socket by this muscle imbalance. The static stabilisers of the shoulder are often completely intact.
In some cases of shoulder instability more than one of the above problems can be going on at the same time.
Diagnosis of Shoulder Instability
Diagnosing Types of Shoulder Dislocations
As with any condition assessment begins with a history and examination of the patient.
History
-
Traumatic Dislocation -
- With traumatic dislocations a history of the exact incident, mechanism of injury, subsequent treatment and any further dislocations is important. The age of the patient at the time of their first dislocation is very significant. Studies have shown that the younger the patient at the time of first dislocation the more likely they are to go on and have further dislocations. In fact, patients under the age of 22 who participate in contact sports are almost guaranteed to have further dislocations without treatment. Patients over the age of 50 years who have a traumatic dislocation have an increasing likelihood of also damaging or tearing their rotator cuff.
- Over 90% of traumatic dislocations involve the shoulder dislocating forwards (Anterior).
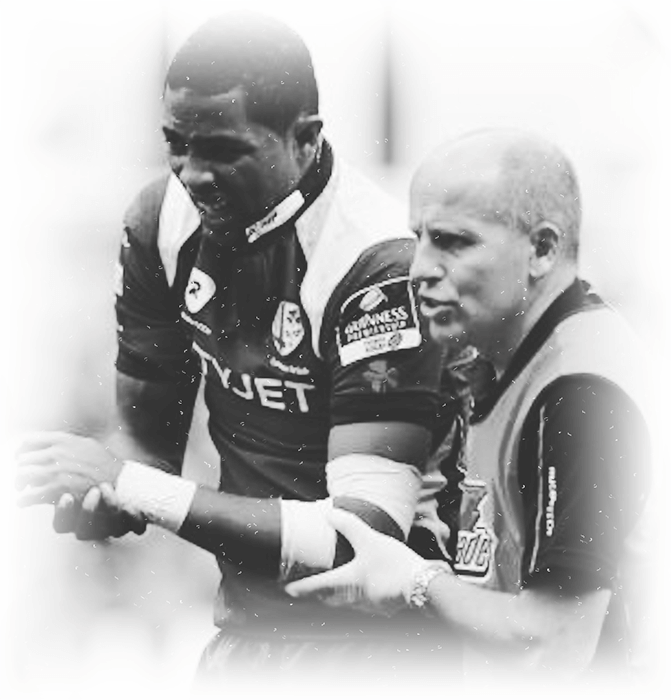
- episodes of dislocation many patients have no specific symptoms. However, in some cases, patients develop a feeling of ‘apprehension’ when they move their arm into certain positions. This is usually when the arm is ABducted and Externally rotated (arm elevated above 900 to the side with the elbow bent at 900 with the hand facing forward and the arm rotating backwards). Patients get a feeling over the front of their shoulder that it may slip out. In more severe cases patients feel that their shoulder almost slips out and they are just able to catch it. They often subconsciously adapt the way that they use their arm and avoid the position of apprehension
- Ligamentous Laxity & Muscle Patterning - Patients with ligamentous laxity or a muscle patterning problem usually have not had an initial traumatic event. Their problems tend to develop over time without a significant precipitating injury. Unlike traumatic dislocations the shoulder may be unstable in multiple directions. They may notice that their shoulder feels ‘apprehenisve’ in a number of different positions.
Patients with ligamentous laxity may also have problems with other joints. Ligamentous laxity may cause problems with the other shoulder, the knees, ankles and hips.
Examination
- It is initially important to assess for generalised ligamentous laxity for all patients with shoulder instability. The Bieghton Score is a simple assessment giving a score out of 9 for generalised joint laxity.
- As with all shoulder problems an initial general examination of both shoulders is undertaken looking for areas of pain, comparing the range of movement and for rotator cuff muscle strength.
- Special tests are then undertaken specifically to look for any instability in all directions.
Find out more about examination of the shoulder and special tests…
Investigations
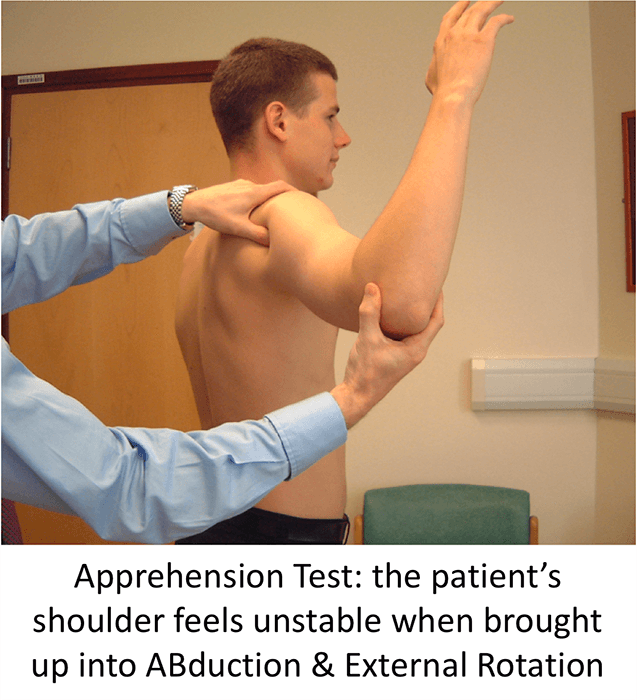
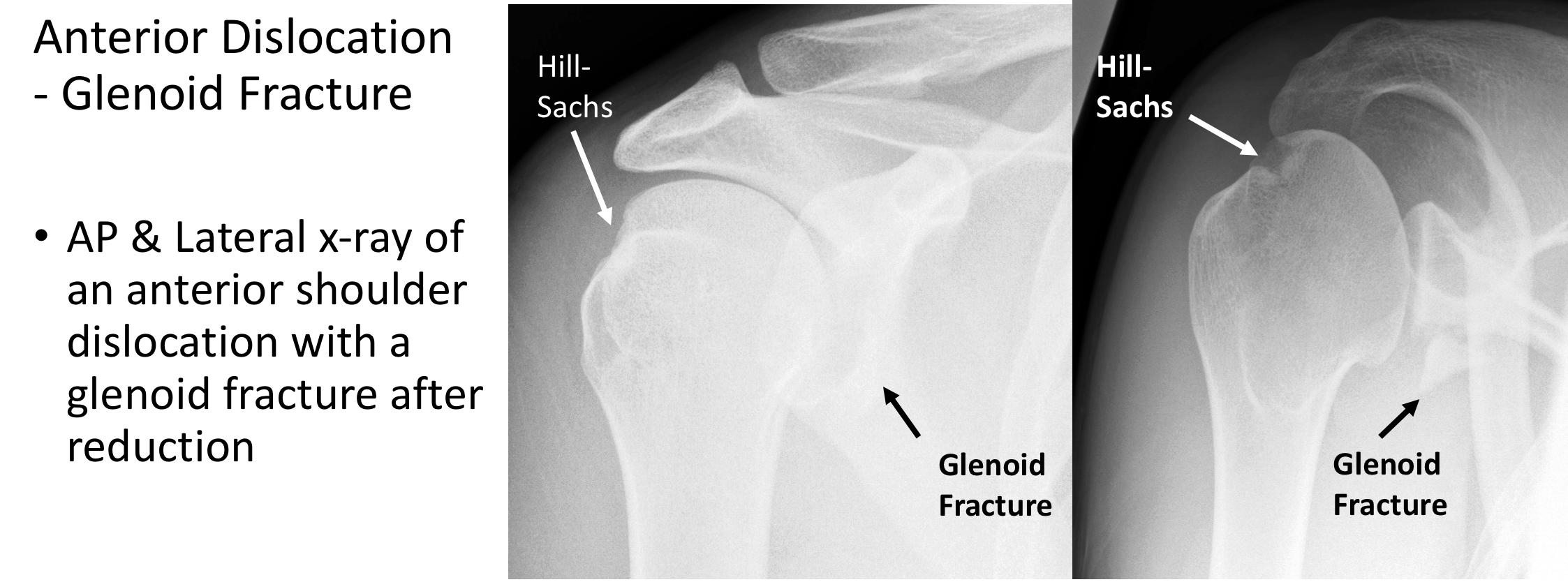
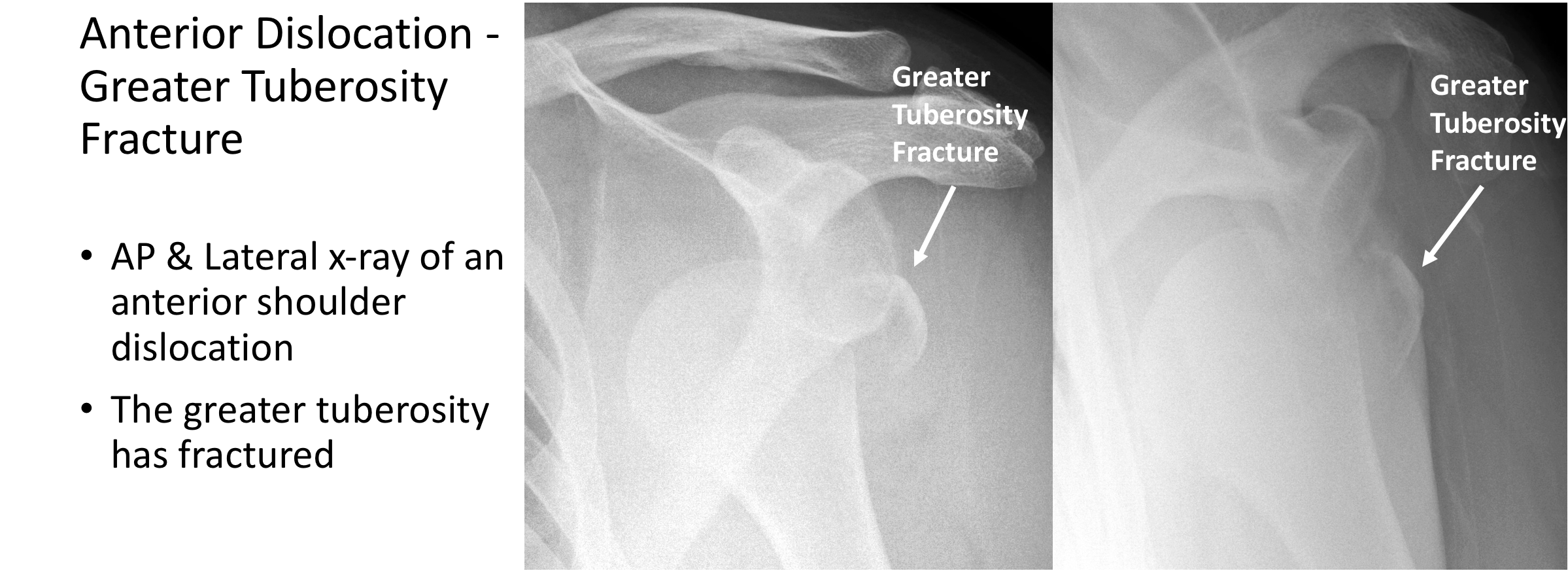
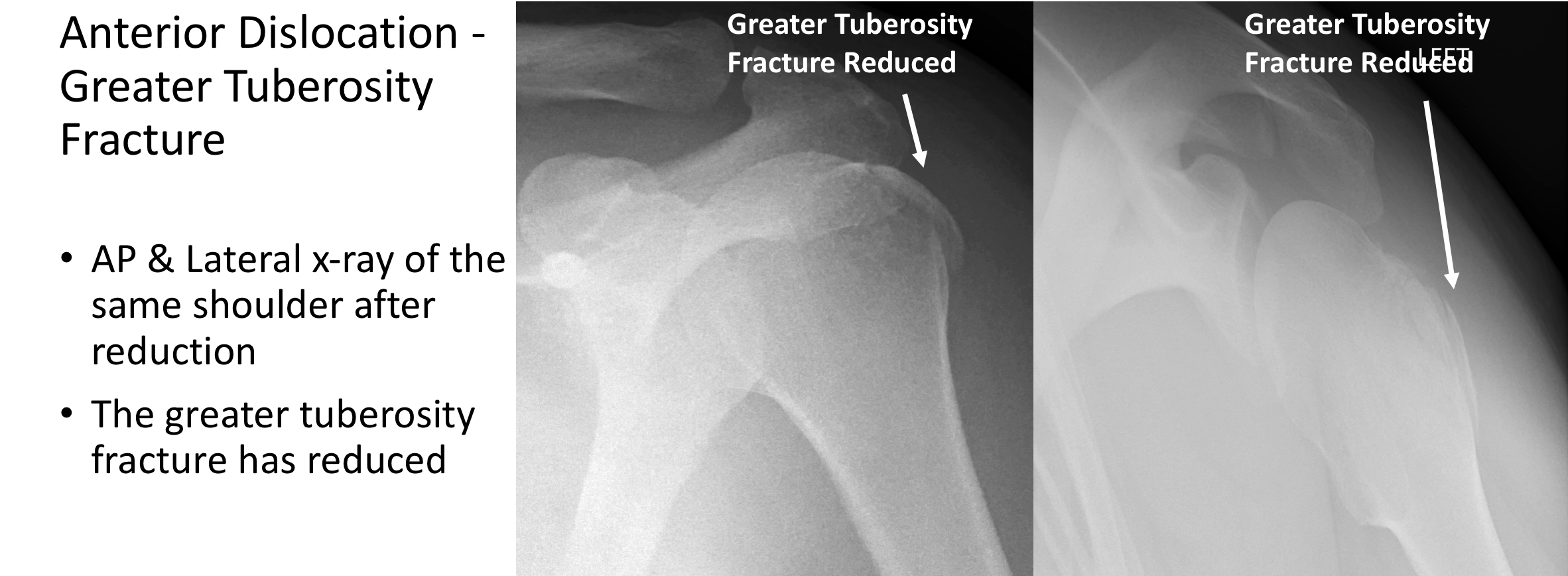
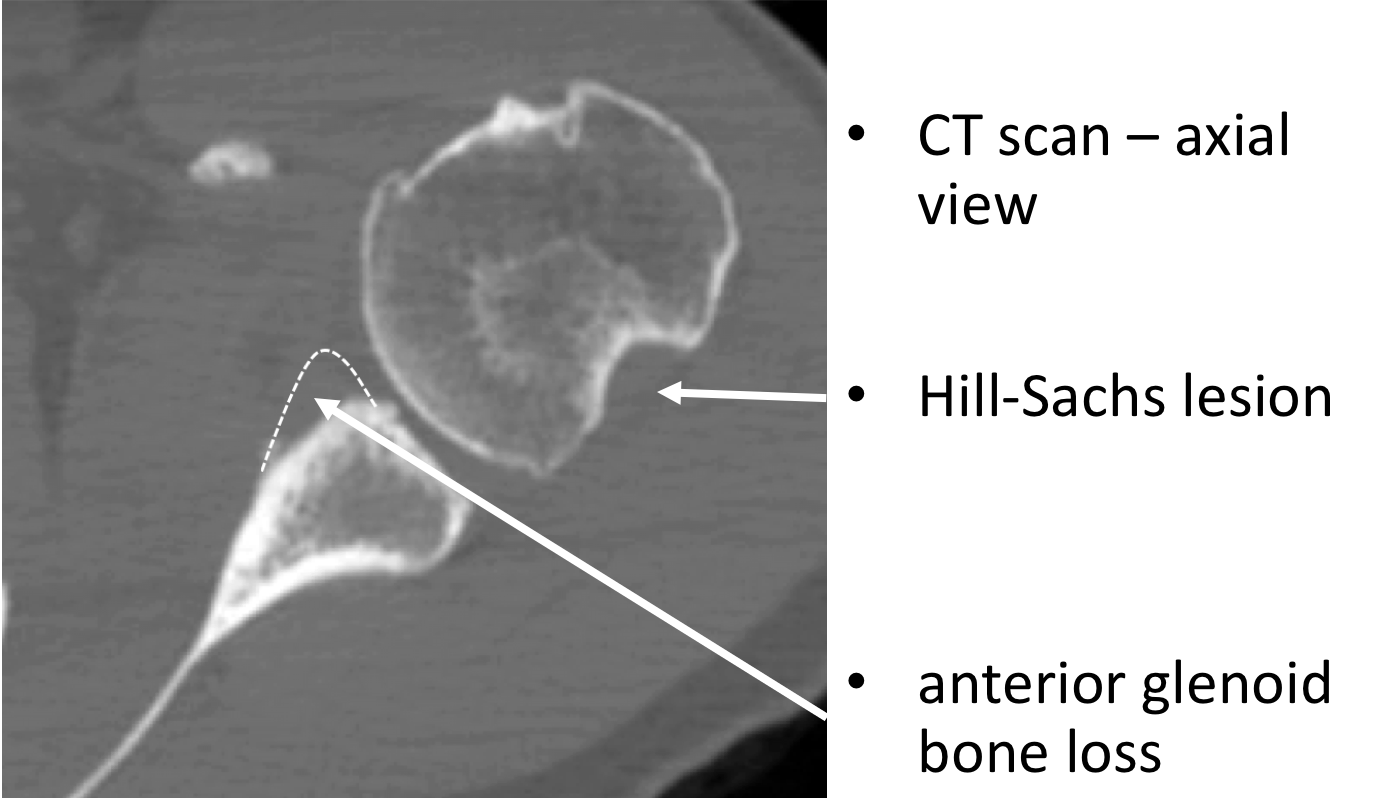
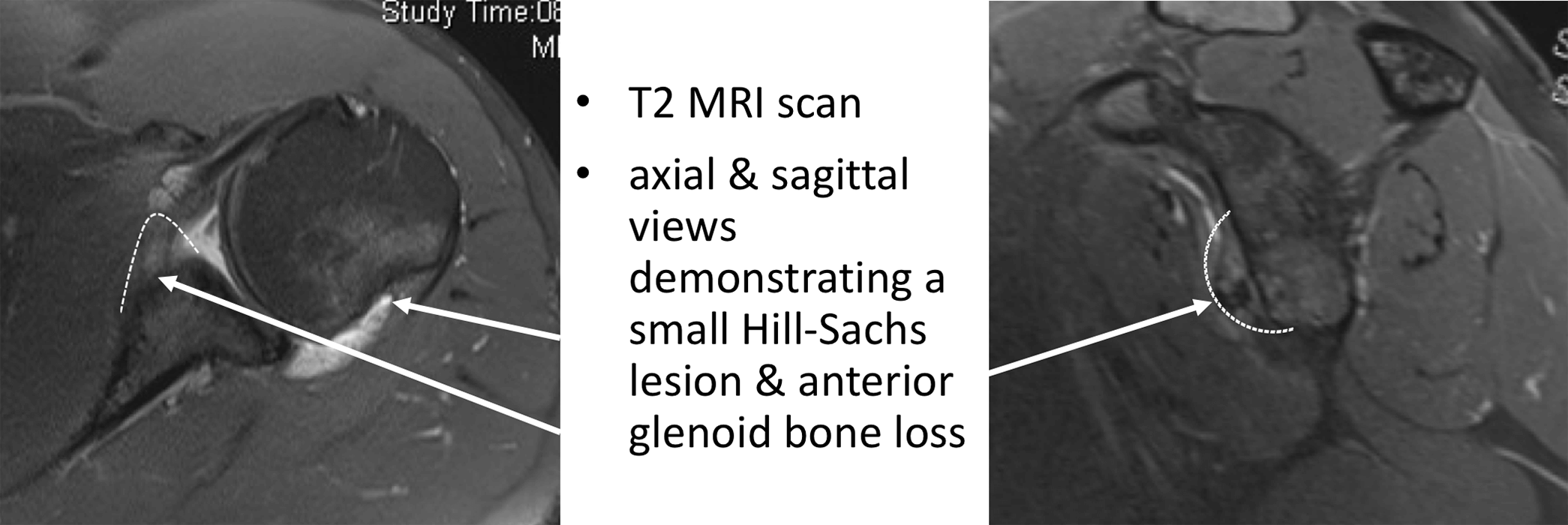
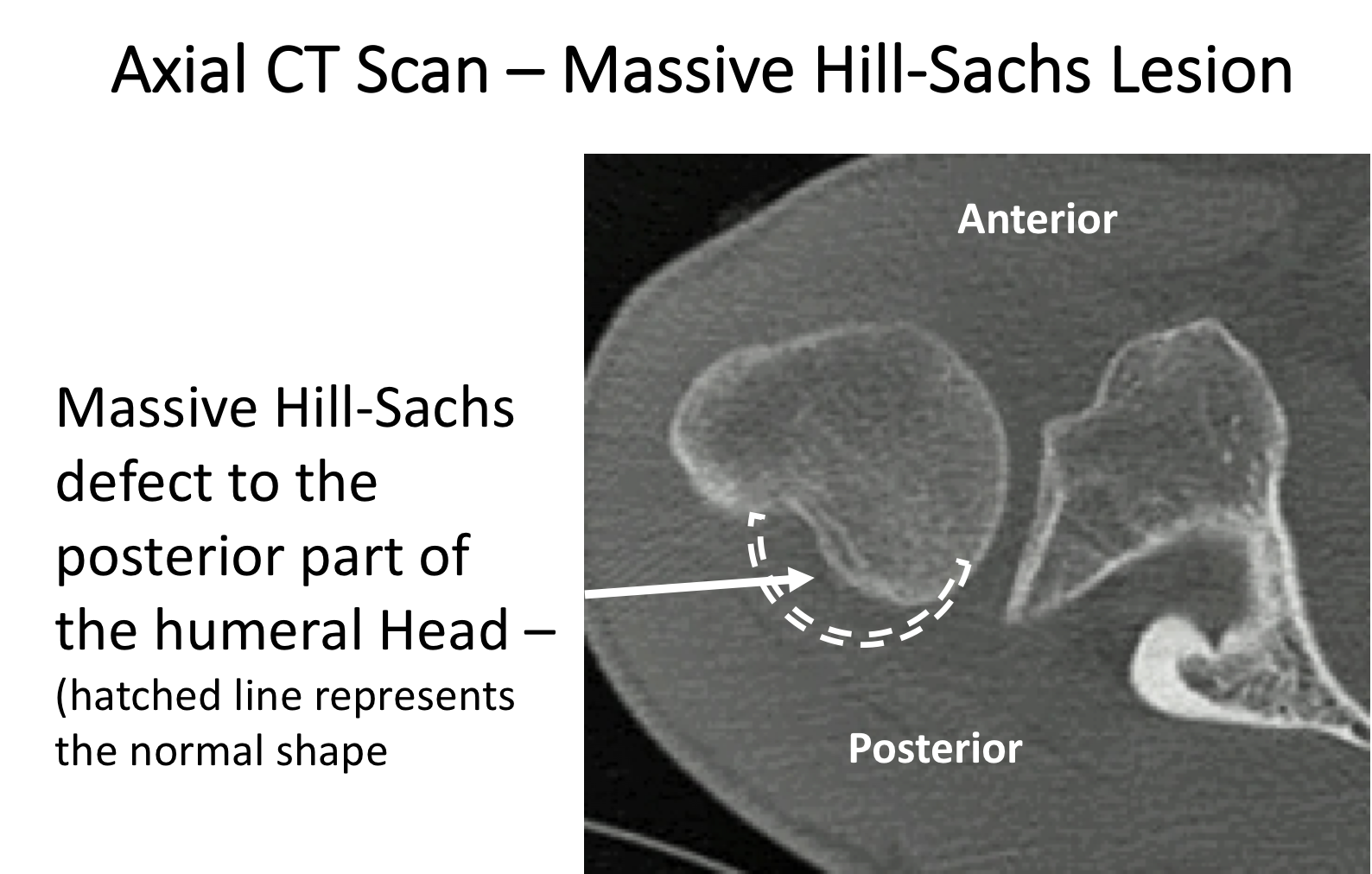
- X-Ray -Shoulder instability is usually due to a problem with the soft-tissues around the shoulder, which are not visualised on a plain x-ray. However, patients with traumatic instability and who have had multiple dislocations can often damage the bones around the shoulder. The bone at the front of the glenoid can be broken or chipped as the humeral head is impacted onto it when the shoulder dislocates. The back of the humeral head can also be dented at the same time, creating a Hill-Sachs lesion. This damage can sometimes be seen on x-rays taken at a special angle.
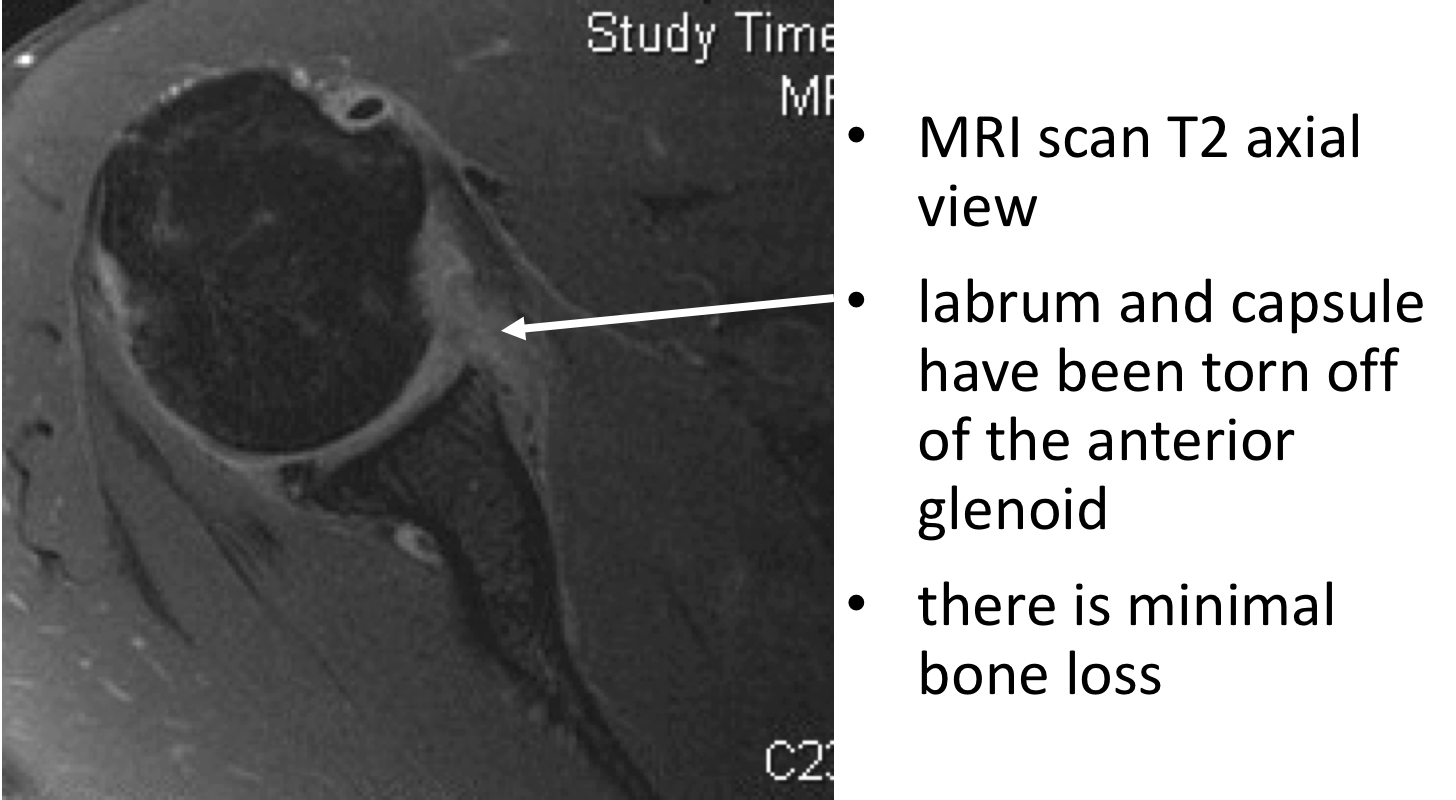
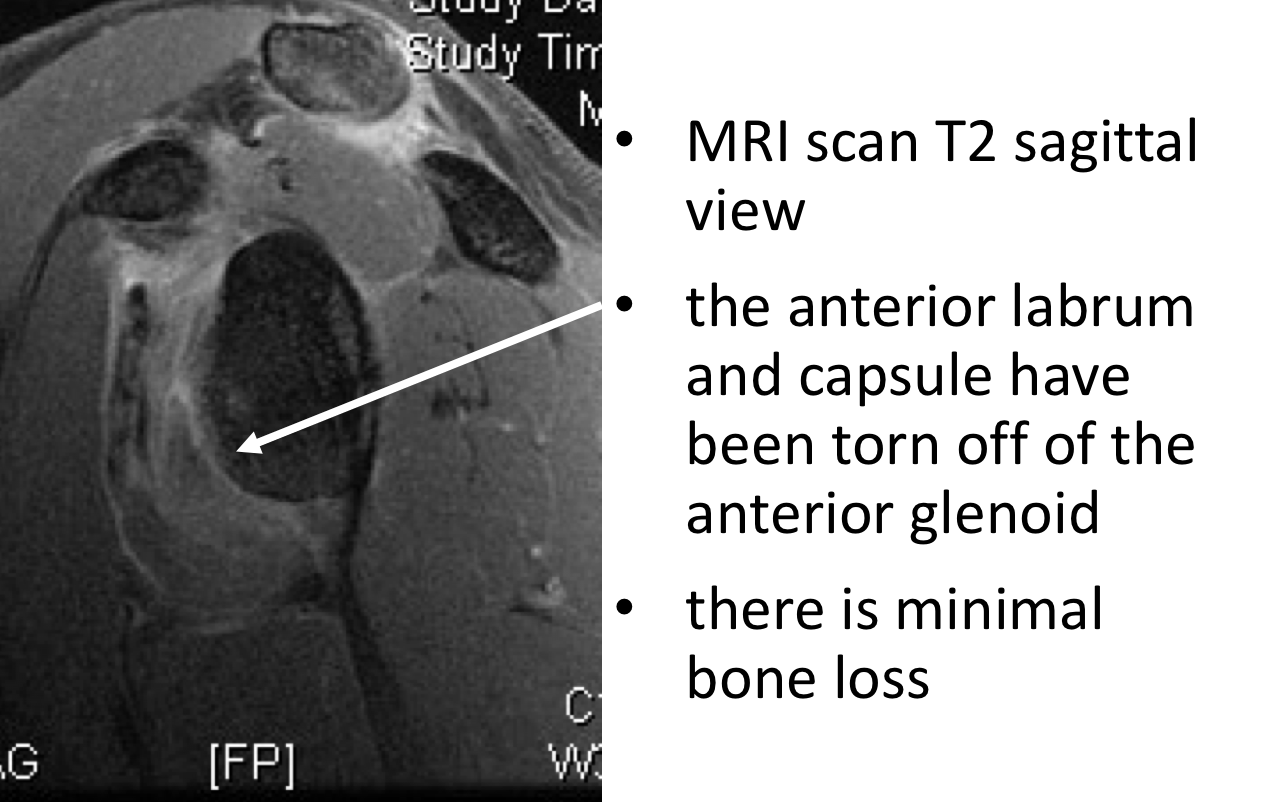
- MRI Scan – This is the best investigation to assess for shoulder instability. MRI scans are usually undertaken with the patient’s arm lying across their body. In this position the soft-tissue structures are under no strain and there is a possibility that the damaged capsule, ligaments or labrum happen to lie in the correct position and appear to be normal on the scan. To try and avoid this situation and enhance the sensitivity of the MRI scan a special ‘dye’ (Gadolinium) can be used. This can either be injected into the patient’s blood system via their arm (Indirect Arthrogram) or injected, under local anaesthetic, directly into the patient’s shoulder (Direct Arthrogram).
An MRI Arthrogram is a very good investigation to assess any damage to the labrum, capsule and ligaments of the shoulder and can also demonstrate any significant damage to the bones.
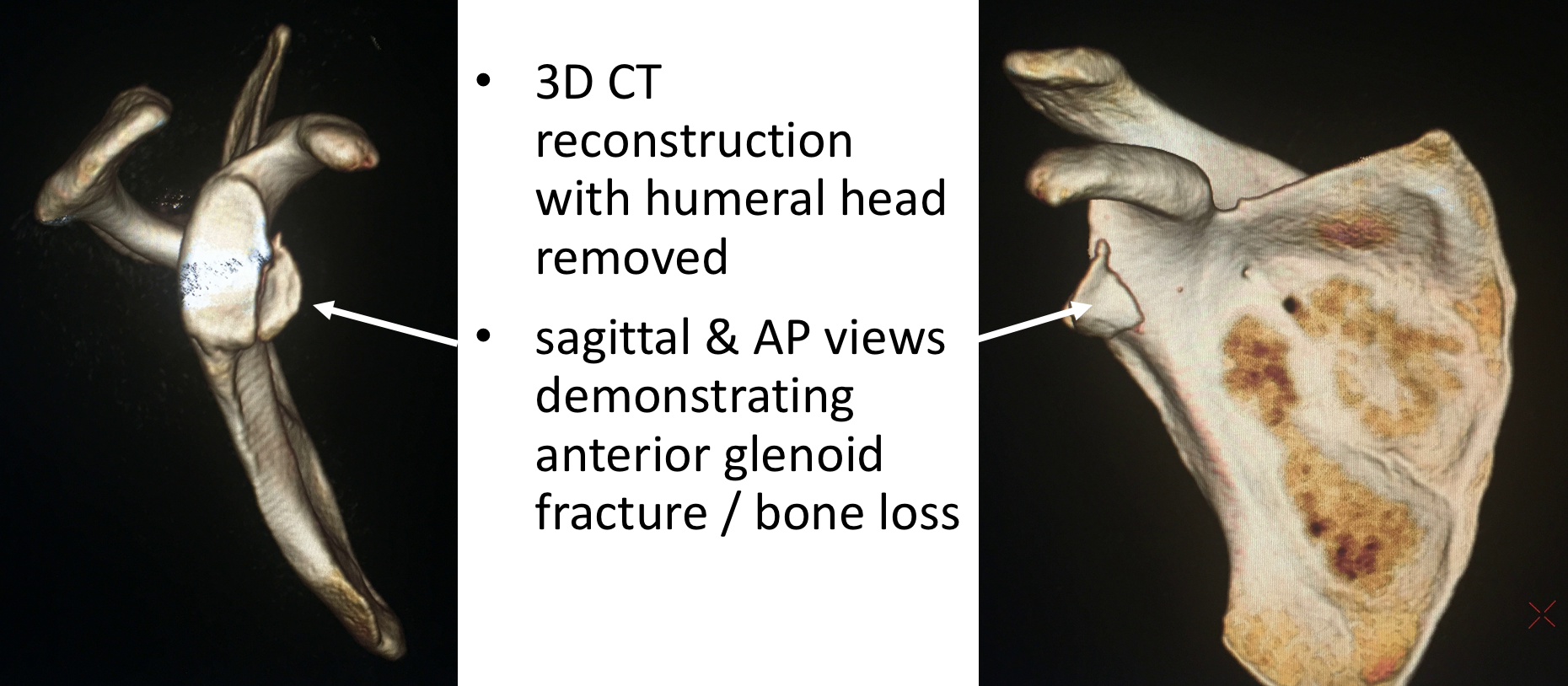
- CT Scan – A CT scan is a very good investigation to assess damage or injury to the bones around the shoulder. It is able to give 3-D images of the humeral head and glenoid. This can be very helpful where there is any concern about significant bone damage. It can then provide important information when deciding the best type of surgical treatment that might be required.
Treatment of Instability
Treatment of Shoulder Dislocations
This most important factor that determines how to best treat someone with a shoulder dislocation is whether it is due to a Traumatic Dislocation or Ligamentous Laxity/Muscle Patterning. Someone with a symptomatic Traumatic Dislocation will usually require some form of surgical repair and someone with Ligamentous Laxity or Muscle Patterning can usually be treated with a specialised rehabilitation programme supervised by a suitably experienced physiotherapist.
Management of Traumatic Anterior Shoulder Instability
What has happened?
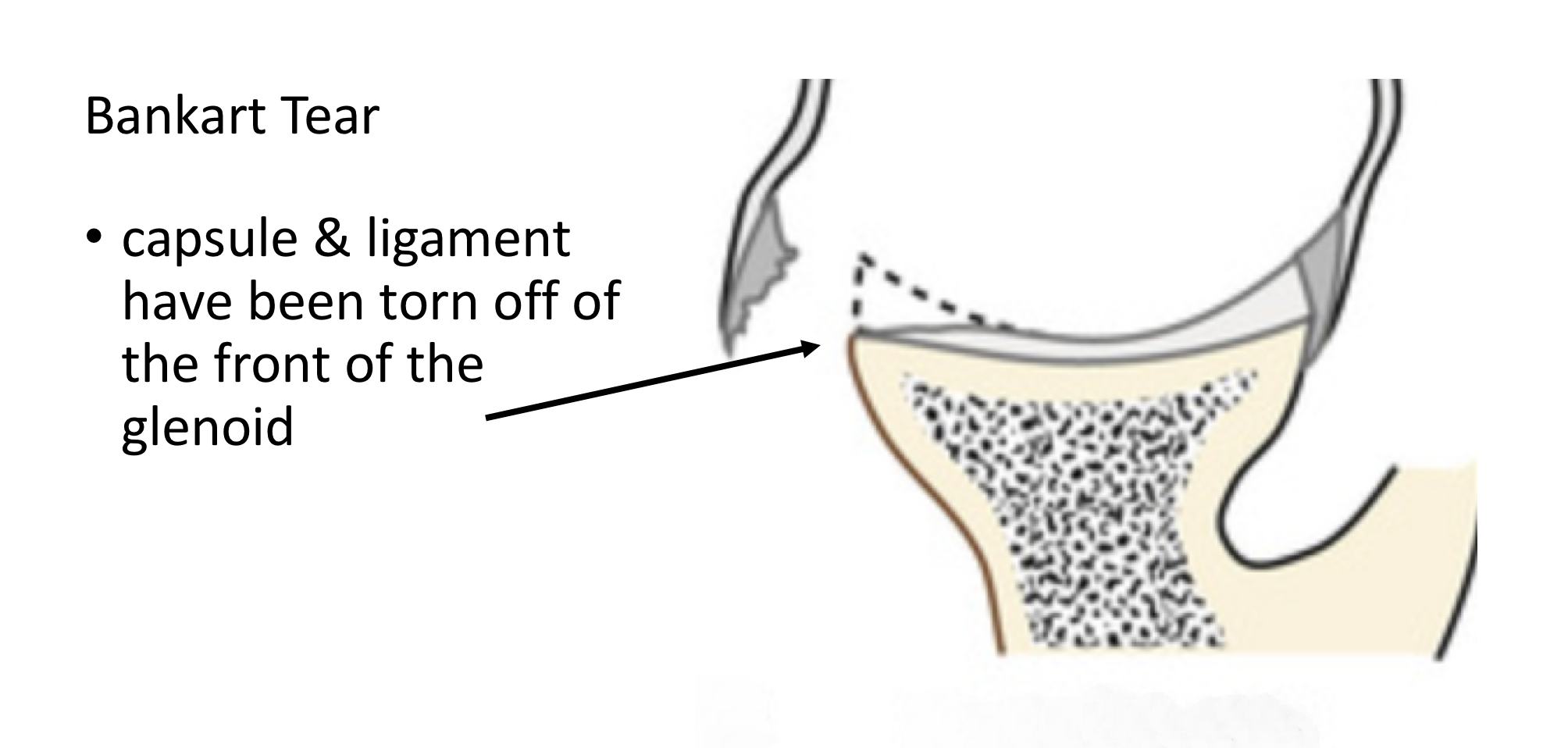
When the shoulder sustains a traumatic dislocation the ligaments and capsule at the front, lower half of the joint are usually torn away from their insertion onto the front of the Glenoid (socket). Sometimes, rather than the ligaments tearing off, a small piece of bone where the ligaments attach breaks off instead. This is known as a Bankart Tear.
Due to the constant traction on the torn ligaments and capsule and also the synovial fluid within the joint, that can inhibit healing, a Bankart Tear does NOT usually heal. As a result, there will always be a vulnerability to further instability and dislocations when the arm is elevated with the hand reaching back (ABduction& External Rotation), putting a load on the damaged area. This is sometimes known as ‘The Position of Instability’.
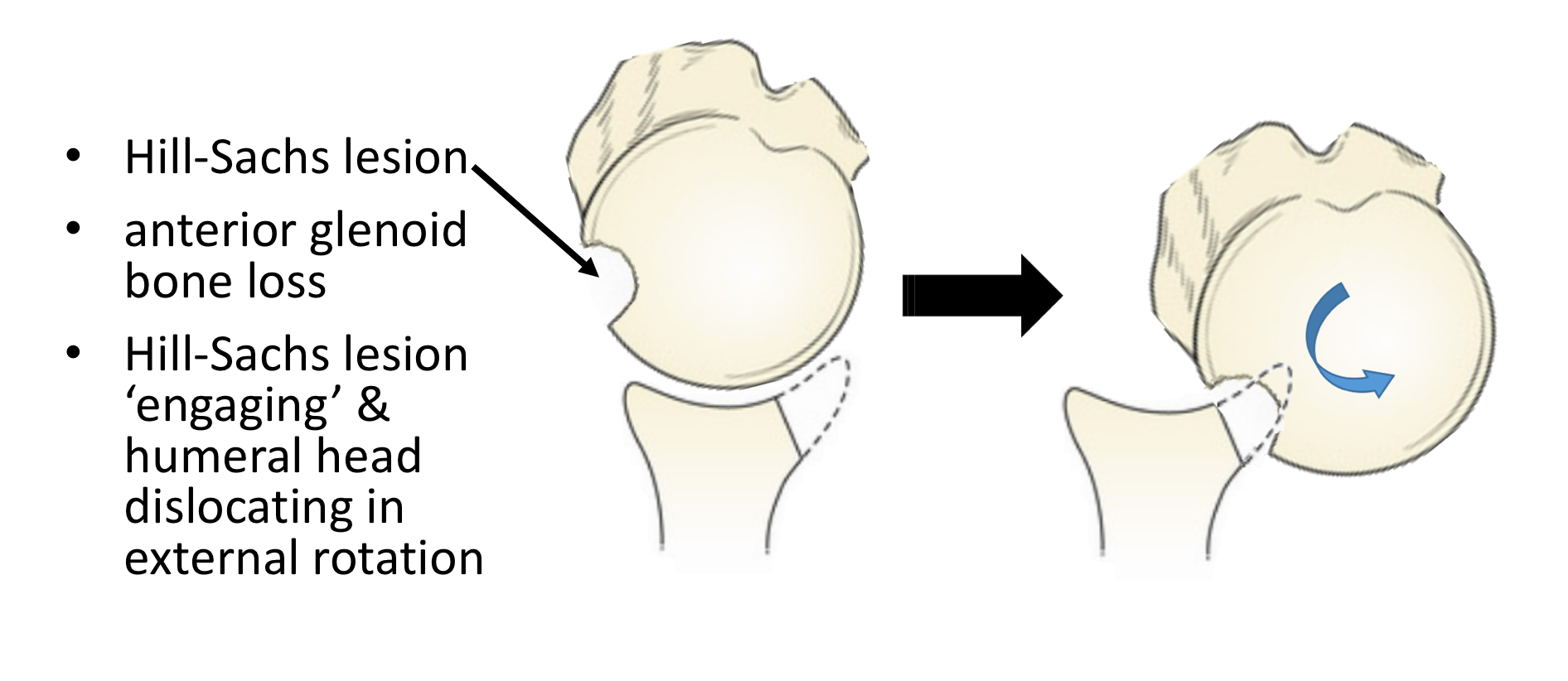
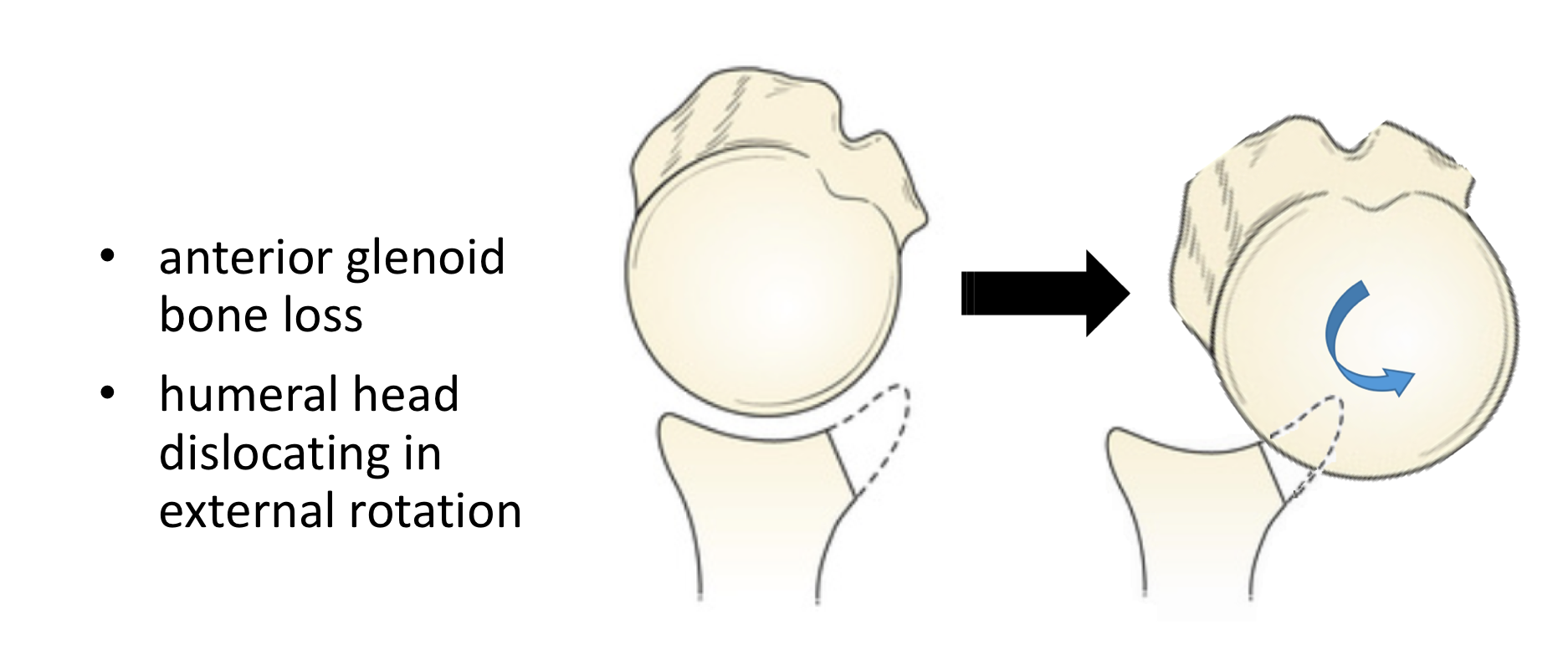
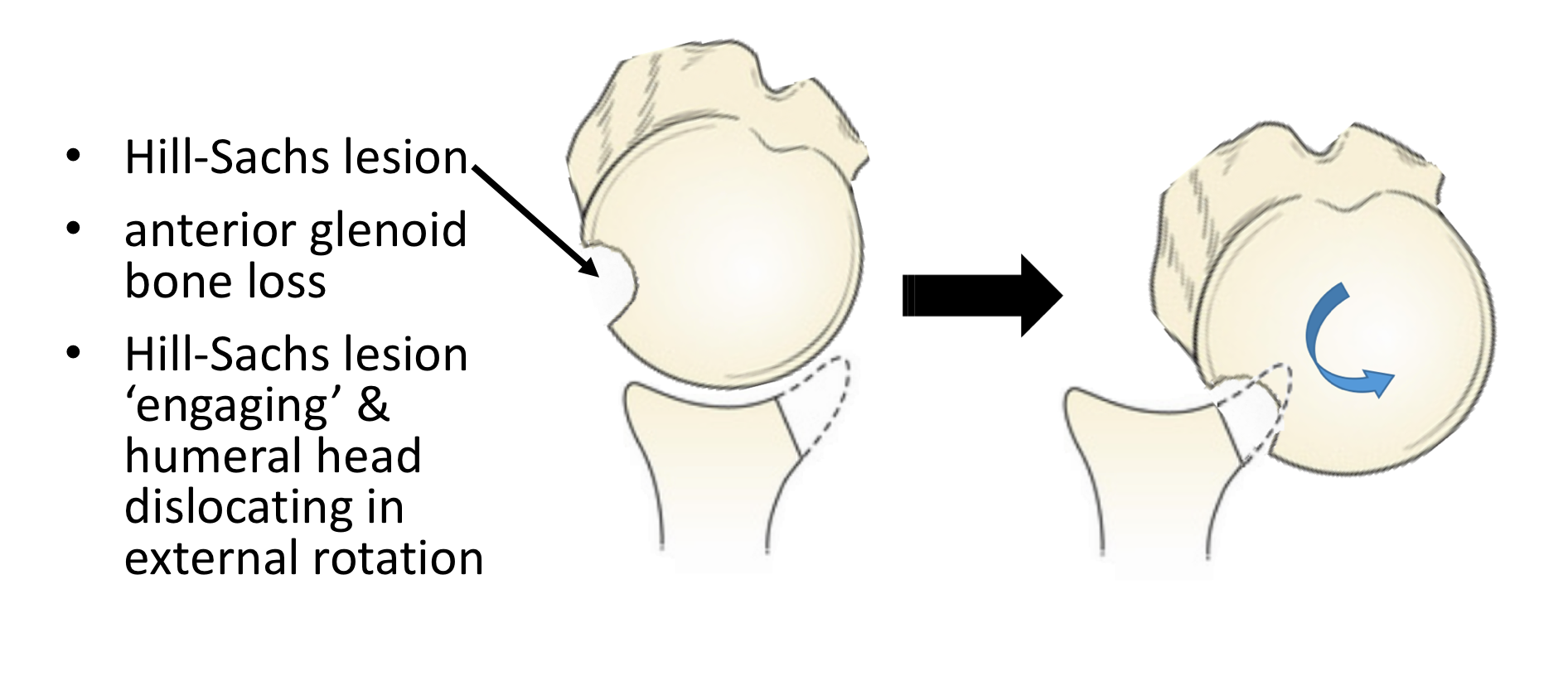
In certain cases, where the initial dislocation was due to a major force or after multiple dislocations, additional damage can also occur to the bone on back of the Humeral Head (Ball) and/or the Glenoid (Socket). When the back of the Humeral Head impacts the front edge of the Glenoid, as the shoulder dislocates, an ‘Impaction Fracture’ can occur. This creates a permanent divot in the back of the Humeral Head. At the same time the front of the Glenoid can also undergo a fracture resulting in bone loss. When these bone losses are small it is still possible to stabilise the shoulder by repairing the ligaments and capsule only. However, in certain situations where there is a significant bone loss, a different procedure may be required to address the bone loss.
Treatment for Traumatic Anterior Shoulder Instability
Not everyone who has sustained a traumatic shoulder dislocation requires an operation. Studies have shown that the older someone is when they sustain their first traumatic dislocation, the less likely that there are going to sustain a further dislocation over time. However, the younger someone is when they first dislocate their shoulder and if they are involved in overhead or contact sports the more likely they will have a further dislocation. In fact, anyone under the age of 22 years who returns to overhead or contact sports has an almost 100% chance of a further dislocation.
Once someone has had a second dislocation, and has become a ‘Recurrent Dislocator’, the likelihood is that they will continue to have further dislocations over time.
Anterior Instability
Surgery for Traumatic Anterior Shoulder Instability
The best operation for someone who has had a traumatic anterior dislocation with a Bankart tear is an Anatomic Repair of the torn ligaments and capsule. This is sometimes known as a Bankart Repair.
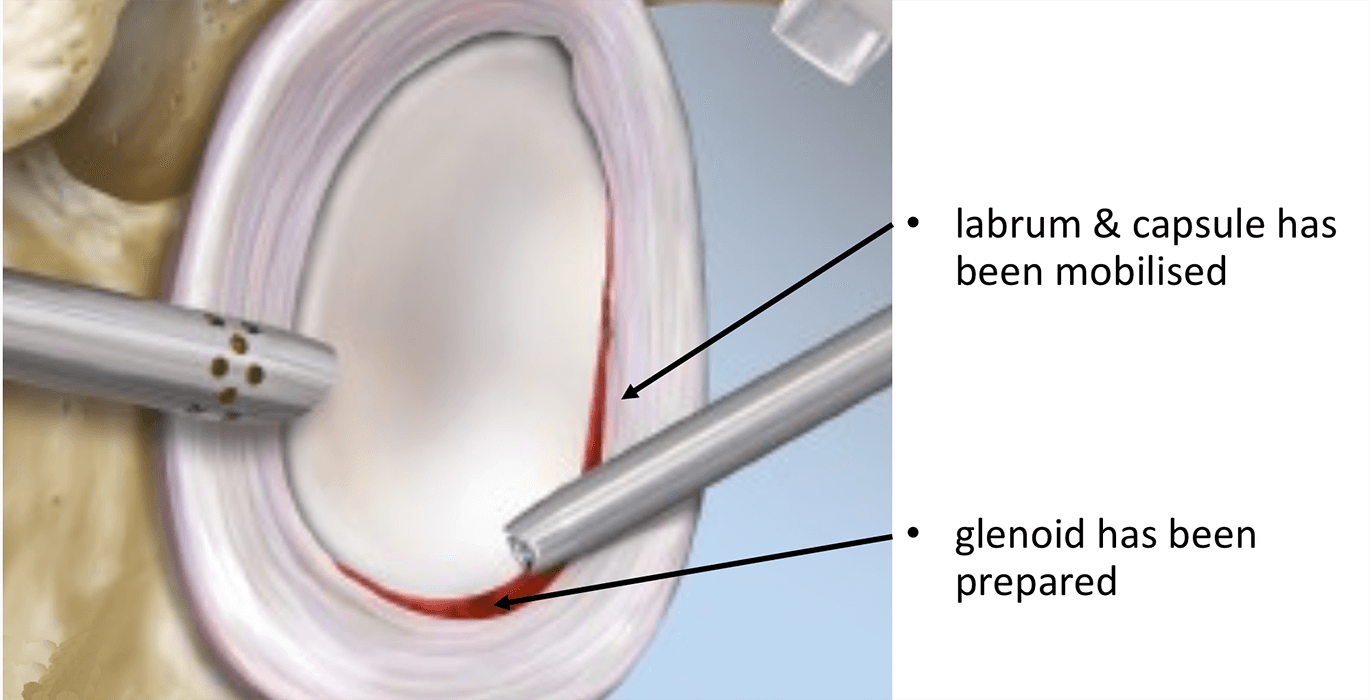
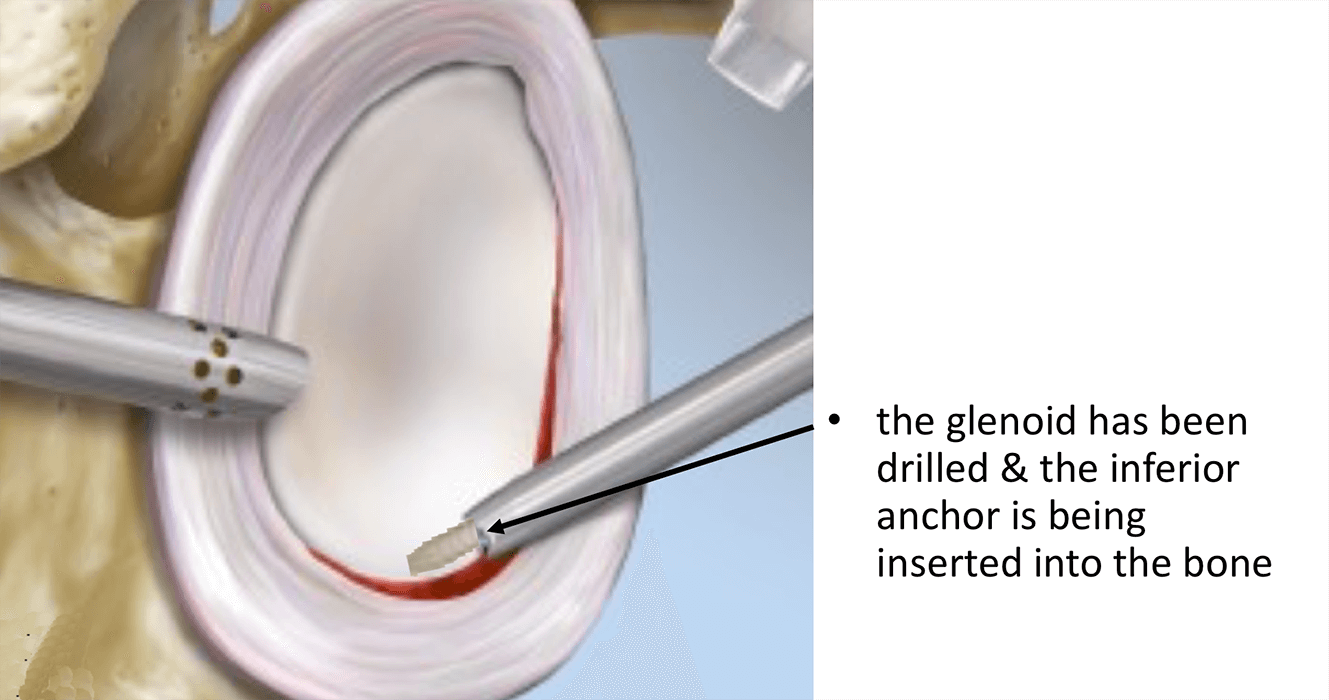
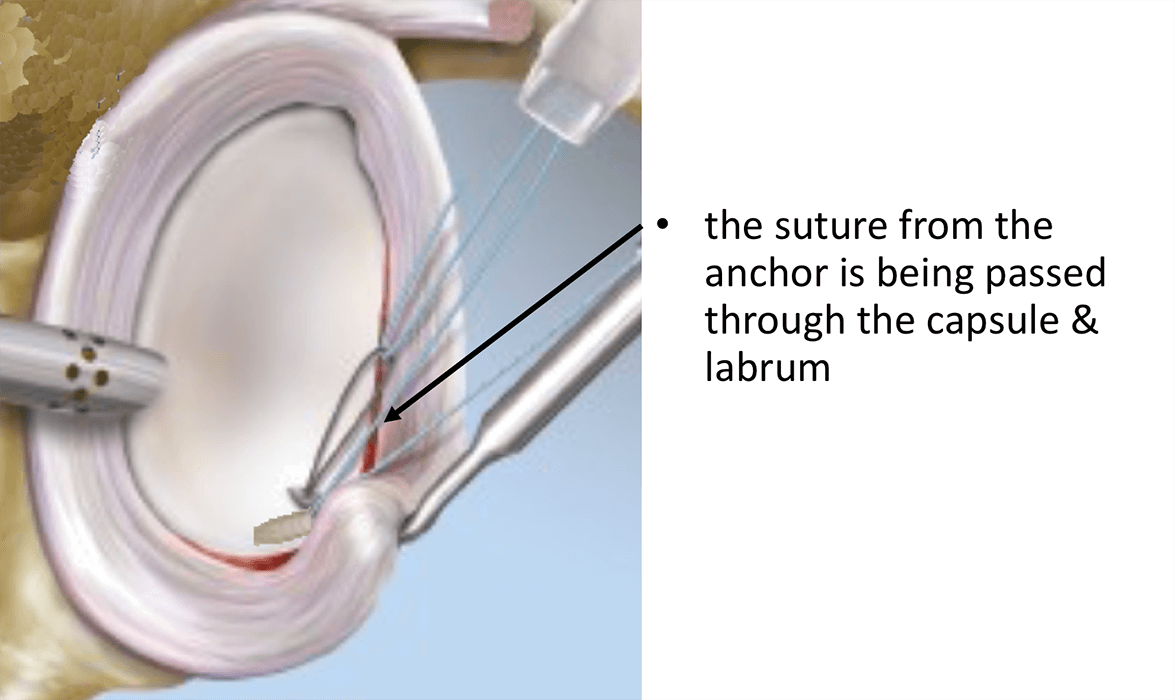
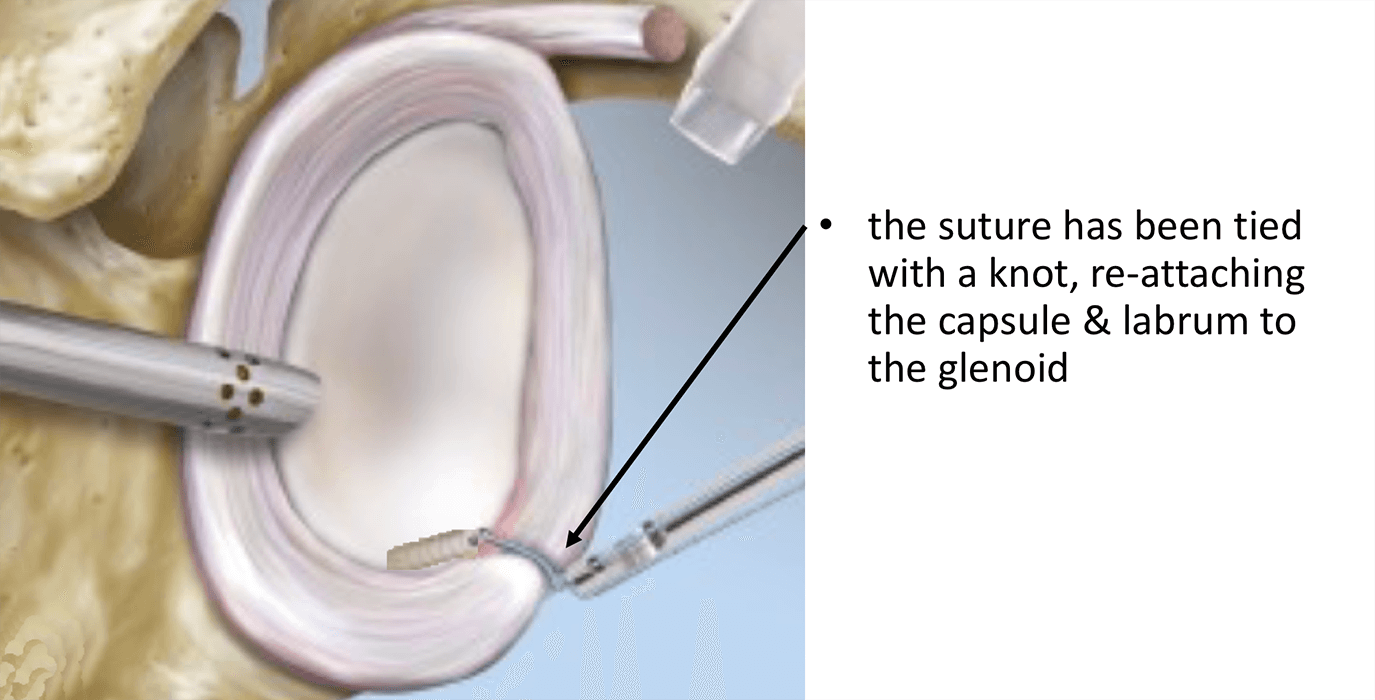
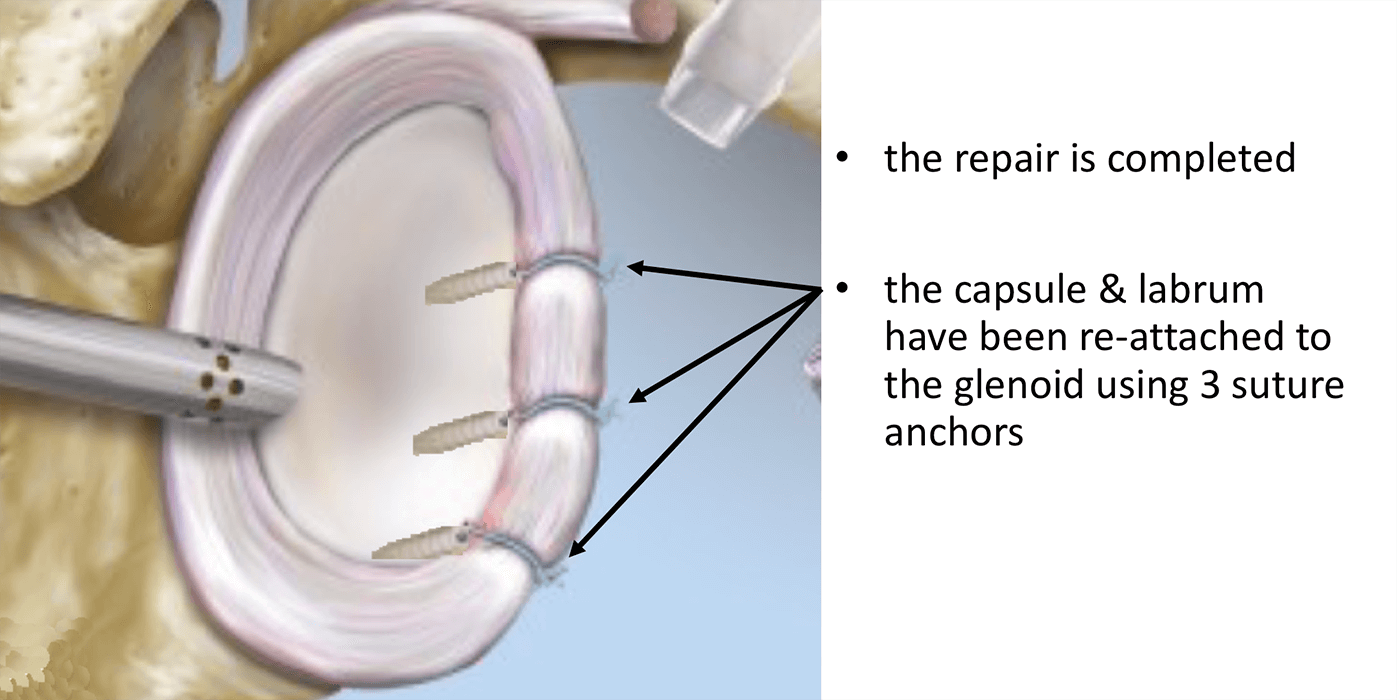
Essentially this involves mobilising and freshening up the torn edges of the ligament and capsule and then re-attaching them on to the front of the Glenoid (Socket), the bone here having also been freshened. The tissue is usually attached to the bone using ‘suture anchors’. These are small implants, made of various materials, that can be inserted, by drill holes, into the bone. Attached to the anchors are sutures that can then be passed through the torn ligaments and capsule and tied down into position. Having re-attached the freshened ligaments and capsule to the freshened bone of the socket they can then heal.
Find out more about suture anchors….
Arthroscopic Bankart Repair (Anterior Shoulder Stabilisation)
A Bankart Repair operation can be undertaken as an open or an arthroscopic procedure. The advantages of an arthroscopic procedure are that smaller incisions are used without having to disturb and cut through other structures and it is possible to more accurately assess the damage to the shoulder and quality of repair.
I undertake all of my Bankart Repairs arthroscopically. There are a number of different variations to the technique and different implants that can be used. I have evolved my technique over the past 15 years, taking advantage of new implants and equipment, and have obtained consistently good results, with which I am happy. My routine Arthroscopic Bankart Repair is described below,
Watch a video of an arthroscopic Bankart Repair….
Find out more about Arthroscopic Shoulder Surgery….
Procedure
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block…. - Prophylactic iv antibiotics are given
- A posterior and 2 anterior portals are used for joint access
- The joint is initially assessed to confirm the presence of the Bankart Tear, to assess the extent of any Hill-Sachs Lesion or Glenoid Bone Loss and any other pathology
- The Bankart Tear is then fully mobilised and the tissues freshened
- The Anterior Glenoid is then prepared and freshened
- 3 Osteoraptor or Pushlok bio-composite anchors are inserted into the anterior, inferior glenoid and the capsule and ligaments re-attached with a superior shift
- The repair is assessed and the wounds closed
After the Surgery
Post-Operative Care
Following an Arthroscopic Bankart Repair the patient may be able to go home that day or may need to stay in the Hospital overnight, depending on circumstances. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team who will instruct them on how to take the sling on and off and the ‘safe zones’ of movement. Further physiotherapy will then be organised from the 3 week mark onwards.
Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month, 3 months and 6 months after their procedure to assess their progress and recovery.
Period of Sling Immobilisation & Rehabilitation Protocol
After an arthroscopic Bankart Repair the patient’s arm needs to be in a sling for 3 weeks. It is initially important to ‘protect’ the repair from any significant load as it begins to heal whilst, at the same time, it is preferable to not allow the shoulder to get too stiff. The physiotherapists will instruct the patient on the ‘safe zones’ of movement out of their sling over this period.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
|
Milestones |
|
|
Week 6 |
Active range of movement at least 75% of normal |
|
Week 12 |
Full ROM, with minor loss of combined abduction and external rotation |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Contact Sport |
|
| Lifting |
|
Success of Surgery, Risks & Complications
Success following an Arthroscopic Bankart Repair has to be assessed slightly differently from other procedures. Rather than being able to measure how much better the shoulder is after the operation we are waiting for a further dislocation NOT to happen. By convention, for a stabilisation procedure to be considered successful, the patient needs to have had no episodes of instability for at least 2 years after their operation.
For a standard Arthroscopic Bankart Repair >90% of patients’ shoulders will be stable 2 years after their surgery. For patients returning to contact sports this figure is decreased to > 80%.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Recurrence – The 2- year re-dislocation rate <10% (for Contact Athletes <20%)
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Anterior Instability with Bone Loss
Management of Traumatic Anterior Shoulder Instability with Bone Loss
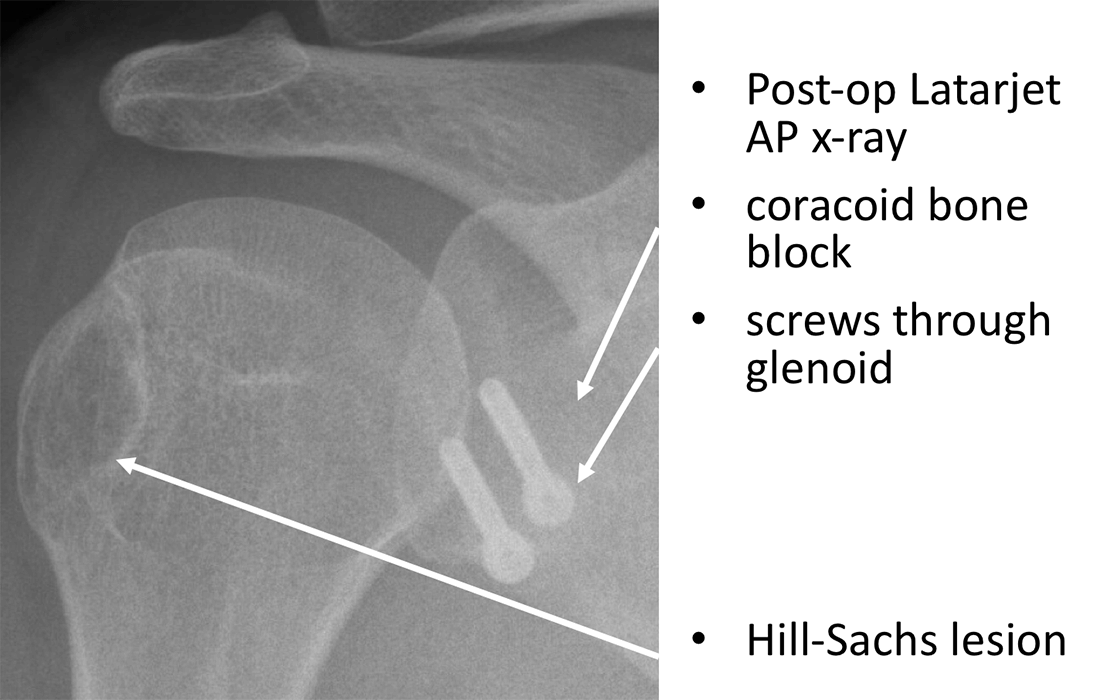
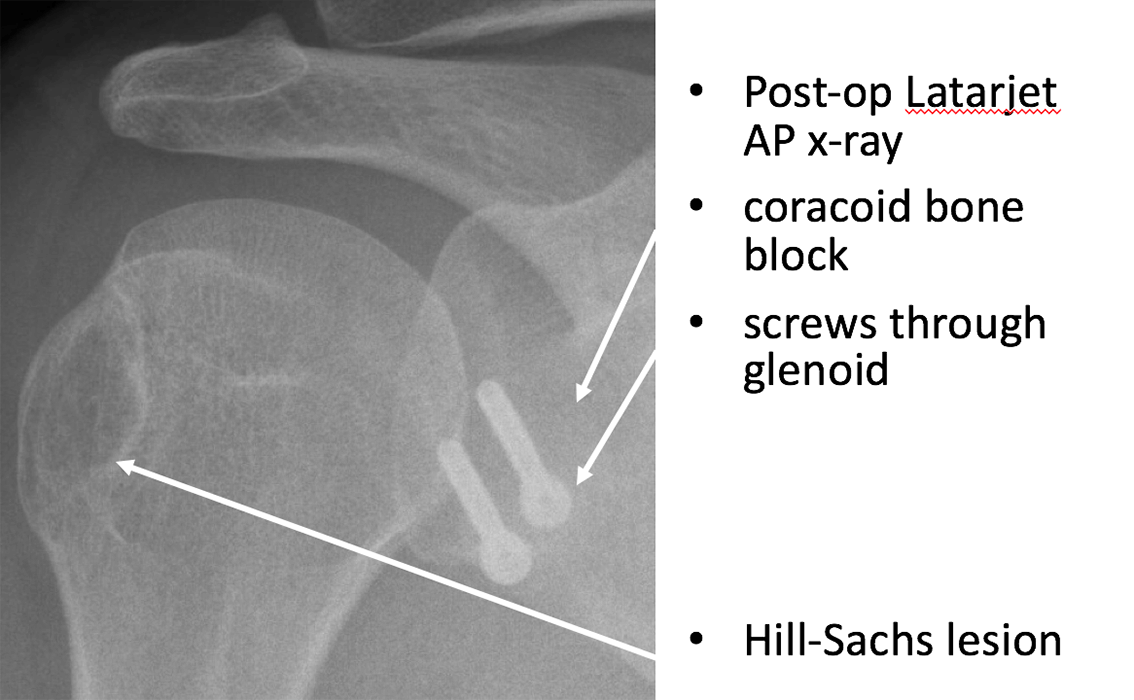
In certain cases of traumatic anterior shoulder instability not only is there a Bankart tear to the capsule and ligament, but there is also significant bone loss at the front of the Glenoid (socket) and/or on the back of the Humeral Head (Hill-Sachs Lesion). This can result from either a particularly forceful initial dislocation or be due to repeated dislocations.
It is possible to undertake a successful soft-tissue Bankart repair with a small amount of bone loss, but there is a threshold where the loss of bone becomes so much that it is unlikely that a soft-tissue procedure, on its own, will successfully stabilise the shoulder. In this case, a different type of procedure is required to help address the additional bone loss.
There is no precise amount of bone loss that will indicate whether a soft-tissue Bankart repair, on its own, will be sufficient to stabilise the shoulder. However, it is generally accepted that a loss of 25% or more of the anterior glenoid bone-stock, coupled with a Hill-Sachs lesion, will significantly decrease the likely success of a Bankart repair. The best way to assess bone loss is on either and MRI scan or CT scan.
A number of different procedures have been described to treat Glenoid bone loss with varying success. The most popular and most successful procedures involve fixing a bone graft onto the front of the damaged Glenoid (Socket) to re-constitute the articular surface. I prefer to adopt this approach and usually either transfer some bone from the adjacent Coracoid Process, with its tendon attached, or take a Bone Graft from the hip to fill the defect at the front of the Glenoid. I am able to do both of these operations either as an open or an arthroscopic procedure. Both procedures are described below.
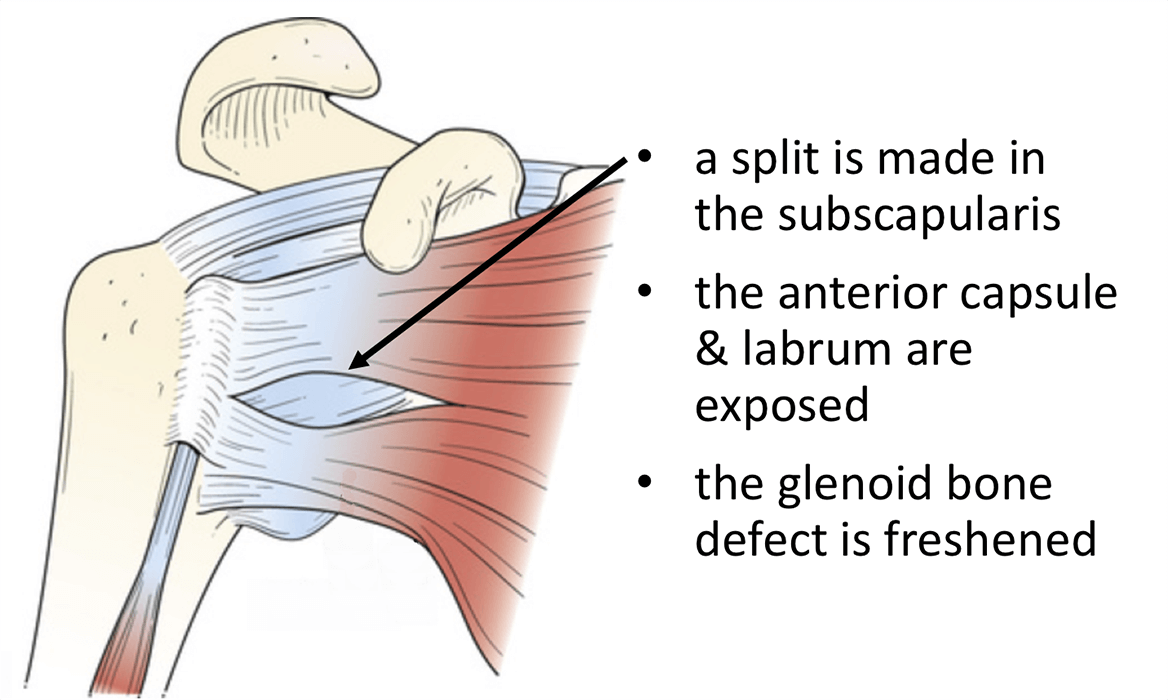
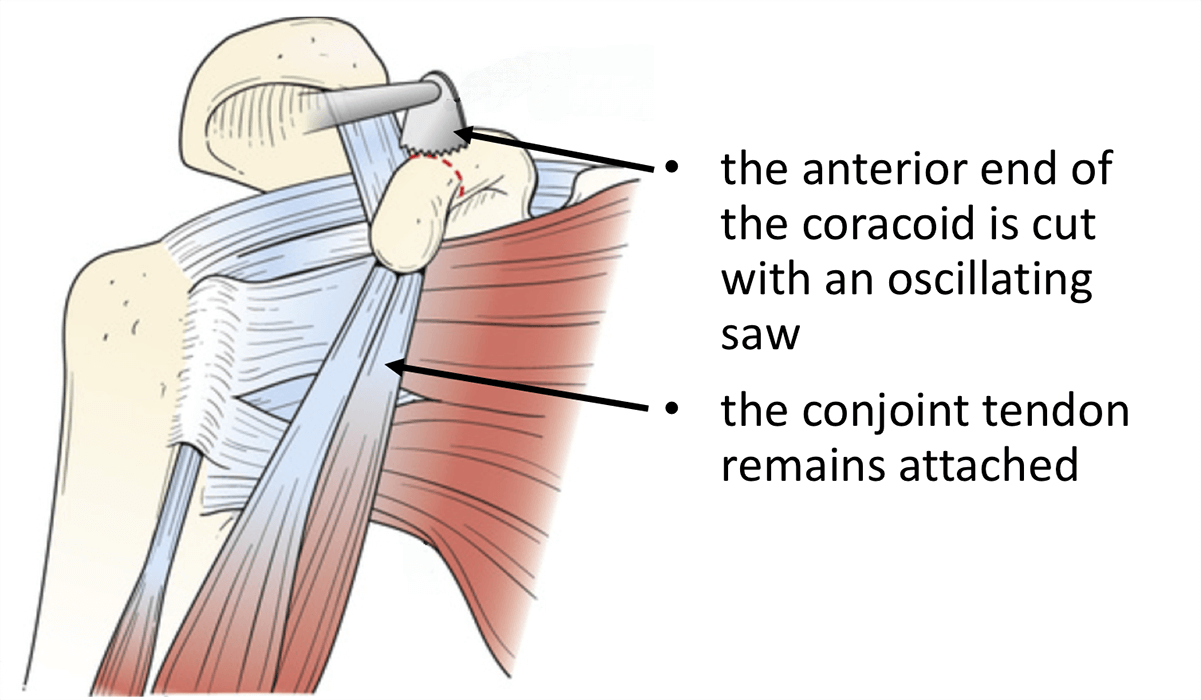
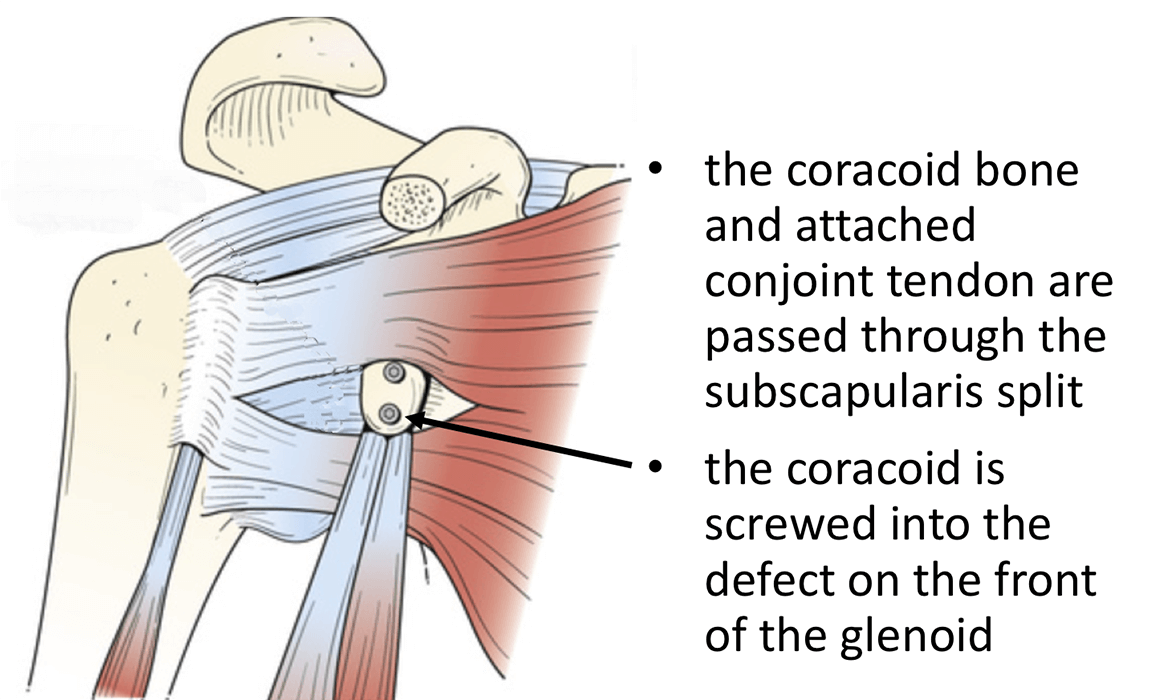
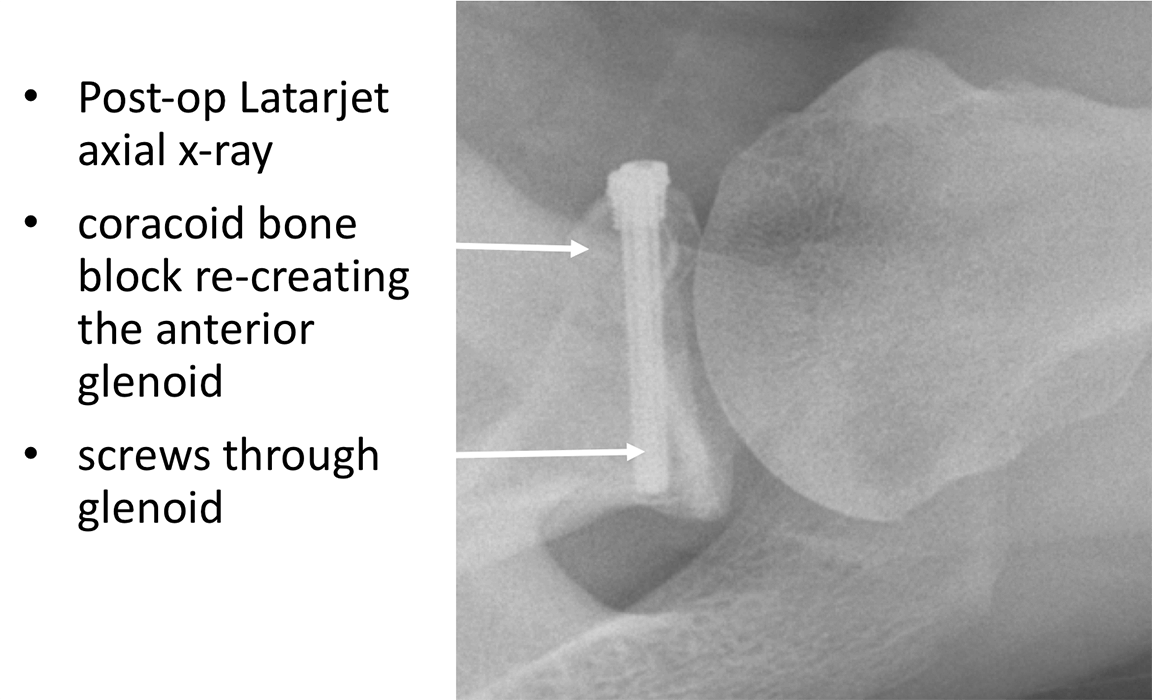
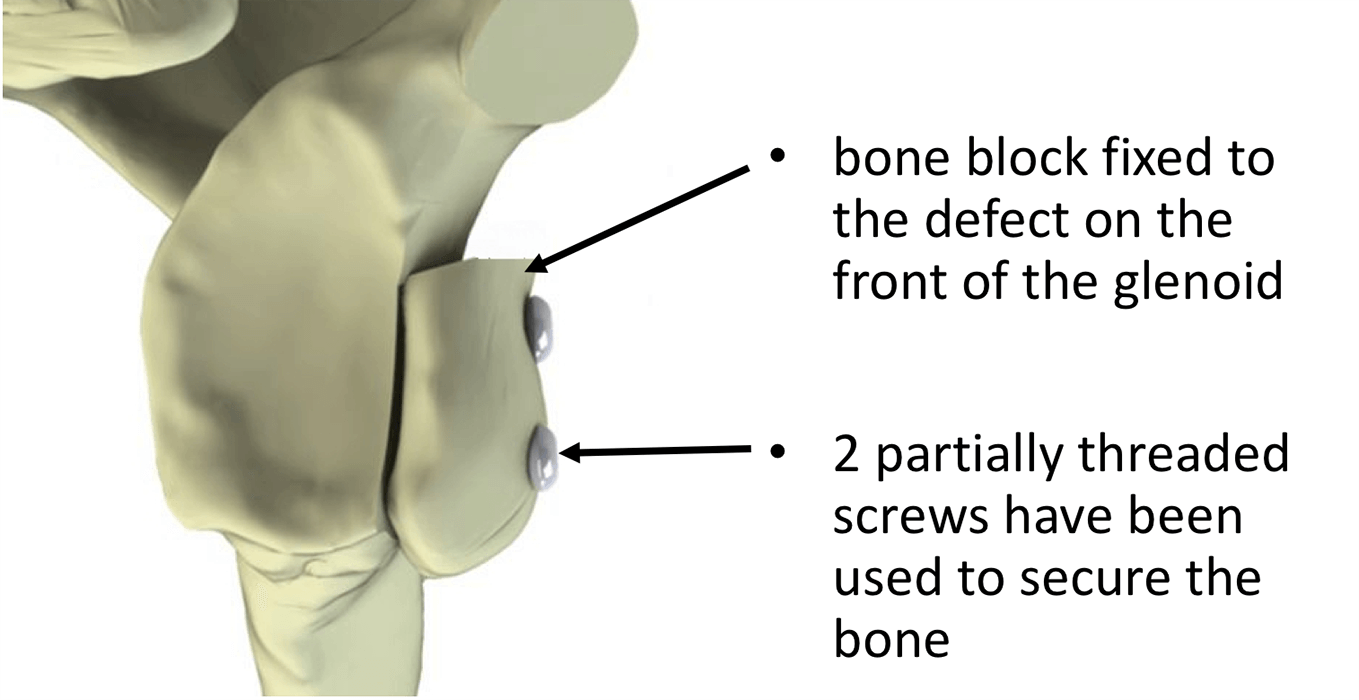
Coracoid Transfer Procedure (Bristow-Latarjet Procedure)
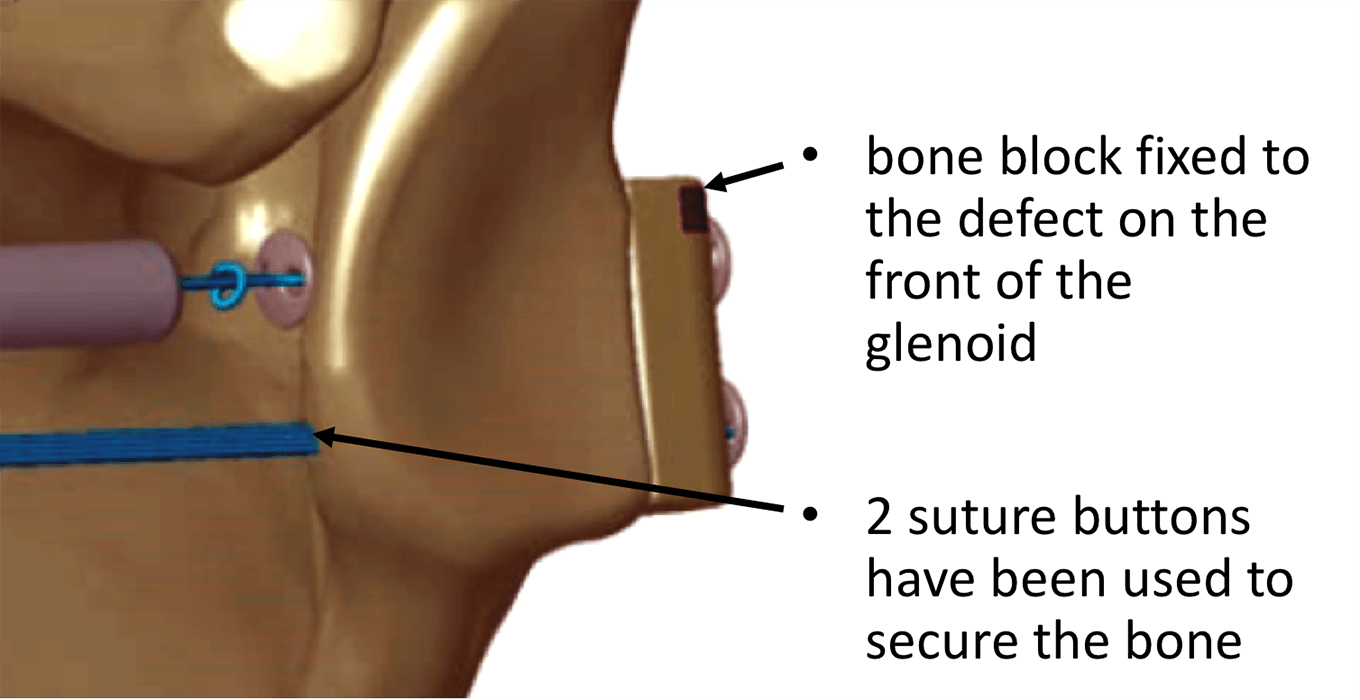
The Latarjet procedure involves cutting the tip of the coracoid process off and then mobilising it with its attached Conjoint Tendon. The bone on the side of the coracoid is then prepared and two drill holes made through it. The Subscapularis tendon at the front of the shoulder is then split in line with its fibres and the joint exposed. The damaged bone at the front of the Glenoid is then prepared. The Coracoid bone is then passed through the split in Subscapularis and positioned on the prepared bone defect on the front of the Glenoid. Through the prepared drill holes in the Coracoid the Glenoid is drilled and 2 screws are inserted fixing the Coracoid graft onto the front of the Glenoid. Various types of screws and suture-button devices can be used to do this. The joint capsule and ligaments are sometimes then re-attached to the glenoid, depending on their condition.
The advantages of the Latarjet procedure is that it is a local bone transfer and does not require a bone graft from elsewhere in the body. Also, by re-positioning the Conjoint tendon over the front of the shoulder, it is able to act as a ‘Dynamic Sling’ adding additional stability. The disadvantages of the procedure are that it is technically challenging, there is often a loss of 5 – 10 degrees of External Rotation, there is a possibility of damage neurovascular structures and it does distort the normal anatomy.
This is my procedure of choice to treat Anterior Shoulder Instability with significant Bone Loss. It is an operation that I am able to undertake as both an Open and Arthroscopic procedure.
Watch a video of an arthroscopic Latarjet procedure….
Find out more about Arthroscopic Shoulder Surgery….
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
Post-Operative Care
Following an Open or Arthroscopic Eden-Hybinette Procedure the patient would usually require to stay in the Hospital overnight. I would see the patient after their surgery to discuss how the procedure has gone and the next morning, having obtained a check X-Ray of the shoulder, to check on their progress and to arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team who will instruct them on how to take the sling on and off and the ‘safe zones’ of movement. Further physiotherapy will then be organised from the 3 week mark onwards.
<Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month with an X-ray, 3 months with an X-Ray and 6 months with a CT Scan after their procedure to assess their progress and recovery.
Period of Sling Immobilisation & Rehabilitation Protocol
After an Eden-Hybinette Procedure the patient’s arm needs to be in a sling for 2 weeks. It is initially important to ‘protect’ the repair from any significant load as it begins to heal whilst, at the same time, it is preferable to not allow the shoulder to get too stiff. The physiotherapists will instruct the patient on the ‘safe zones’ of movement out of their sling over this period.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
|
Milestones |
|
|
Week 6 |
Active range of movement at least 75% of normal |
|
Week 12 |
Full ROM, with minor loss of combined abduction and external rotation |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Contact Sport |
|
| Lifting |
|
Success of Surgery, Risks & Complications
Success following a Latarjet Procedure has to be assessed slightly differently from other procedures. Rather than being able to measure how much better the shoulder is after the operation we are waiting for a further dislocation NOT to happen. By convention, for a stabilisation procedure to be considered successful, the patient needs to have had no episodes of instability for at least 2 years after their operation.
For a standard Latarjet Procedure >95% of patients’ shoulders will be stable 2 years after their surgery. For patients returning to contact sports this figure is slightly decreased to > 90%.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Recurrence – The 2- year re-dislocation rate is < 5% (for Contact Athletes <10%)
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.5%
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
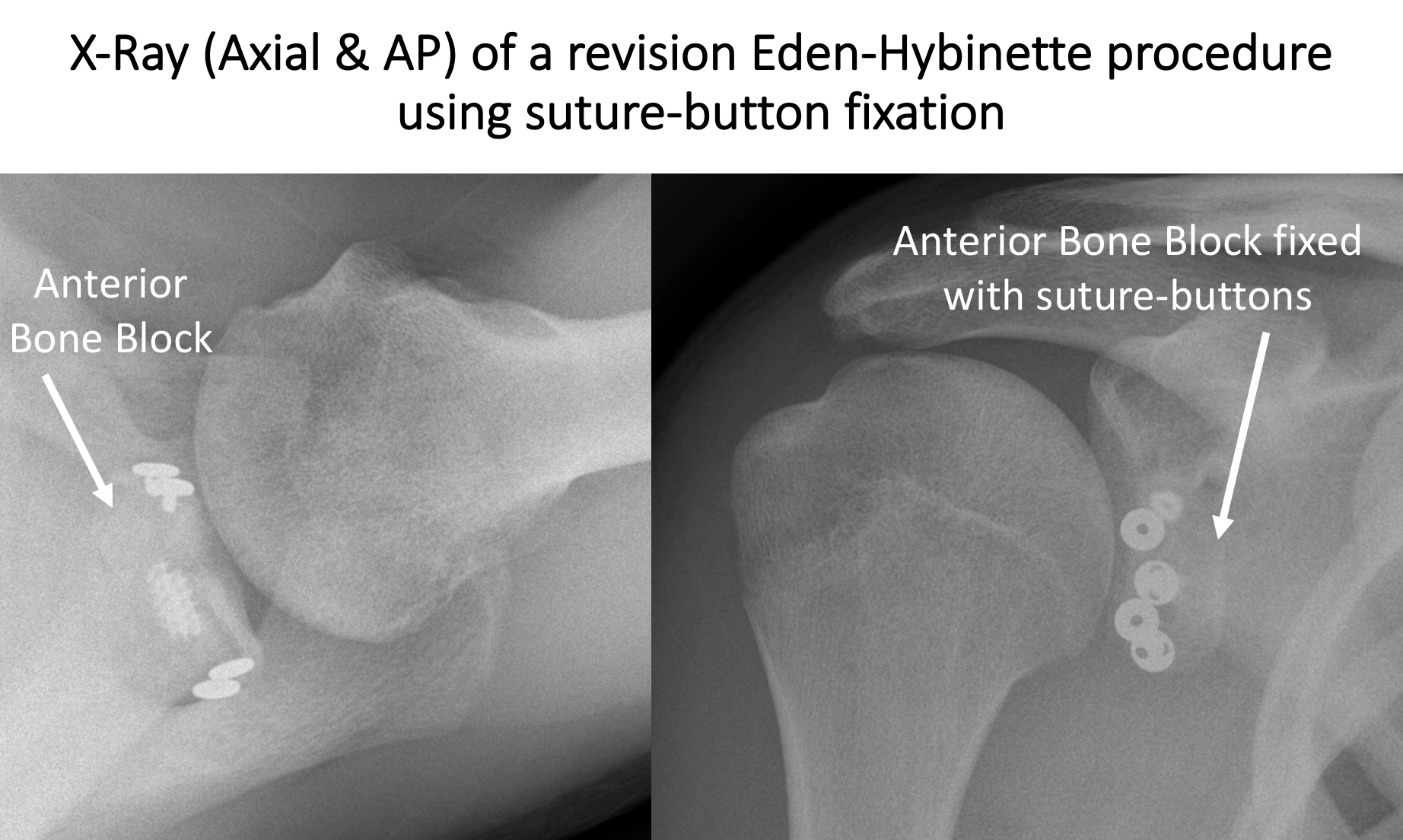
Anterior Bone Block Procedure (Eden-Hybinette Procedure)
The standard Eden-Hybinette uses a 1.5 – 2cm tri-cortical Bone Graft that is harvested from the Iliac Crest, which is the bone at the front of the hip. This is done through a 5cm incision just above the crest and, although sometimes painful for a time afterwards, does not usually lead to any detrimental function. The Bone Graft is then prepared with 2 drill holes.
The front of the shoulder is then approached and, by either splitting the Subscapularis Tendon along the line of its fibres or by retracting the top edge of it downwards, the front of the Glenoid exposed. The area of the Glenoid defect is then prepared and the pre-prepared Bone Graft positioned over it. Through the prepared drill holes in the Bone Graft the Glenoid is drilled and 2 screws are inserted fixing the Bone Graft onto the front of the Glenoid. Various types of screws and suture-button devices can be used to do this. The joint capsule and ligaments are sometimes then re-attached to the glenoid, depending on their condition.
The advantage of the Eden-Hybinette procedure is that none of the other structures around the shoulder are disturbed and it recreates the near normal anatomy. The disadvantages of the procedure are that it requires a donor site at the hip, there is often a loss of 5 – 10 degrees of External Rotation and that it does not provide the additional ‘Dynamic Sling’ effect that the Latarjet procedure offers.
Watch a video of an arthroscopic Eden-Hybinette procedure….
Watch a video of an arthroscopic Eden-Hybinette procedure….
Find out more about having an anaesthetic….
Find out more about an Inter-scaelene Nerve Block….
Post-Operative Care
Following an Open or Arthroscopic Latarjet Procedure the patient would usually require to stay in the Hospital overnight. I would see the patient after their surgery to discuss how the procedure has gone and the next morning, having obtained a check X-Ray of the shoulder, to check on their progress and to arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team who will instruct them on how to take the sling on and off and the ‘safe zones’ of movement. Further physiotherapy will then be organised from the 3 week mark onwards.
find out more about the Supraspinatus Tendon and the Acromion…
I would usually review patients in the clinic 1 month with an X-ray, 3 months with an X-Ray and 6 months with a CT Scan after their procedure to assess their progress and recovery.
Period of Sling Immobilisation & Rehabilitation Protocol
After an Eden-Hybinette Procedure the patient’s arm needs to be in a sling for 2 weeks. It is initially important to ‘protect’ the repair from any significant load as it begins to heal whilst, at the same time, it is preferable to not allow the shoulder to get too stiff. The physiotherapists will instruct the patient on the ‘safe zones’ of movement out of their sling over this period.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
|
Milestones |
|
|
Week 6 |
Active range of movement at least 75% of normal |
|
Week 12 |
Full ROM, with minor loss of combined abduction and external rotation |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Contact Sport |
|
| Lifting |
|
Success of Surgery, Risks & Complications
Success following an Eden-Hybinette Procedure has to be assessed slightly differently from other procedures. Rather than being able to measure how much better the shoulder is after the operation we are waiting for a further dislocation NOT to happen. By convention, for a stabilisation procedure to be considered successful, the patient needs to have had no episodes of instability for at least 2 years after their operation
For a standard Eden-Hybinette Procedure >95% of patients’ shoulders will be stable 2 years after their surgery. For patients returning to contact sports this figure is slightly decreased to > 90%.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Recurrence – The 2- year re-dislocation rate is < 5% (for Contact Athletes <10%)
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
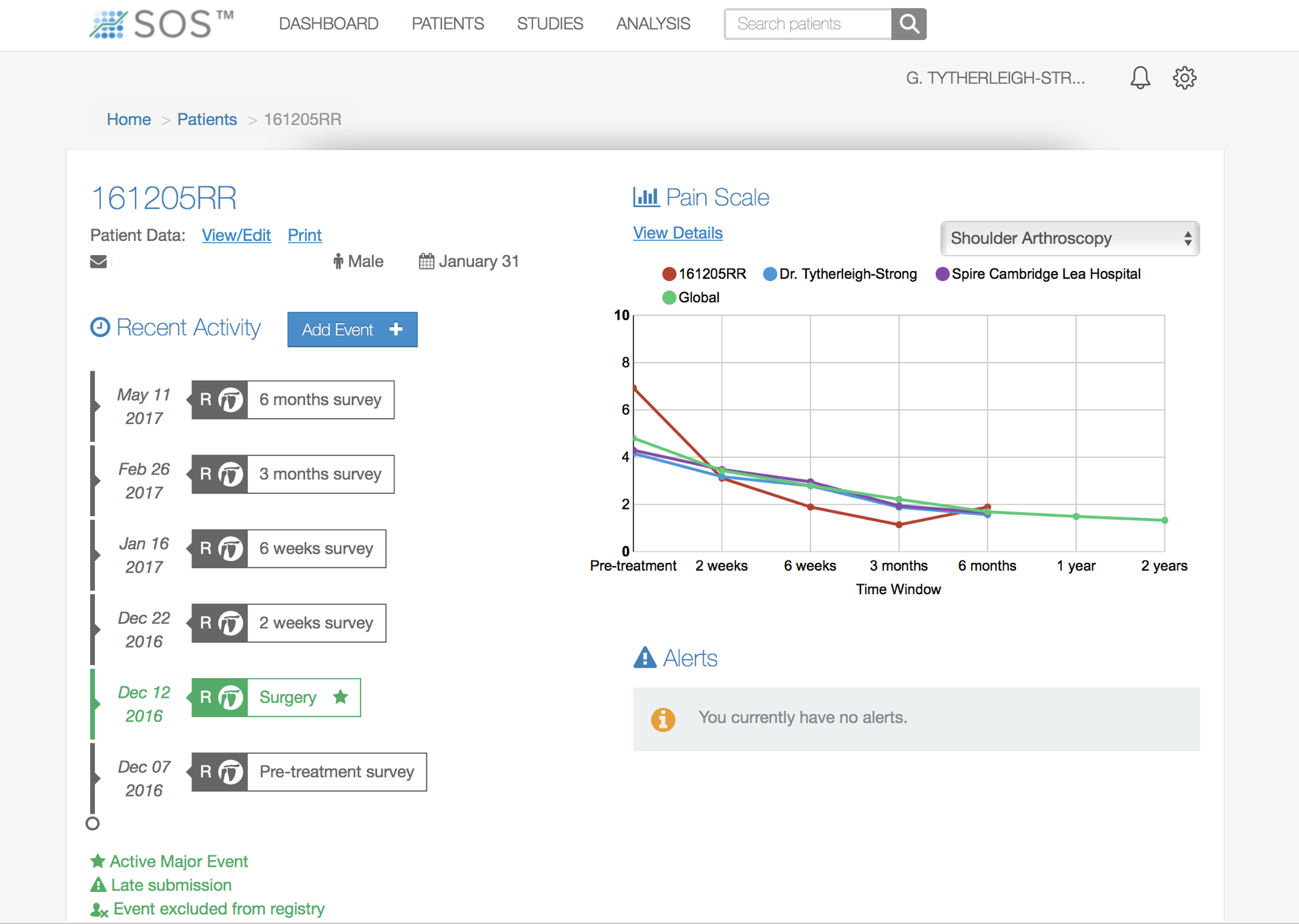
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise. It is able to follow and document an individual patient’s progress, can assess the cumulative outcomes of patients undergoing the same procedure and can be a very useful research tool.
I use a web-based outcome system, SOS (Surgical Outcome Scores) to help me and my patients assess their progress and recovery. This will usually be discussed with the patient in the Out-Patient Clinic, when we have decided to proceed with surgery. My Research Nurse will then contact them prior to their surgery to enroll them and record some base line data. Following surgery patients will be contacted occasionally at set time intervals to assess their progress. This is predominantly an internet based system, but it is possible to arrange for the data to be recorded by either phone or by post.
Of course, this is an entirely voluntary process and there would be no problem if someone did not want to participate. All of the data collected is held securely and anonymized.
Management of Large/Isolated Hill-Sachs Lesion
In most instances the contribution to shoulder instability created by the Hill-Sachs lesion, at the back of the humeral head, is adequately corrected by a Bone-Block procedure to the front of the Glenoid (Socket). Occasionally, however, when the Hill-Sachs defect is very large or if there isn’t significant glenoid bone loss to warrant a Bone-Block procedure, surgery to correct nds.
Like bone loss at the front of the Glenoid, many procedures have been described to treat a large Hill-Sachs lesion. As this is a very unusual problem the most appropriate procedure needs to be tailored specifically for each case. The 3 types of procedures that are available are.
- Arthroscopic Infraspinatus Remplissage
- A Humeral Head Allograft
- A Hemiarthroplasty (Shoulder Replecement)
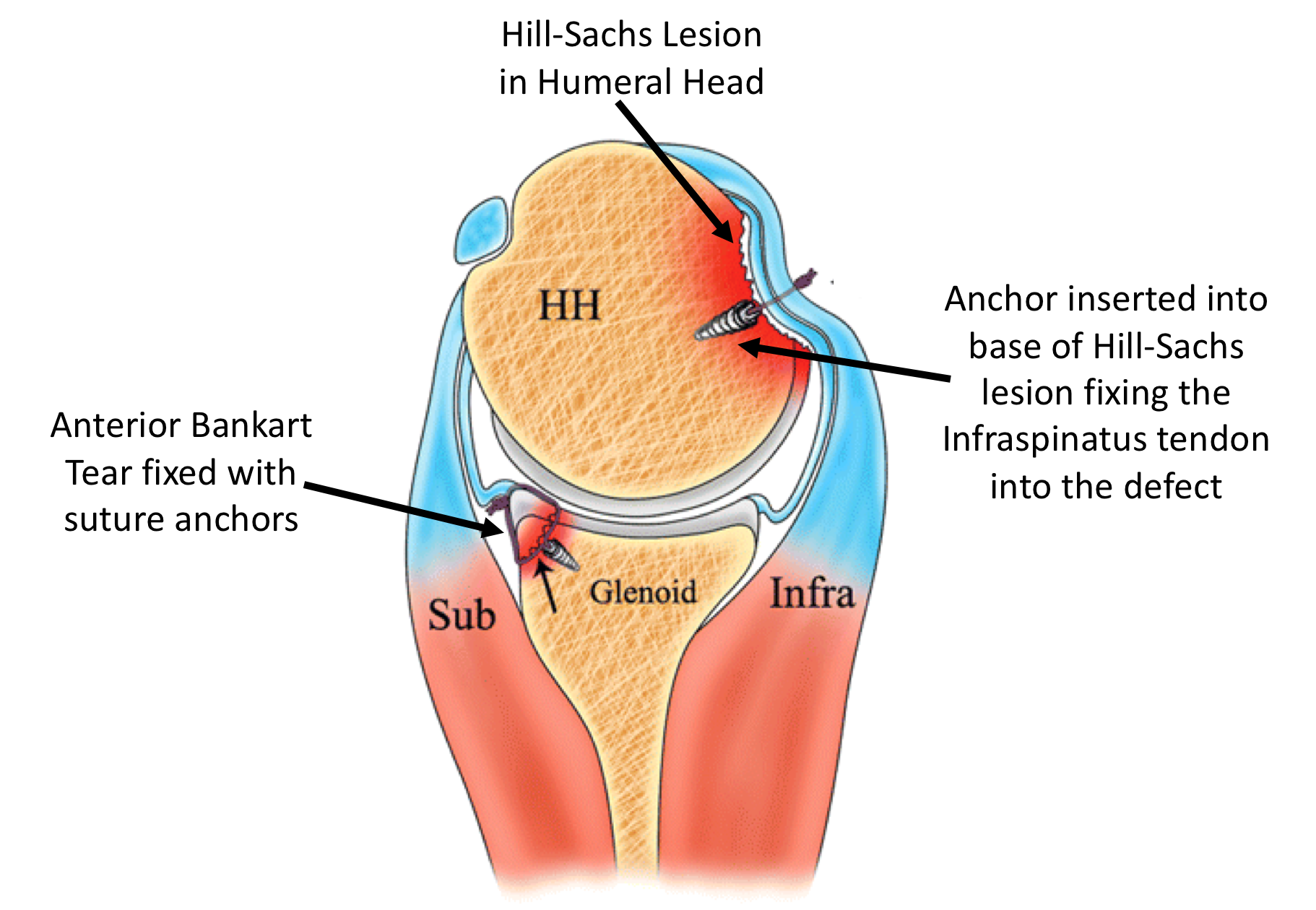
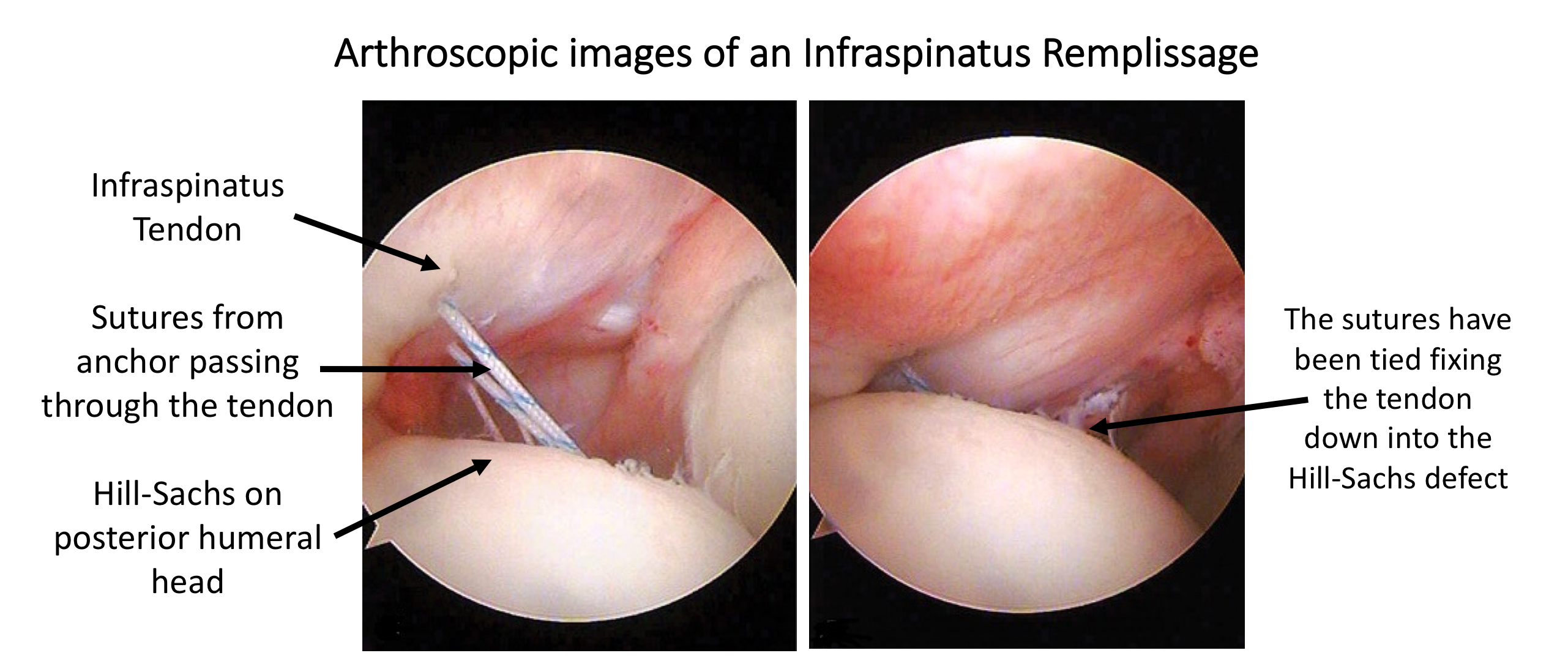
Arthroscopic Infraspinatus Remplissage
The most straightforward procedure, that is appropriate for most intermediate cases, is an Infraspinatus Remplissage. This is often coupled with an anterior bone block procedure used to address any concomitant anterior inferior glenoid bone loss.
An Infraspinatus Remplissage involves de-corticating (roughening up) the bone at the base of the Hill-Sachs lesion. The Infraspinatus tendon, which is attached to the humeral head where the Hill-Sachs lesion is positioned, is then ‘fixed’ down onto the bony bed.
This procedure can be done using an arthroscopic technique, securing the tendon to the bone using suture anchors. The rational is that the tendon will heal into the bone defect so that, when the humeral head rotates into external rotation, the newly fixed tendon will prevent the defect from engaging with the humeral head. Although this initial restricts external rotation, it can recover over time.
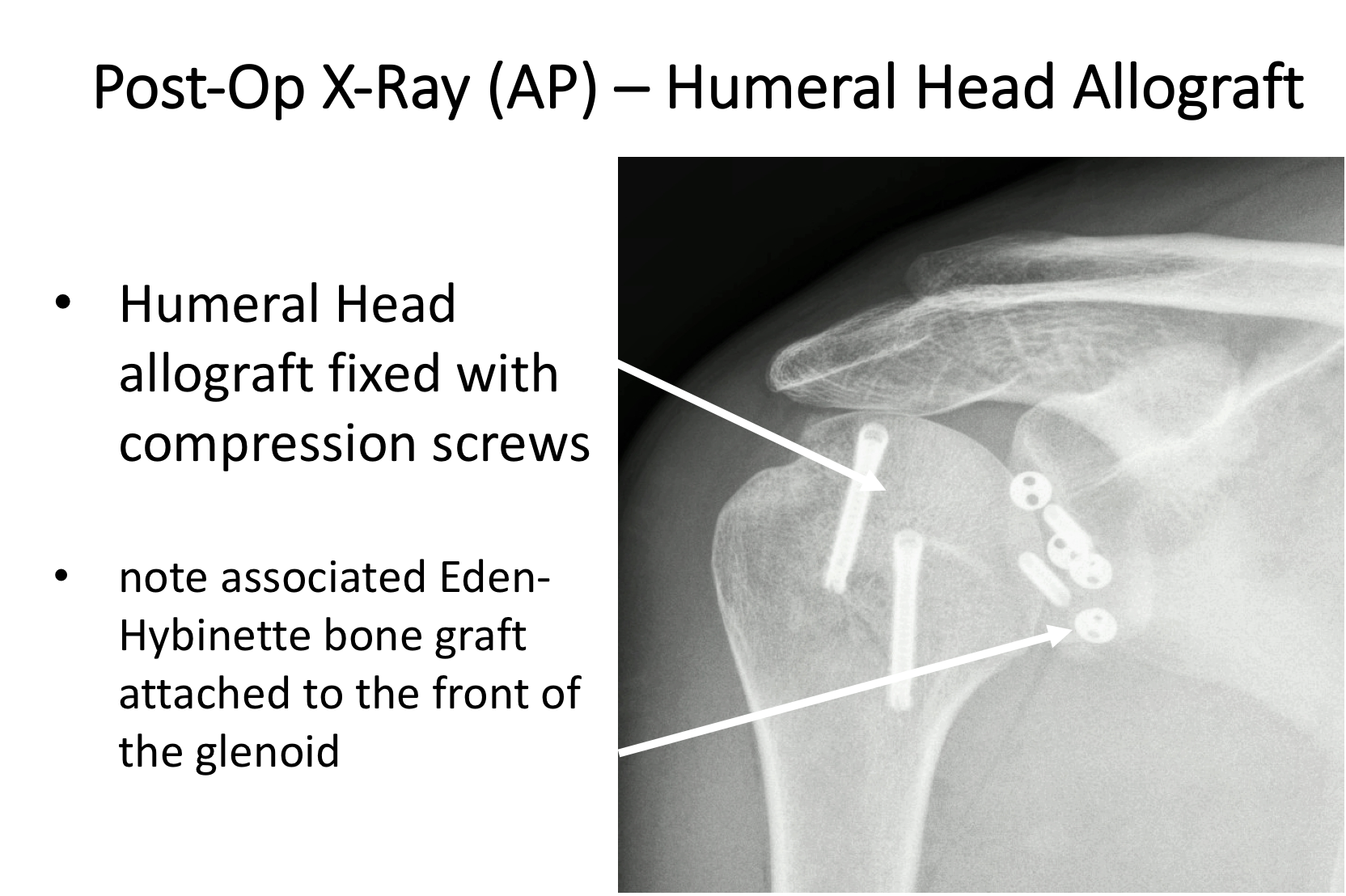
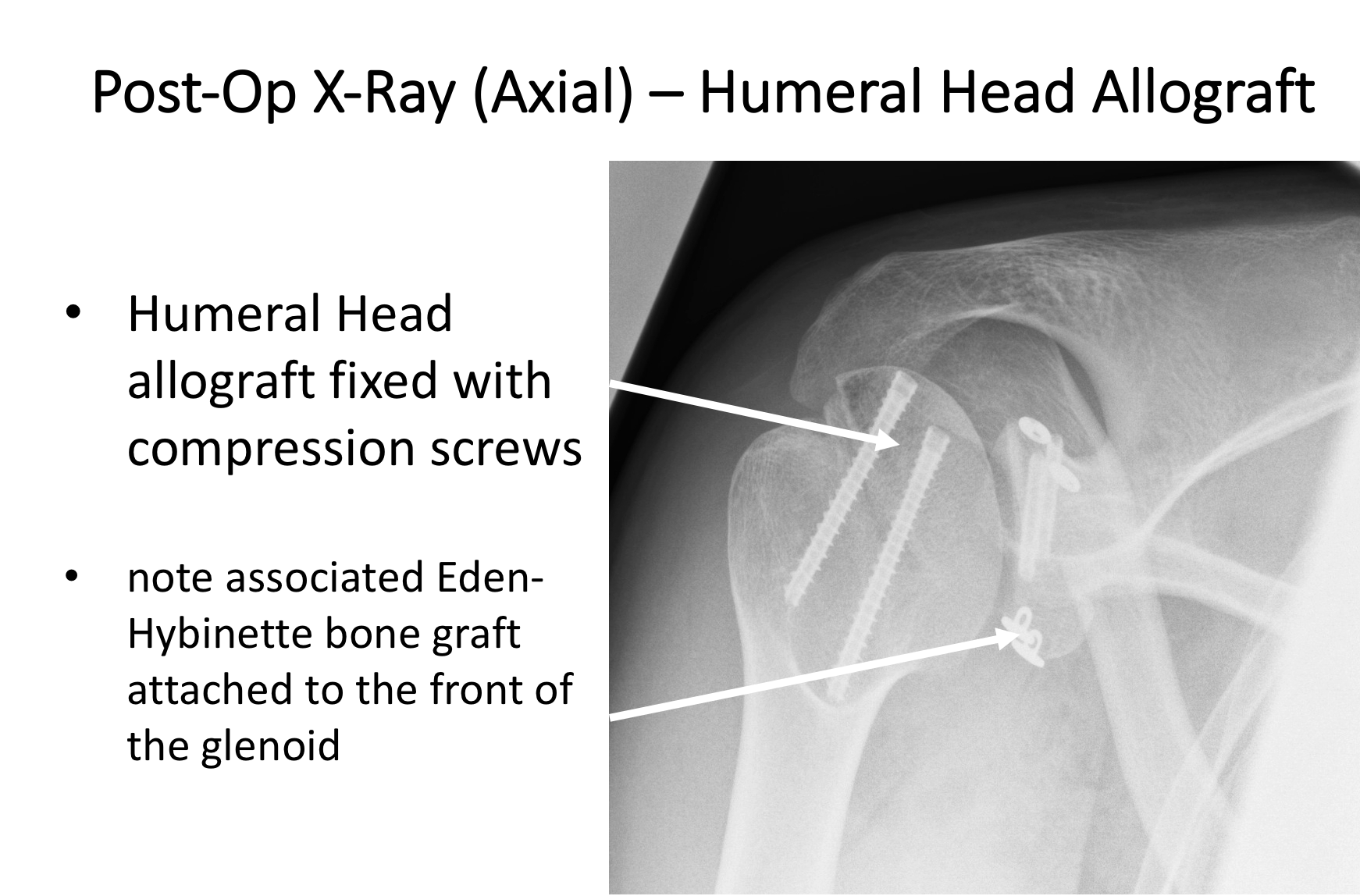
Humeral Head Allograft
This procedure involves using a matched osteo-articular humeral head allograft from a donor. It is usually reserved for very large Hill-Sachs lesions in younger patients. This tends to be in patients that have suffered from repeated epileptic fits, in which they have had multiple ‘violent’ anterior dislocations of the shoulder.
A Humeral Head allograft is undertaken as an open procedure. Survival of the graft has to be carefully monitored over several years. There is a chance that the graft may resorb over time resulting in the development of osteoarthritis. If this occurs, and is symptomatic, a shoulder Hemiarthroplasty maybe required.
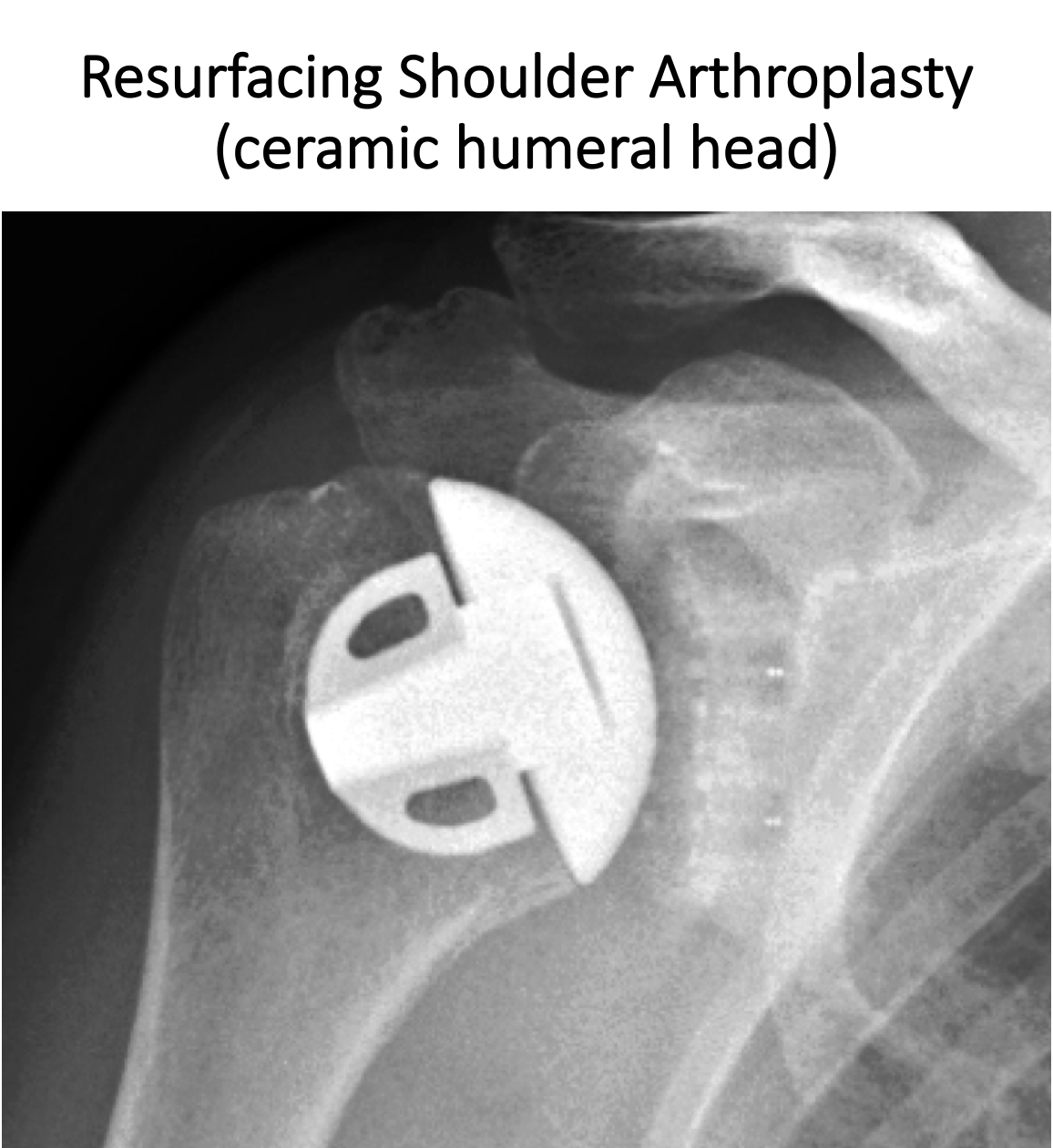
Humeral Head Hemiarthroplasty
In older patients who have had multiple dislocations and have developed a large Hill-Sachs lesion, the rest of the humeral head often undergoes significant ‘wear and tear’, leading to osteoarthritis. In these cases undertaking a ‘resurfacing hemiarthroplasty’ is the best way to address this problem.
Find out more about Humeral Head Hemiarthroplasty…. (Shoulder Arthritis – Shoulder Arthritis 4 – Shoulder Replacement)
Posterior Shoulder Instability
Posterior Shoulder Instability (Dislocation)
Posterior dislocations of the shoulder are far less common than anterior dislocations (5%). The shoulder, glenohumeral joint, is held in joint by a number of stabilising structures.
Shoulder Stabilisers
The shoulder is the most mobile joint in the body with a relatively small socket (gelnoid) and large head (humeral head). This configuration means that it is potentially unstable and it is the most frequently dislocated joint in the body. Fortunately, this still occurs relatively rarely and is because there are a number of mechanisms that help to keep it in joint. These are divided into 2 groups,
- Static Stabilisers – these are the socket (glenoid) with its convex shape, the glenoid labrum (that deepens the socket) and the ligaments that connect the ball to the socket.
- Dynamic Stabilisers – these are the multiple groups of muscles that surround the shoulder girdle and work in a complex rhythm to move the shoulder whilst keeping it in joint.
Types of Dislocations
When the shoulder dislocates or subluxes it will be due to an injury or failure of either the dynamic or static stabilisers or both. There are 3 ways in which shoulder stability fails,
- Traumatic Injury –
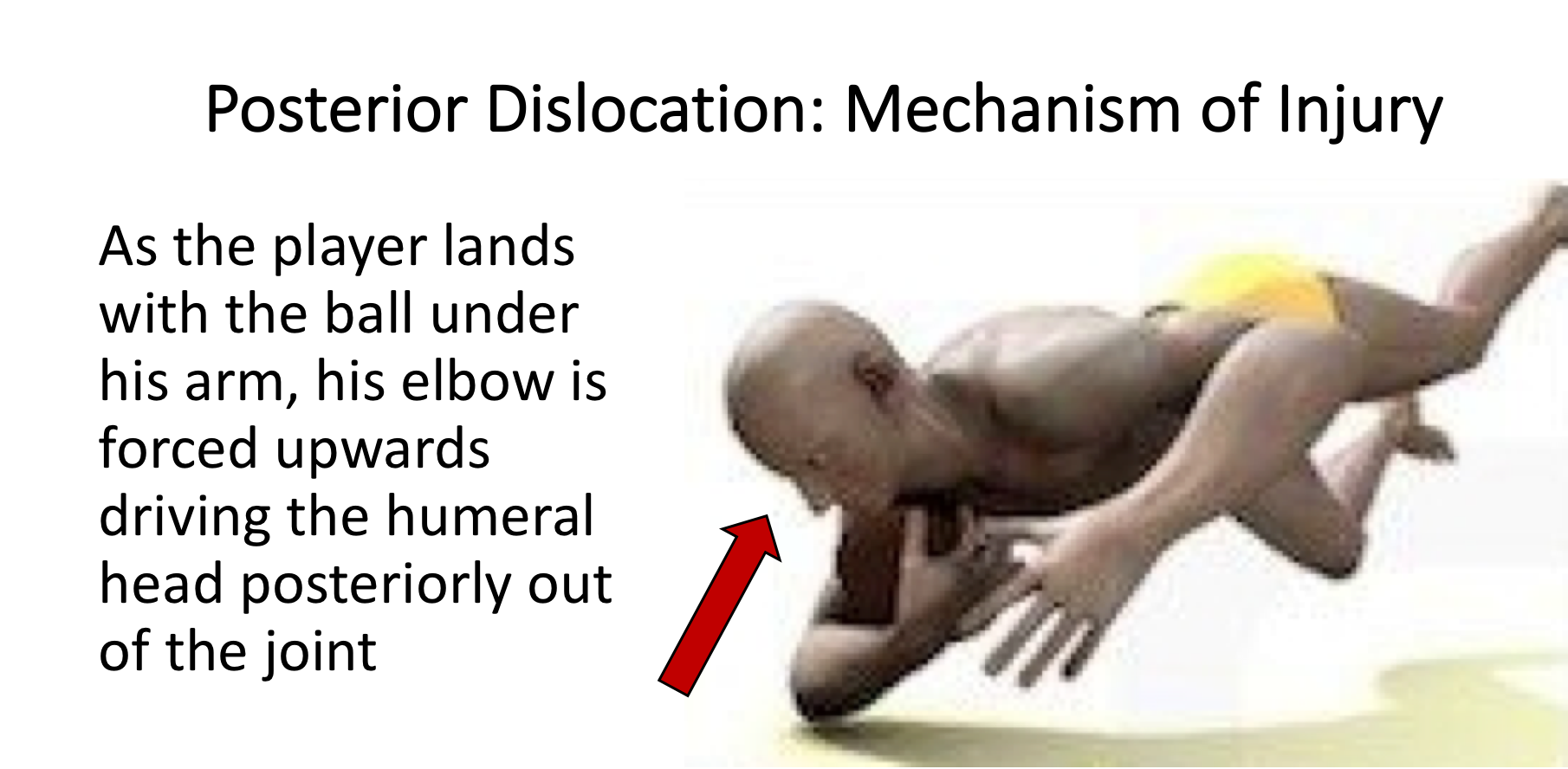
- Posterior dislocations of the shoulder are much less common than anterior dislocations and may often be missed. Athletes, such as rugby players, weight-lifters, throwers and swimmers tend to be at higher risk. They often have inherently lax shoulders, which can be an advantage in their sport, but can make them more vulnerable to injury.
- Traumatic posterior dislocations can occur as the result of a single specific injury. The majority of posterior dislocations reduce spontaneously, immediately after the injury, and by the time the patient is seen in the emergency room the shoulder has reduced and the x-ray may appear normal.
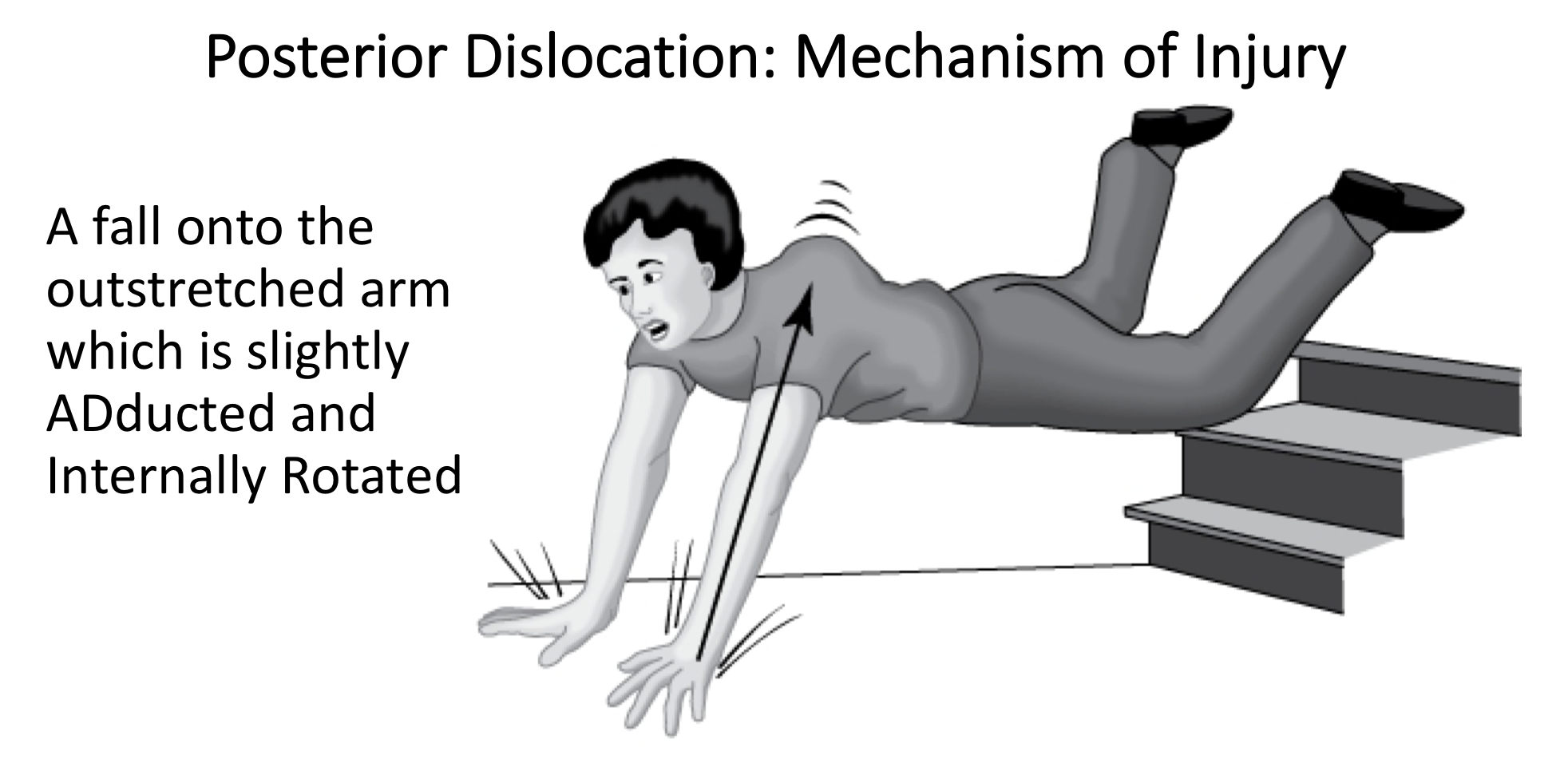
Single Traumatic Injury-
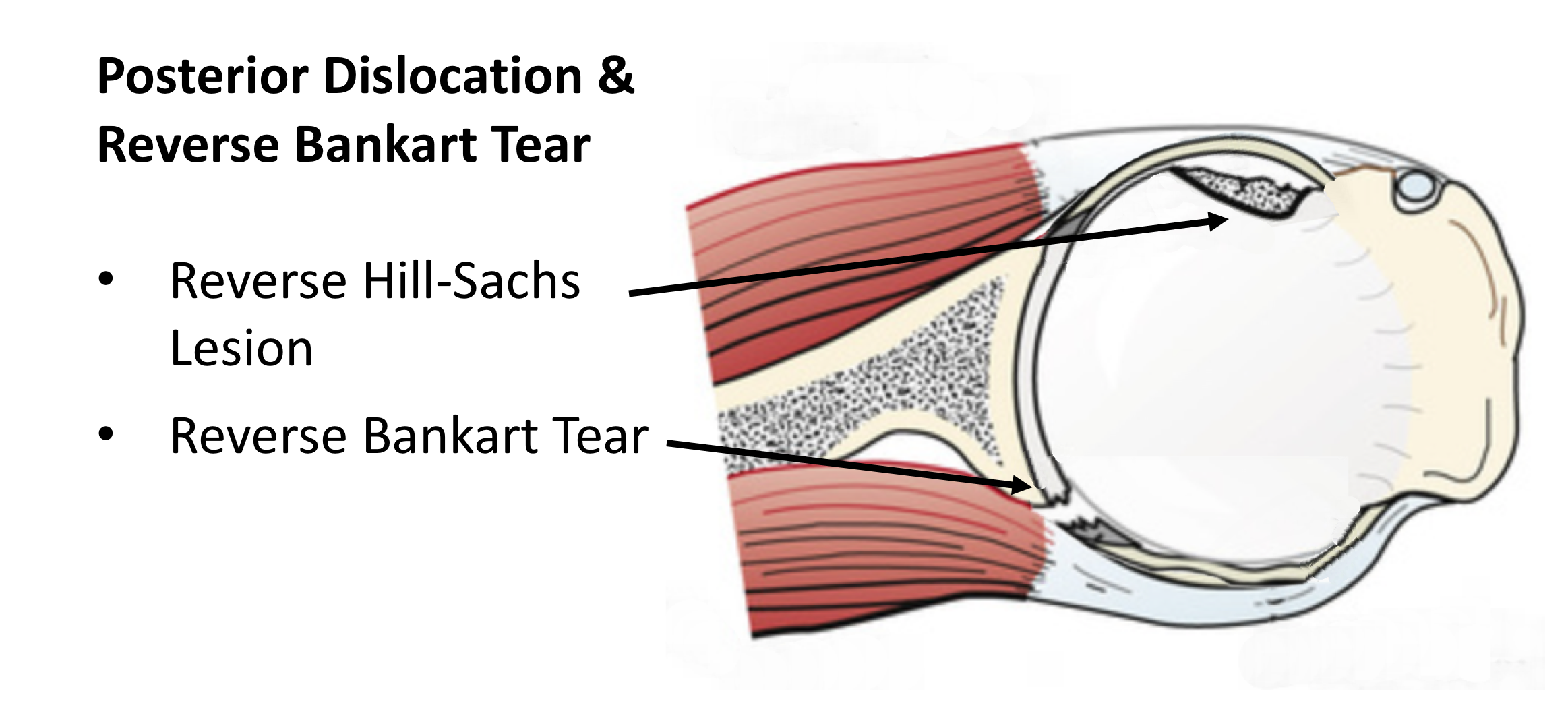
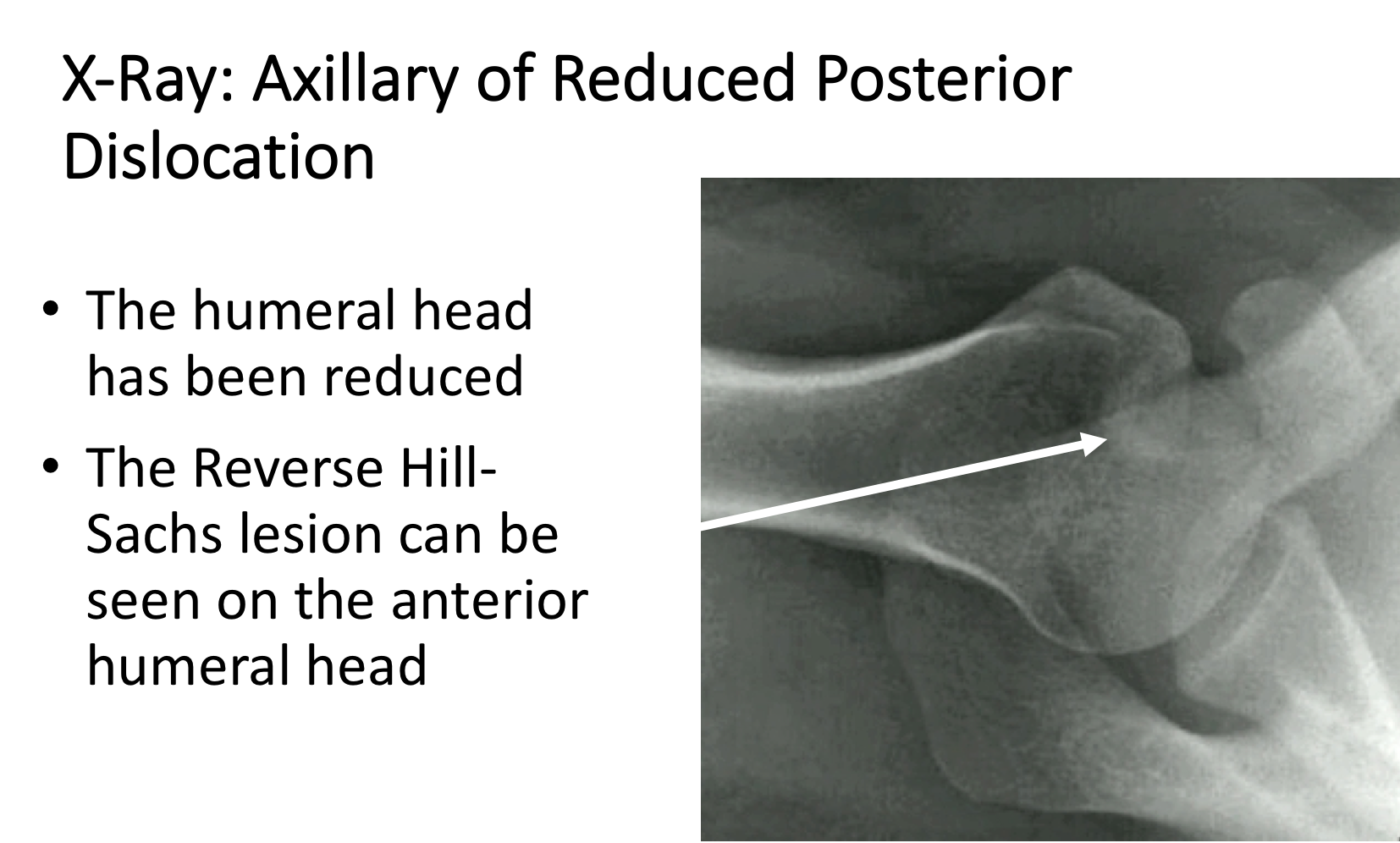
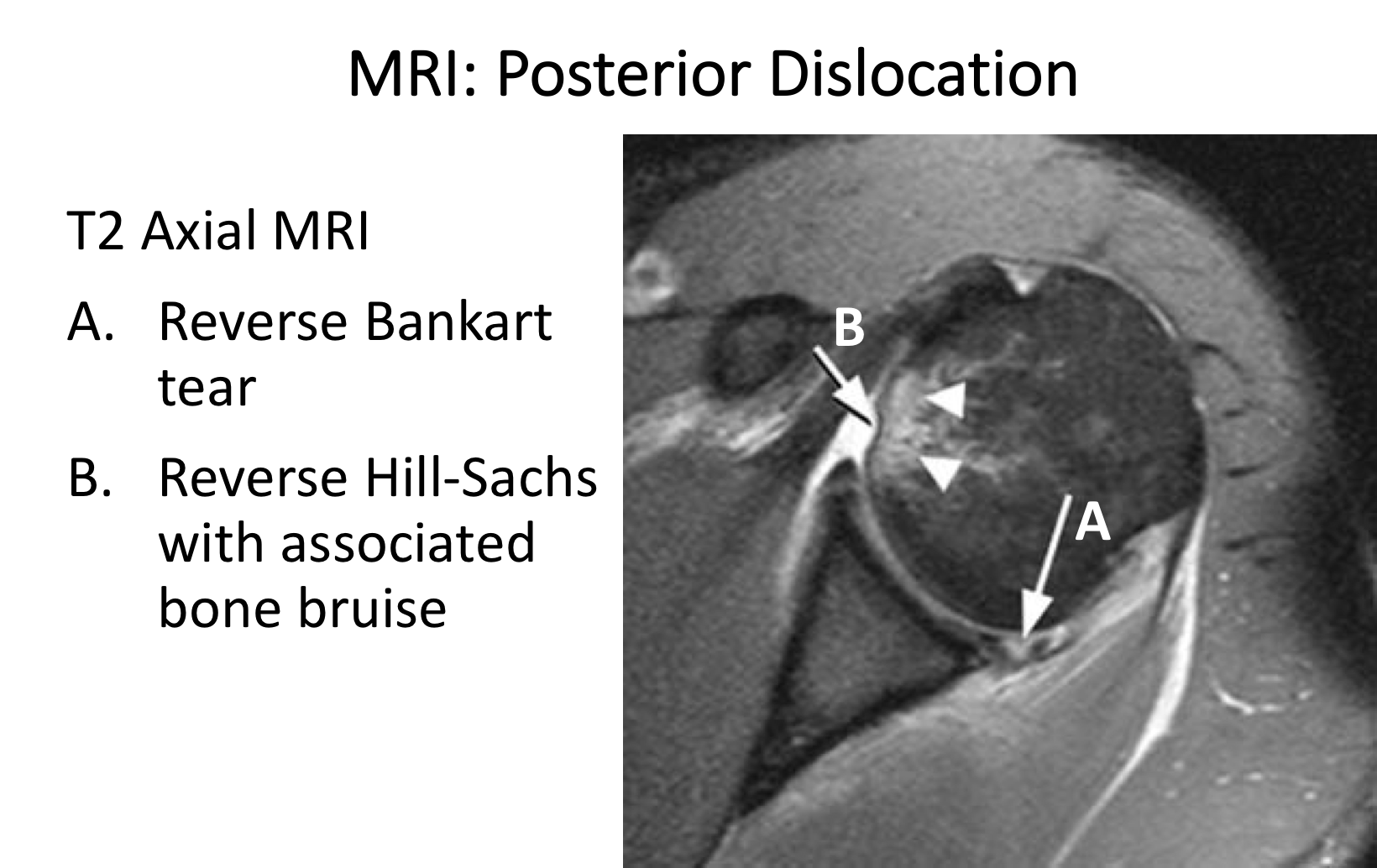
- a posterior dislocation usually occurs when a patient falls onto their arm when reaching across their body with the arm internally rotated. This will tend to force the humeral head backwards out of the glenoid and tearing / breaking the capsulolabral insertion. This creates a Reverse Bankart tear. As the humeral head is dislocated posteriorly the anterior surface can impact onto the posterior edge of the glenoid creating a Reverse Hill-Sachs lesion
- A specific injury can occur to rugby players if they are diving forwards to score a try with the ball tucked under their arm. As they hit the ground with the point of their elbow their humeral head can be forced backwards out of the glenoid.
- Posterior dislocations are also associated with epileptic seizures and electric shock injuries.
- Ligamentous Laxity –
- some peoples’ tissues are more lax/stretchy than others. This tends to occur more often in females than males and in younger people. In certain cases the ligaments around the shoulder are so lax that they are unable to completely restrain the ball within the socket. This can result in subluxation or dislocation of the shoulder without a significant injury. When this does occur the ball can dislocate in any direction leading to mult-directional instability.
- Muscle Patterning Disorder –
- occasionally the complex sequence in which the groups of muscles work to stabilise the ball into the socket as the shoulder moves become disrupted. In this situation muscles that should be contracting, relax or aren’t strong enough whilst other muscles that should be relaxing, contract. This can result in the shoulder being ‘pulled’ out of the socket by this muscle imbalance. The static stabilisers of the shoulder are often completely intact.
In some cases of shoulder instability more than one of the above problems can be going on at the same time.
History
- Traumatic Dislocation - With traumatic dislocations a history of the exact incident, mechanism of injury, subsequent treatment and any further dislocations is important. Often patients do not present with a typical history of true or repetitive dislocations but may describe posterior joint pain or clicking. It is important to ascertain in exactly what position the arm is in when this occurs. It is usually when the arm is flexed and in internal rotation.
- Ligamentous Laxity & Muscle Patterning - Patients with ligamentous laxity or a muscle patterning problem usually have not had an initial traumatic event. Their problems tend to develop over time without a significant precipitating injury. Unlike traumatic dislocations the shoulder may be unstable in multiple directions. They may notice that their shoulder feels ‘apprehenisve’ in a number of different positions.
Patients with ligamentous laxity may also have problems with other joints. Ligamentous laxity may cause problems with the other shoulder, the knees, ankles and hips.
Examination
The clinical examination is the most important element of the diagnostic process. Unlike anterior instability, patients with posterior instability tend to not be ‘apprehensive’, which can make it harder to elicit clinical signs.
- It is initially important to assess for generalised ligamentous laxity for all patients with shoulder instability. The Bieghton Score is a simple assessment giving a score out of 9 for generalised joint laxity.
- As with all shoulder problems an initial general examination of both shoulders is undertaken looking for areas of pain, comparing the range of movement and for rotator cuff muscle strength.
- Special tests are then undertaken specifically to look for any instability in all directions.
Find out more about examination of the shoulder for instability…
Investigations
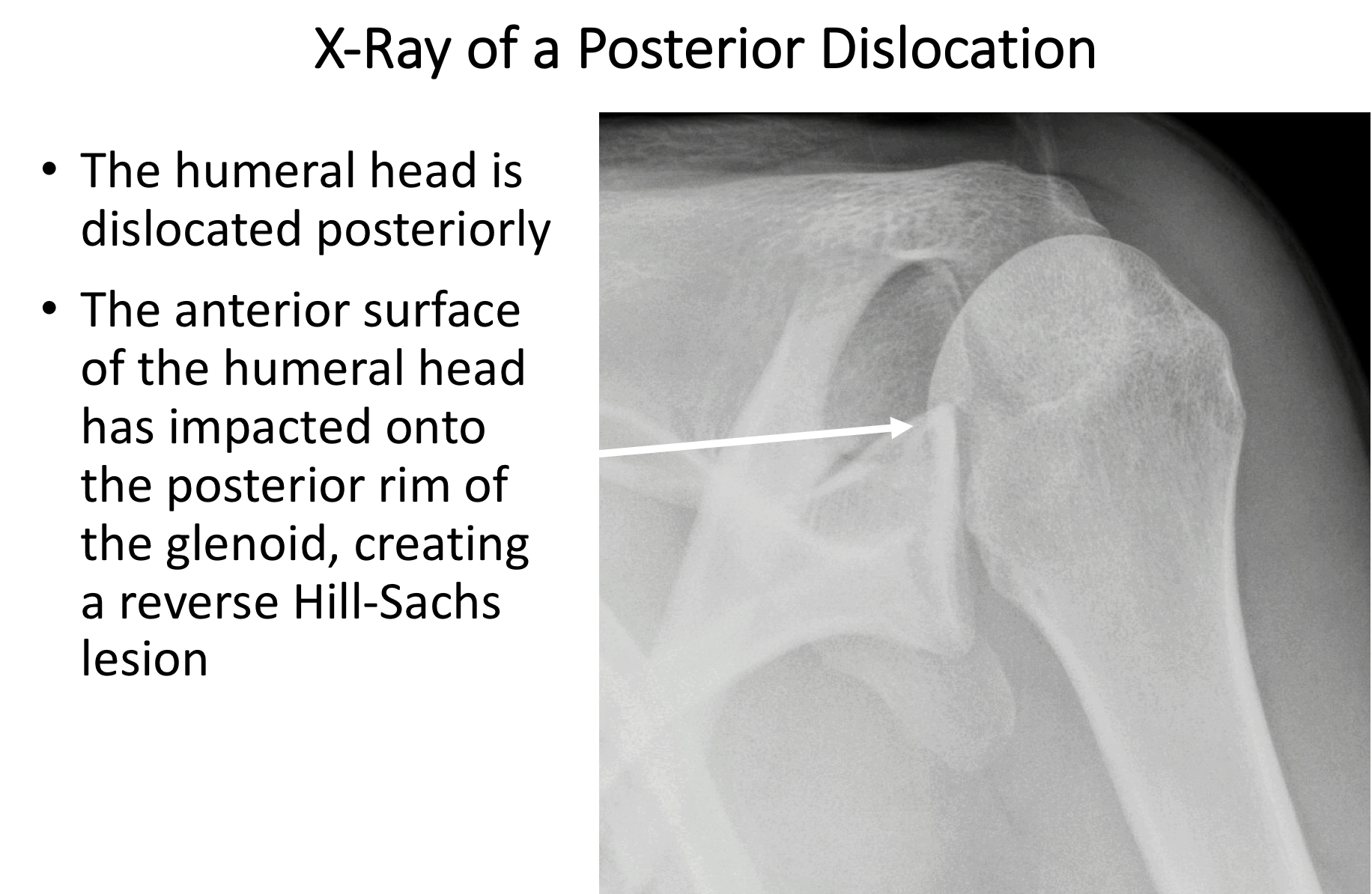
- X-Ray – Posterior shoulder instability is usually due to a problem with the soft-tissues around the shoulder, which are not visualised on a plain x-ray. However, patients with traumatic instability can damage the bones around the shoulder. The bone at the back of the glenoid can be broken or chipped as the humeral head is levered backwards out of the glenoid. This can create a bony Reverse Bankart lesion. The front of the humeral head can also be dented at the same time, creating a reveres Hill-Sachs lesion. This damage can sometimes be seen on x-rays taken at a special angle.
- MRI Scan – This is the best investigation to assess for shoulder instability. MRI scans are usually undertaken with the patient’s arm lying across their body. In this position the soft-tissue structures are under no strain and there is a possibility that the damaged capsule, ligaments or labrum happen to lie in the correct position and appear to be normal on the scan. To try and avoid this situation and enhance the sensitivity of the MRI scan a special ‘dye’ (Gadolinium) can be used. This can either be injected into the patient’s blood system via their arm (Indirect Arthrogram) or injected, under local anaesthetic, directly into the patient’s shoulder (Direct Arthrogram).
An MRI Arthrogram is a very good investigation to assess any damage to the labrum, capsule and ligaments of the shoulder and can also demonstrate any significant damage to the bones.
Find out more about shoulder MRI scans…
- CT Scan – A CT scan is a very good investigation to assess damage or injury to the bones around the shoulder. It is able to give 3-D images of the humeral head and glenoid. This can be very helpful where there is any concern about significant bone damage. It can then provide important information when deciding the best type of surgical treatment that might be required.
Treatment of Posterior Instability
This most important factor that determines how to best treat someone with a shoulder dislocation is whether it is due to a Traumatic Dislocation or Ligamentous Laxity/Muscle Patterning. Someone with a symptomatic Traumatic Dislocation will usually require some form of surgical repair and someone with Ligamentous Laxity or Muscle Patterning can usually be treated with a specialised rehabilitation programme supervised by a suitably experienced physiotherapist.
Surgery for Posterior Instability
Surgery for posterior instability depends on the injury and the level of on-going symptoms that the patient is experiencing. It is essential to assess the level of the patients symptoms and their exact pathology. The biggest determinant is whether the patient has a soft-tissue injury or a bony injury.
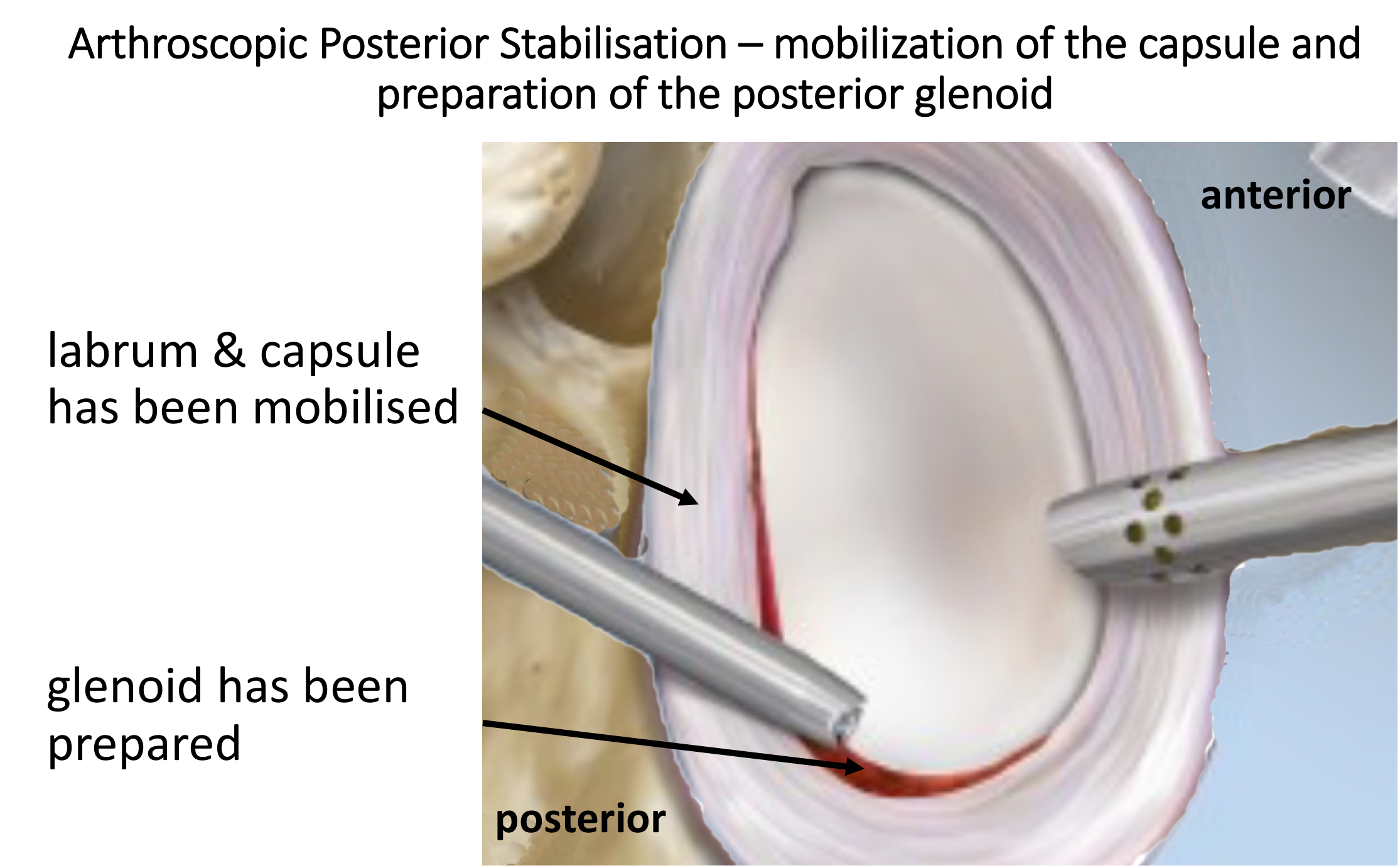
Arthroscopic Posterior Stabilisation (soft-tissue injury)
Essentially this involves mobilising and freshening up the torn edges of the ligament and capsule and then placating or re-attaching them on to the back of the Glenoid (Socket), the bone here having also been freshened. The tissue is usually attached to the bone using ‘suture anchors’. These are small implants, made of various materials, that can be inserted, by drill holes, into the bone. Attached to the anchors are sutures that can then be passed through the torn ligaments and capsule and tied down into position. Having re-attached the freshened ligaments and capsule to the freshened bone of the socket they can then heal.
I undertake all of my Posterior Stabilisations arthroscopically. There are a number of different variations to the technique and different implants that can be used. I have evolved my technique over the past 15 years, taking advantage of new implants and equipment, and have obtained consistently good results, with which I am happy. My routine Arthroscopic Posterior Stabilisation Procedure is described below,
Watch a video of an arthroscopic Posterior Repair….
Find out more about Arthroscopic Shoulder Surgery….
Procedure
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
- Prophylactic iv antibiotics are given
- A Trimano arm holder is used to hold the patient’s arm in external rotation
- A posterior, 1 - 2 anterior and a Wilmington portal are used for joint access
- The joint is initially assessed to confirm the presence of a Posterior Capsular Tear, to assess the extent of any Reverse Hill-Sachs Lesion or Glenoid Bone Loss and any other pathology
- The Posterior Capsular Tear is then fully mobilised and the tissues freshened
- The Posterior Glenoid is then prepared and freshened
- 3 Osteoraptor or Pushlok bio-composite anchors are inserted into the anterior, inferior glenoid and the capsule and ligaments re-attached with a superior shift
- The repair is assessed and the wounds closed
After the Surgery
Post-Operative Care
Following a Posterior Stabilisation the patient may be able to go home that day or may need to stay in the Hospital overnight, depending on circumstances. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team who will instruct them on how to take the sling on and off and the ‘safe zones’ of movement. Further physiotherapy will then be organised from the 3 week mark onwards.
Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month, 3 months and 6 months after their procedure to assess their progress and recovery.
Period of Sling Immobilisation & Rehabilitation Protocol
After an arthroscopic Posterior Stabilisation the patient’s arm needs to be in an External Rotation Brace for 3 weeks. It is initially important to ‘protect’ the repair from any significant load as it begins to heal whilst, at the same time, it is preferable to not allow the shoulder to get too stiff. The physiotherapists will instruct the patient on the ‘safe zones’ of movement out of their sling over this period.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
| Milestones | |
| Week 6 | Active range of movement at least 75% of normal |
| Week 12 | Full ROM, with minor loss of combined abduction and external rotation |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Contact Sport |
|
| Lifting |
|
| Work |
|
Success of Surgery, Risks & Complications
Success following an Arthroscopic Posterior Stabilisation has to be assessed slightly differently from other procedures. Rather than being able to measure how much better the shoulder is after the operation we are waiting for a further dislocation NOT to happen. By convention, for a stabilisation procedure to be considered successful, the patient needs to have had no episodes of instability for at least 2 years after their operation.
For a standard Arthroscopic Posterior Stabilisation>90% of patients’ shoulders will be stable 2 years after their surgery. For patients returning to contact sports this figure is decreased to > 80%.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Recurrence – The 2- year re-dislocation rate <10% (for Contact Athletes <20%)
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Management of Posterior Shoulder Instability with Bone Loss
In certain cases of traumatic posterior shoulder instability not only is there a Reverse Bankart tear to the capsule and ligament, but there is also significant bone loss at the back of the Glenoid (socket) and/or on the front of the Humeral Head (Reveres Hill-Sachs Lesion). This can result from either a particularly forceful initial dislocation or be due to repeated dislocations.
There is no precise amount of bone loss that will indicate whether a soft-tissue repair, on its own, will be sufficient to stabilise the shoulder. However, it is generally accepted that a loss of 25% or more of the posterior glenoid bone-stockwill significantly decrease the likely success of a Bankart repair. The best way to assess bone loss is on either and MRI scan or CT scan.
A number of different procedures have been described to treat Glenoid bone loss with varying success. The most popular and most successful procedures involve fixing a bone graft onto the back of the damaged Glenoid (Socket) to re-constitute the articular surface. I prefer to adopt this approach and usually take a Bone Graft from the hip to fill the defect at the back of the Glenoid. I am prefer to do these operations as an arthroscopic procedure. My standard procedure is described below.
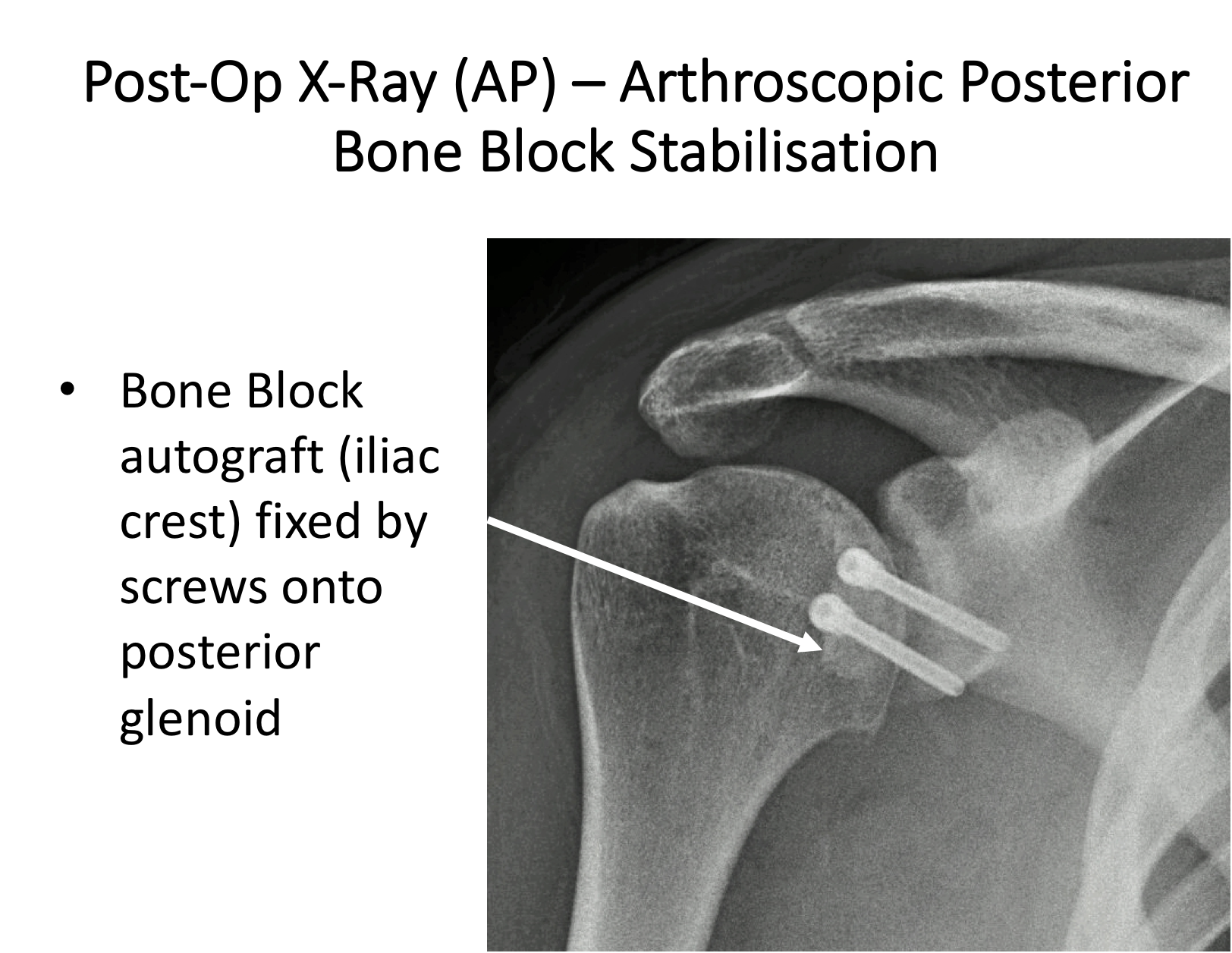
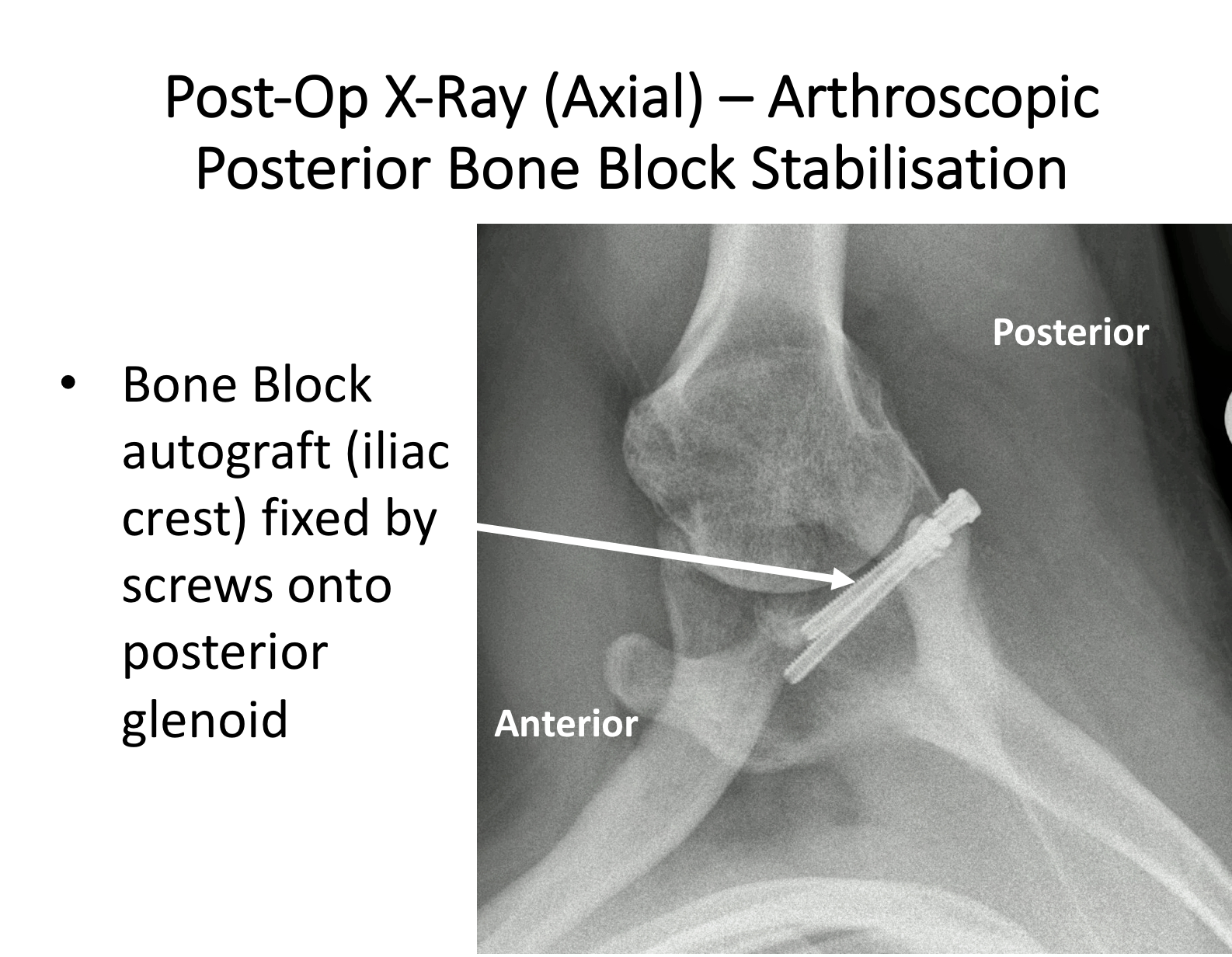
Arthroscopic Posterior Stabilisation (bone-loss)
The standard procedure uses a 1.5 – 2cm tri-cortical Bone Graft that is harvested from the Iliac Crest, which is the bone at the front of the hip. This is done through a 5cm incision just above the crest and, although sometimes painful for a time afterwards, does not usually lead to any detrimental function. The Bone Graft is then prepared with 2 drill holes and mounted onto a specific Bone Block guide.
The shoulder is then arthroscoped and the Posterior Glenoid defect prepared. Through a 3 cm longitudinal incision at the back of the shoulder the infraspinatus muscle is split and, under arthroscopic vision the bone block inserted into the joint. Once the bone block is in a satisfactory position, 2 guide-wires are drilled through the guide and bone block into the glenoid. The wires are then over-drilled with a 3 mm drill bit and two 4mm diameter cannulated, partially threaded screws inserted, securely fixing the bone block onto the back of the glenoid. Following this the posterior capsule is then re-attached to the native posterior glenoid using suture anchors. This exteriorises the bone block, protecting the humeral articular surface.
Watch a video of an arthroscopic Posterior Bone Block Procedure….
Find out more about Arthroscopic Shoulder Surgery….
After the Surgery
Post-Operative Care
Following a Posterior Stabilisation the patient may be able to go home that day or may need to stay in the Hospital overnight, depending on circumstances. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team who will instruct them on how to take the sling on and off and the ‘safe zones’ of movement. Further physiotherapy will then be organised from the 3 week mark onwards.
Find out more about Physiotherapy following Shoulder Surgery….
I would usually review patients in the clinic 1 month, 3 months and 6 months after their procedure to assess their progress and recovery.
Period of Sling Immobilisation & Rehabilitation Protocol
After an arthroscopic Posterior Stabilisation the patient’s arm needs to be in an External Rotation Brace for 3 weeks. It is initially important to ‘protect’ the repair from any significant load as it begins to heal whilst, at the same time, it is preferable to not allow the shoulder to get too stiff. The physiotherapists will instruct the patient on the ‘safe zones’ of movement out of their sling over this period.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 6 Weeks + |
|
| Milestones | |
| Week 6 | Active range of movement at least 75% of normal |
| Week 12 | Full ROM, with minor loss of combined abduction and external rotation |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Contact Sport |
|
| Lifting |
|
| Work |
|
Success of Surgery, Risks & Complications
Success following an Arthroscopic Posterior Stabilisation has to be assessed slightly differently from other procedures. Rather than being able to measure how much better the shoulder is after the operation we are waiting for a further dislocation NOT to happen. By convention, for a stabilisation procedure to be considered successful, the patient needs to have had no episodes of instability for at least 2 years after their operation.
For a standard Arthroscopic Posterior Stabilisation>90% of patients’ shoulders will be stable 2 years after their surgery. For patients returning to contact sports this figure is decreased to > 80%.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Recurrence – The 2- year re-dislocation rate <10% (for Contact Athletes <20%)
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system ….. (Patient Information – Outcome Measures)