Frozen Shoulder (Adhesive Capsulitis)
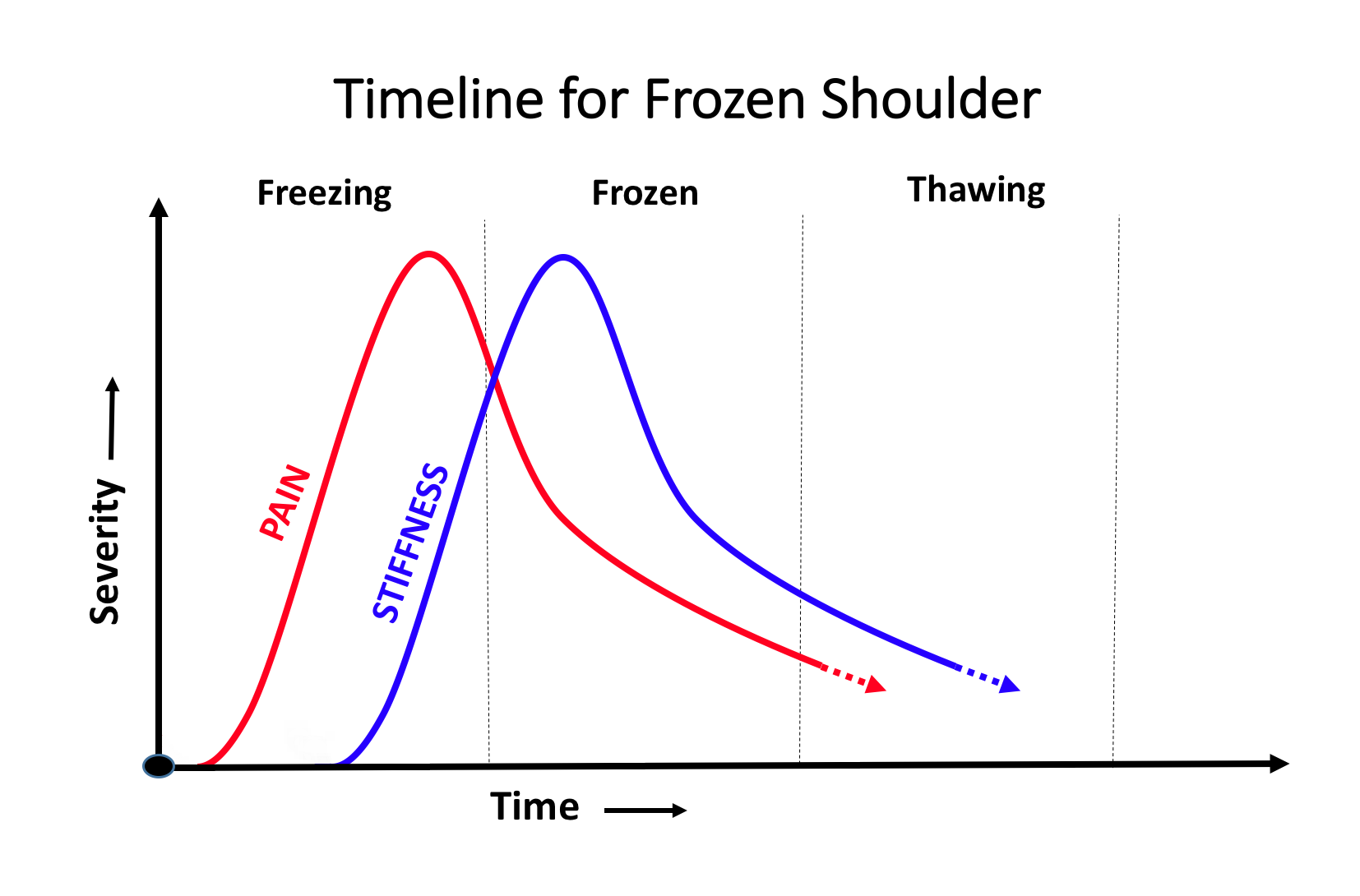
Frozen Shoulder can be a very uncomfortable condition where the shoulder becomes stiff and painful. It tends to affect people between the ages of 40 and 60 (although it can affect other ages) and usually more often women than men. It tends to progress through 3 stages – a Painful/Stiffening stage, a Frozen stage and finally a Thawing stage. The length of time for this process can vary from between 3 months and 3 years +!
What is affected?
-
Frozen Shoulder affects the capsule of the shoulder which becomes severely inflamed
-
the capsule is the innermost, thin lining of the joint
-
part of its job is to produce and contain the synovial fluid which lubricates the joint
-
it is usually very flexible, allowing the shoulder to move freely
-
-
NO other structures in the shoulder are usually affected – the articular cartilages, the muscles, ligaments and tendons are all entirely normal. However, over time due to stiffness, they can become very weak and tight
What happens?
-
a Frozen Shoulder occurs over 3 stages
-
Painful/Freezing Stage
-
initially, when a Frozen Shoulder develops, the capsule becomes very inflamed
-
it remains still flexible but extremely painful
-
patients can initially move their shoulder but it is painful all of the time, night and day, and over time stiffens up
-
in the early stages of Frozen Shoulder it can be difficult to differentiate it from other causes of a painful shoulder
-
-
Frozen Stage
-
over time the inflammation in the capsule settles down but it then becomes ‘scarred up’
-
the ‘scarred’ capsule is inflexible and prevents any movement at the shoulder joint
-
the pain slowly settles but the patient is left with a stiff/frozen shoulder
-
-
Thawing Stage
-
as time progresses the ‘scarred’ capsule recovers and begins to loosen up
-
over this time the patient’s shoulder begins to become more mobile again
-
however, the unaffected muscles, ligaments and tendons are weak and stiff and also have to recover
-
How long does a Frozen Shoulder last?
-
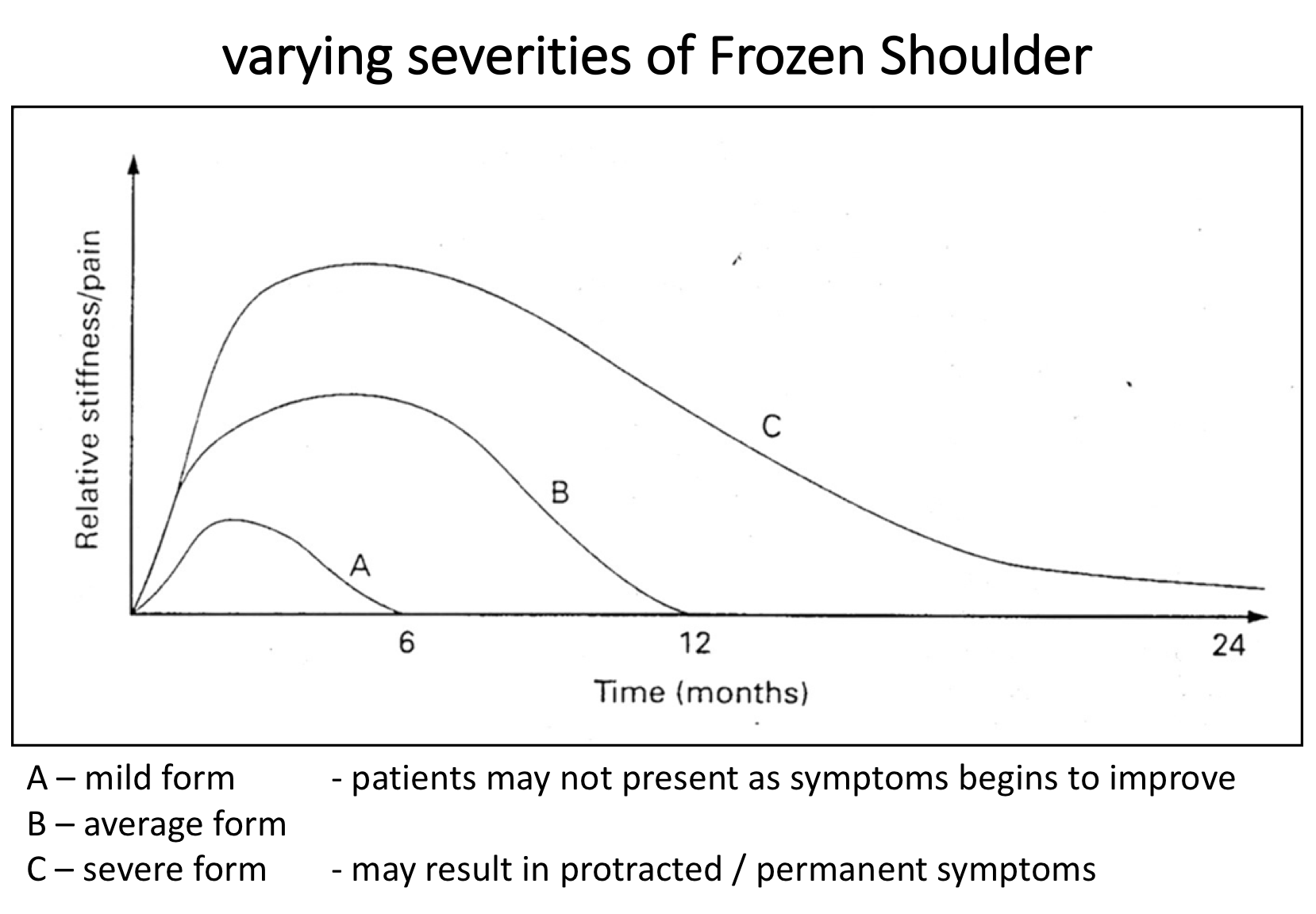
Frozen Shoulder seems to occur in varying severities
-
some Frozen Shoulders settle within 3 months
-
most Frozen Shoulders take 12 - 18 months to recover (6 months Freezing, 6 months Frozen, 6 months Thawing)
-
some severe Frozen Shoulders can last for up to 3 years or longer
Why does a Frozen Shoulder occur & who gets it?
-
we do not know why Frozen Shoulders occur
-
most Frozen Shoulders occur in people between 40 and 60 years of age, whose shoulders are otherwise normal
-
it tends to occur in women more often than men
-
sometimes an injury to the shoulder or another underlying shoulder problem can ‘spark off’ a Frozen Shoulder
-
people with Diabetes are more likely to develop a Frozen Shoulder and, when it does occur, it is often of a more severe type
Can you get a Frozen Shoulder on both sides & can it happen again?
-
it is possible to have a Frozen Shoulder on both sides, however they rarely occur at the same time
-
if you have a Frozen Shoulder on one side it does not usually mean that you are at an increased risk of having one on the other side
-
once you have had a Frozen Shoulder it is very rare that it will occur again on that side
Is it just a Frozen Shoulder?
-
most of the time a Frozen Shoulder occurs in an otherwise normal shoulder
-
sometimes a Frozen Shoulder can be ‘sparked off’ by a shoulder injury or another underlying problem (rotator cuff tendonitis / tear)
-
the symptoms from a Frozen Shoulder are usually so severe that they will ‘mask’ the symptoms from any other shoulder problem
-
as a general rule a patient needs to recover from the Frozen Shoulder before any other shoulder problems can be treated
How do you diagnose a Frozen Shoulder?
To diagnose & treat a Frozen Shoulder, like any other shoulder condition, requires a history, examination and investigations before deciding on an appropriate management plan. The best treatment for someone with a Frozen Shoulder can depend on which Stage their shoulder is in (Freezing, Frozen or Thawing), the severity of their symptoms and sometimes on other factors.
History
- occasionally a Frozen Shoulder can develop quickly, sometimes after a specific incident
- however, most of the time, a Frozen Shoulder develops gradually over time and people often do not initially realise that they have it. Some people think it is something else, others try and ignore it and some try to soldier on. As a result, patients can first present to the clinic at varying stages.
- Initially the shoulder is uncomfortable but over time becomes increasingly painful, to the point that it is there constantly day and, particularly, night. The pain can be isolated to the shoulder but can often radiate up into the neck and down into the arm. The shoulder becomes increasingly painful and stiff to move. Sudden jolts are particularly painful. Painkillers often do not work and people find it very difficult to sleep.
- A Frozen Shoulder can often make people very miserable and chronically tired
- an important part of the history is to check for any other possible causes for these symptoms
Examination
- the examination findings of someone with a Frozen Shoulder can vary differently depending on the severity of their symptoms and the Stage of their Frozen Shoulder
- Freezing Stage – although the shoulder is painful on movement there is usually no specific pain on palpation around the shoulder. Most of the movements around the shoulder are painful, particularly towards the end of range, but have been retained. Unless there are associated rotator cuff problems, testing for instability or rotator cuff symptoms is usually normal
- Frozen Stage – there is often still fairly significant pain on attempted movements but these are often restricted. Patients often find it very difficult to put their hand behind their back, even to reach their pocket. Movements to the side are often significantly restricted. Patients can usually elevate their arm forward up to shoulder height but often do so by shrugging their shoulder up. This is because whilst there is minimal movement at the Gleno-Humeral joint (shoulder joint) they can still move their Scapula (shoulder blade) on their chest wall. Some patients begin to develop pain around the scapula muscles and neck due to this exaggerated movement.
find out more about examination of the shoulder …..
Investigations
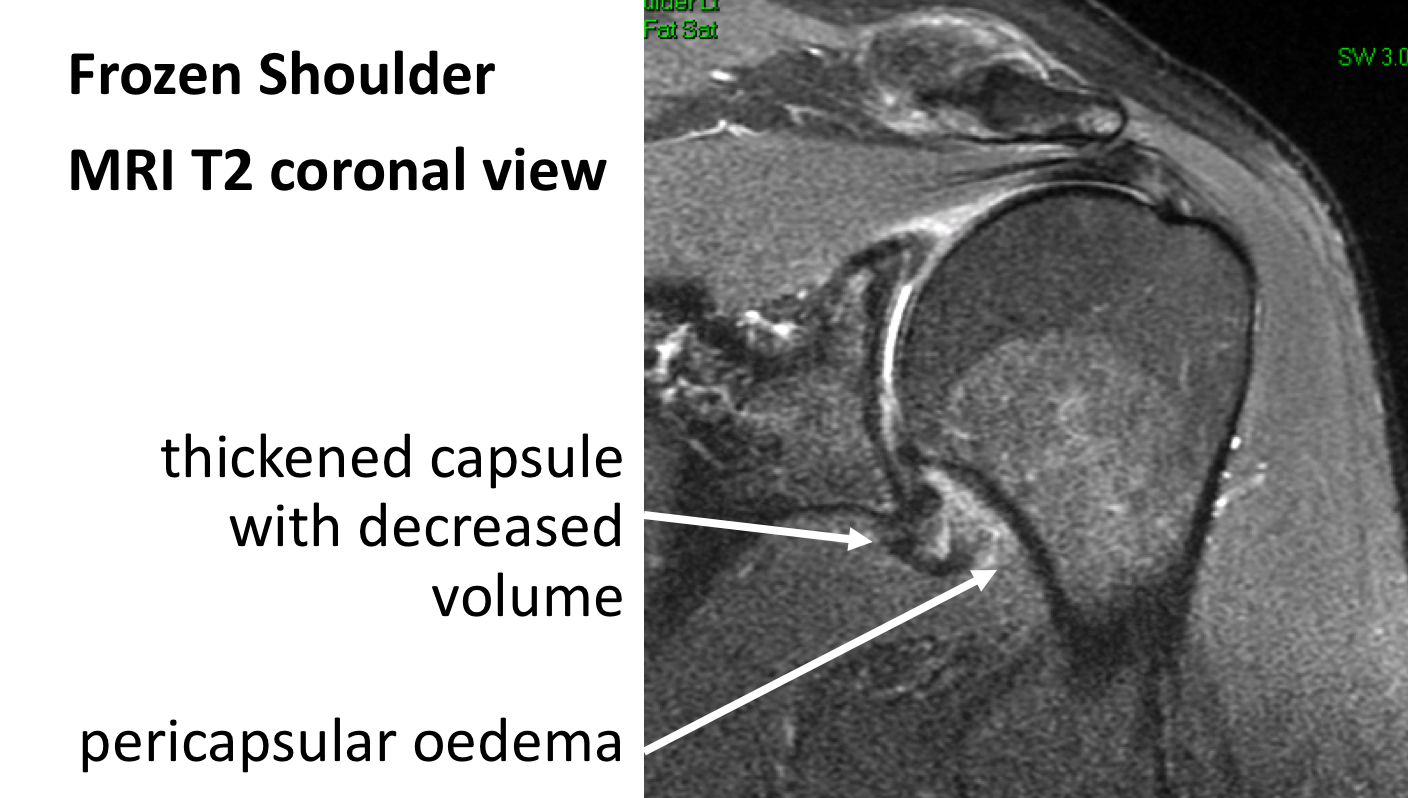
- Frozen Shoulder only affects the joint capsule, which is very difficult to visualize on any type of scans and tests. The main reason for undertaking investigations is to ‘rule out’ any other possible cause for the symptoms or to look for any other associated problems
- X-Ray – another cause of a painful stiff shoulder is arthritis. A plain x-ray is a useful investigation to rule this out and see whether they might be any previous boney injuries or clues. A plain x-ray can also show evidence of a calcific tendonitis that can be associated with a Frozen Shoulder
Find out more about X-Rays of the shoulder ….
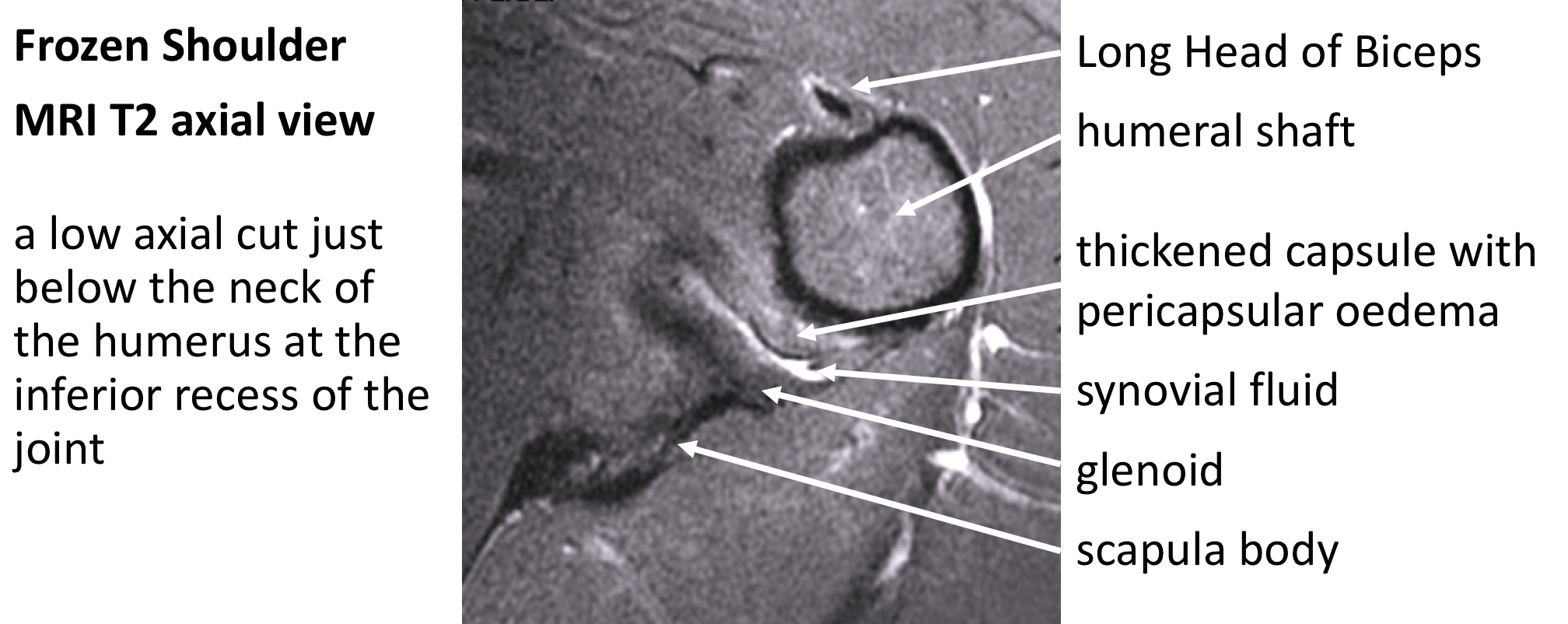
- MRI Scan– an MRI scan is the most useful investigation to look for any other causes or conditions that might be with a Frozen Shoulder.It can detect any rotator cuff problems, evidence of early arthritis or a bony injury. In severe cases of Frozen Shoulder an MRI scan can show evidence of capsular thickening or of associated per-capsular oedema.
Find out more about MRI scans of the shoulder….
Treatment for Frozen Shoulder
- Frozen Shoulder is an inflammatory condition and, as of yet, there is no medication available to actually stop this process
- However, there are a number of possible treatments for a Frozen Shoulder
- The most appropriate treatment for a particular patient depends on the Stage of the Frozen Shoulder
Analgesia/Pain Relief
- pain is the most severe problem associated with a Frozen Shoulder, particularly in the Freezing Stage
- there are no medals for bravery for a patient with a Frozen Shoulder
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response, they are useful at all Stages of Frozen Shoulder
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
- Nociceptive Analgesics –
- Nociceptive pain killers work on nerve generated pain
- Amitriptyline in lower doses works as a nociceptive pain killer. It has a useful side-effect in that it can make patients drowsy
- in cases of severe pain Amitriptyline can be prescribed at night
Physiotherapy
- physiotherapy can be very useful at certain Stages of a Frozen Shoulder
- in the early stages of a Frozen Shoulder, where it may not actually be evident that a Frozen Shoulder is developing, physiotherapy can be of some use
- when the Freezing Stage of a Frozen Shoulder has become established and the shoulder is very painful and stiffening up, there is no benefit in physiotherapy. In fact forcing the shoulder to move may make it more painful and delay recovery
- towards the end of the Freezing Stage and in the established Thawing Stage physiotherapy is very useful. It will help to stretch out the recovering capsule and improve movement. It is also important to stretch and re-strengthen all of the muscles and tendons around the shoulder that have not been working for a while
Find out more about Shoulder Physiotherapy….
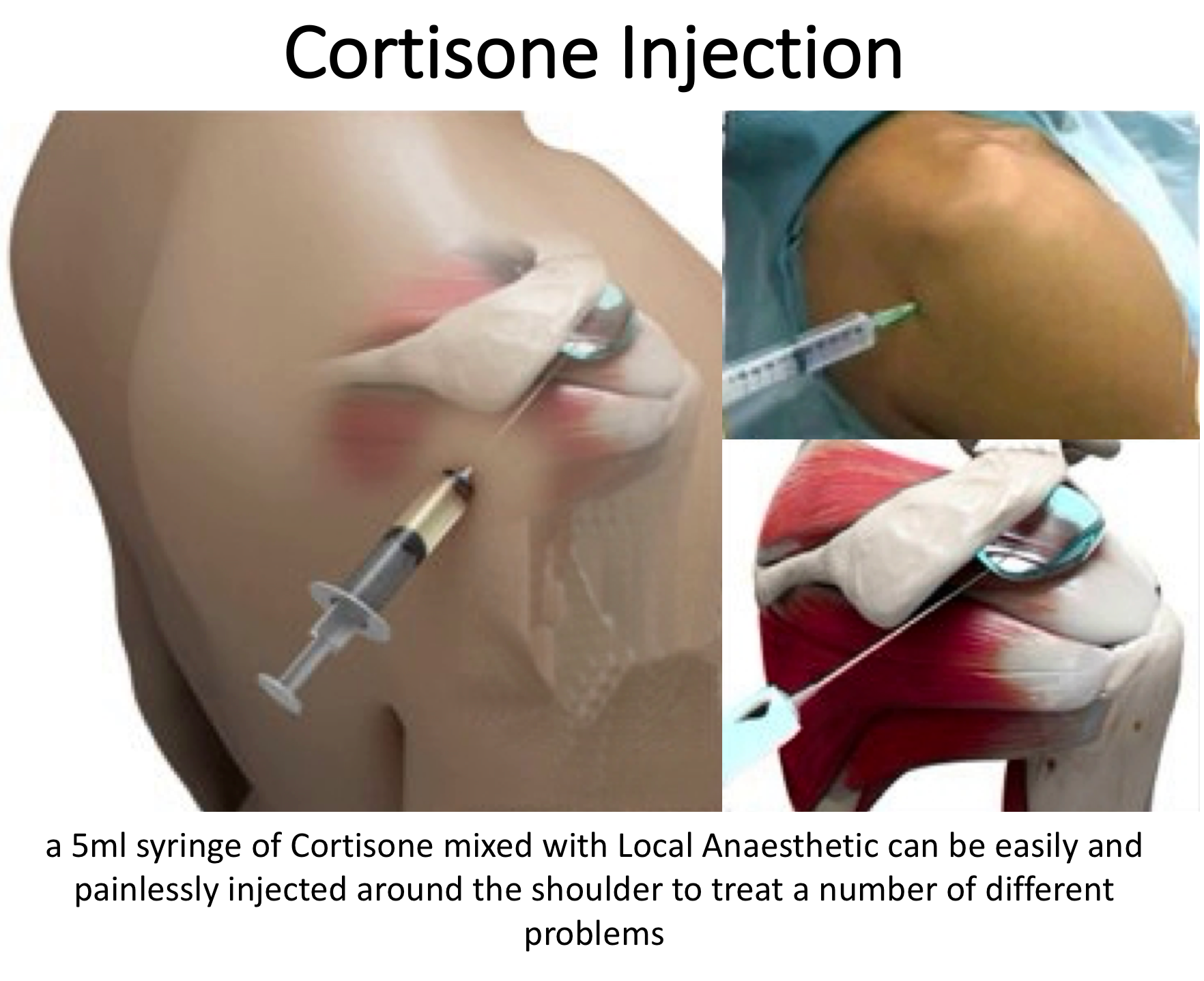
Cortisone Injection
- Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the Shoulder & Subacromial space it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- a Cortisone injection can be very helpful at all Stages of a Frozen Shoulder
- it can usually be injected simply in the Out-Patient Clinic
- it can often take several days to have an effect
- the risks of a single Cortisone injection are very small, however multiple injections are not advised
Capsular Hydrodistension/Hydrodilatation/Arthrographic Distension
- Capsular Hydrodistension of the shoulder is a relatively new and can be a very effective treatment in the Freezing & Frozen Stages of Frozen Shoulder. It can also be of some benefit in a resistant Thawing Stage
- Capsular Hydrodistension is an outpatient procedure undertaken by the radiologists and usually takes 15 to 30 minutes
- the Radiologist initially puts some local anaesthetic into the patient’s shoulder
- using either x-ray imaging or ultrasound scan the Radiologist inserts a small needle into the patient’s glenohumeral joint (shoulder joint)
- under imaging, a solution of warm normal saline with some contrast is injected into the shoulder. The injected fluid can be seen to expand the joint capsule. Usually between 20 – 40 ml of fluid can be injected
- distension of the glenohumeral joint is thought to disrupt adhesions within the joint and stretch out the scar tissue, encouraging it to resorb
- the results from a Capsular Hydrodistension are usually very good with 90% of patients gaining a significant improvement in their pain and an 80% improvement with movement
- the speed with which a Capsular Hydrodistension works can vary from within a couple of hours to a week or two
- after a Capsular Hydrodistension it is very important that the patient undergoes aggressive physiotherapy to regain strength and movement
Find out more about Physiotherapy following Hydrodistension….
Surgery for Frozen Shoulder
- some cases of Frozen Shoulder can be extremely severe and resistant to all treatments. This can often be the case in patients with Diabetes
- for resistant cases of Frozen Shoulder an Arthroscopic Capsular Release can make a significant difference
- an Arthroscopic Capsular Release can be done in the Frozen & Thawing Stage of a resistant Frozen Shoulder
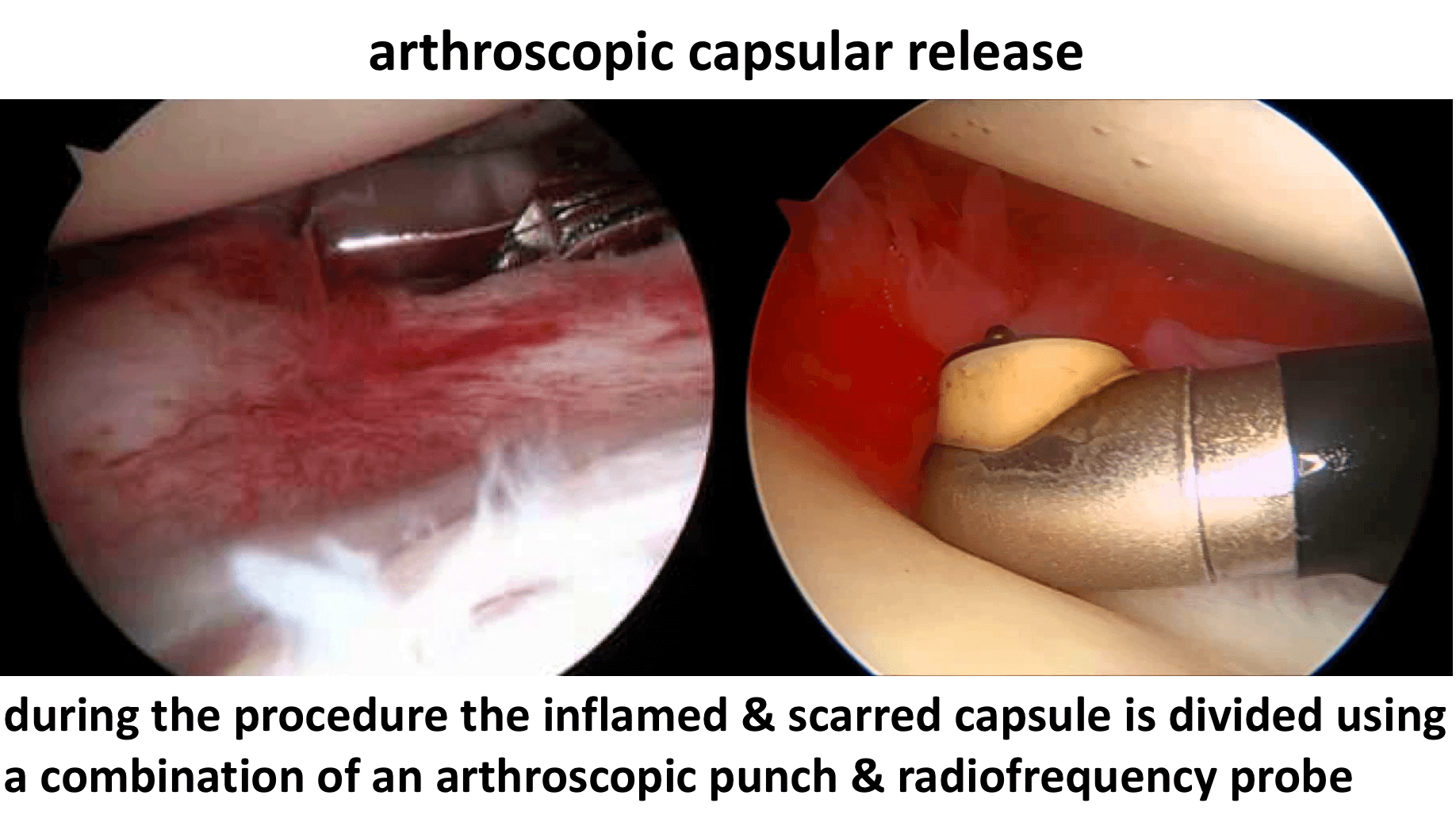
Arthroscopic Capsular Release
An Arthroscopic Capsular Release is usually done as an In-Patient procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to circumferentially release the scar tissue from around the whole shoulder and tidy up the rest of the joint. At the same time the rest of the shoulder can be assessed and an Arthroscopic Subacromial Decompression undertaken. After the surgery it is essential to keep the shoulder as mobile as possible to prevent the scar tissue reforming. The procedure is undertaken using a general anaesthetic, an interscaelane nerve block and an additional pain pump. The pain pump contains 250ml of local anaesthetic and is connected to the shoulder through a small 2mm diameter tube. The pump delivers a constant flow of local anaesthetic into the shoulder for the next few days, keeping the shoulder comfortable. The next day the Physiotherapists take the patient through several intensive sessions of physiotherapy to help maintain the recovered range of motion and to regain strength. My routine Arthroscopic Capsular Release Procedure is described below,
Watch a video of an Arthroscopic Capsular Release….
Find out more about Arthroscopic Shoulder Surgery…
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
- A posterior and a single lateral portal are used to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- The Glenohumeral Joint is initially assessed to assess for the extent of the capsular contracture and any other associated problems, in particular, the Rotator Cuff and the Long Head of Biceps
- An anterior portal is then created and an extensive capsular release undertaken using a combination of an arthroscopic punch, shaver and radiofrequency probe (Fig 7)
- The Subacromial Space is then entered and the undersurface of the Acromion identified.
- A lateral portal is then created
- Using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the Subacromial Spur.
- A powered burr is then used to resect about 5mm of bone from the undersurface of the acromion
- The Decompression is then assessed to check that sufficient bone has been resected
- The tube for the Subacromial Pain Pump is then inserted
- If any significant damage is found to the Rotator Cuff this will be then also be repaired
- The Subacromial Space is then washed out and the wounds closed with sub-cuticular sutures
Find out more about having an operation…
After the Surgery
Post-Operative Care
Following an Arthroscopic Capsular Release the patient usually stays in the hospital overnight. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further follow-up. The patient will be seen by the In-Patient Physiotherapy team and undergo several sessions of intensive physiotherapy before going home. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following Shoulder Surgery…
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, the patients arm is kept elevated in a sling, for protection and to prevent any contractures reforming. After the nerve block has worn off the arm can be taken out of the sling and the physiotherapy and mobilisation can start. I encourage patients to try and use their shoulders as much as possible to try and regain movement.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person. My advice to most patients is to try and organise to be off of work for 1 – 2 weeks after the surgery. This is so that they can be as diligent as possible in doing their exercises. The physiotherapsits would usually recommend that patients initially do exercises every hour that they are awake.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic Capsular Release is usually a very successful procedure but, because the surgery only releases the capsule and contractures within the shoulder, it usually takes between 3 – 6 months for the muscles, ligaments and tendons to fully recover and for the Shoulder to return to normal. Often patients do not obtain a complete recovery of all shoulder movements but gain a more than functional range of motion. For a standard Arthroscopic Capsular Release >95% of patients’ will be happy with their shoulders after 6 months.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
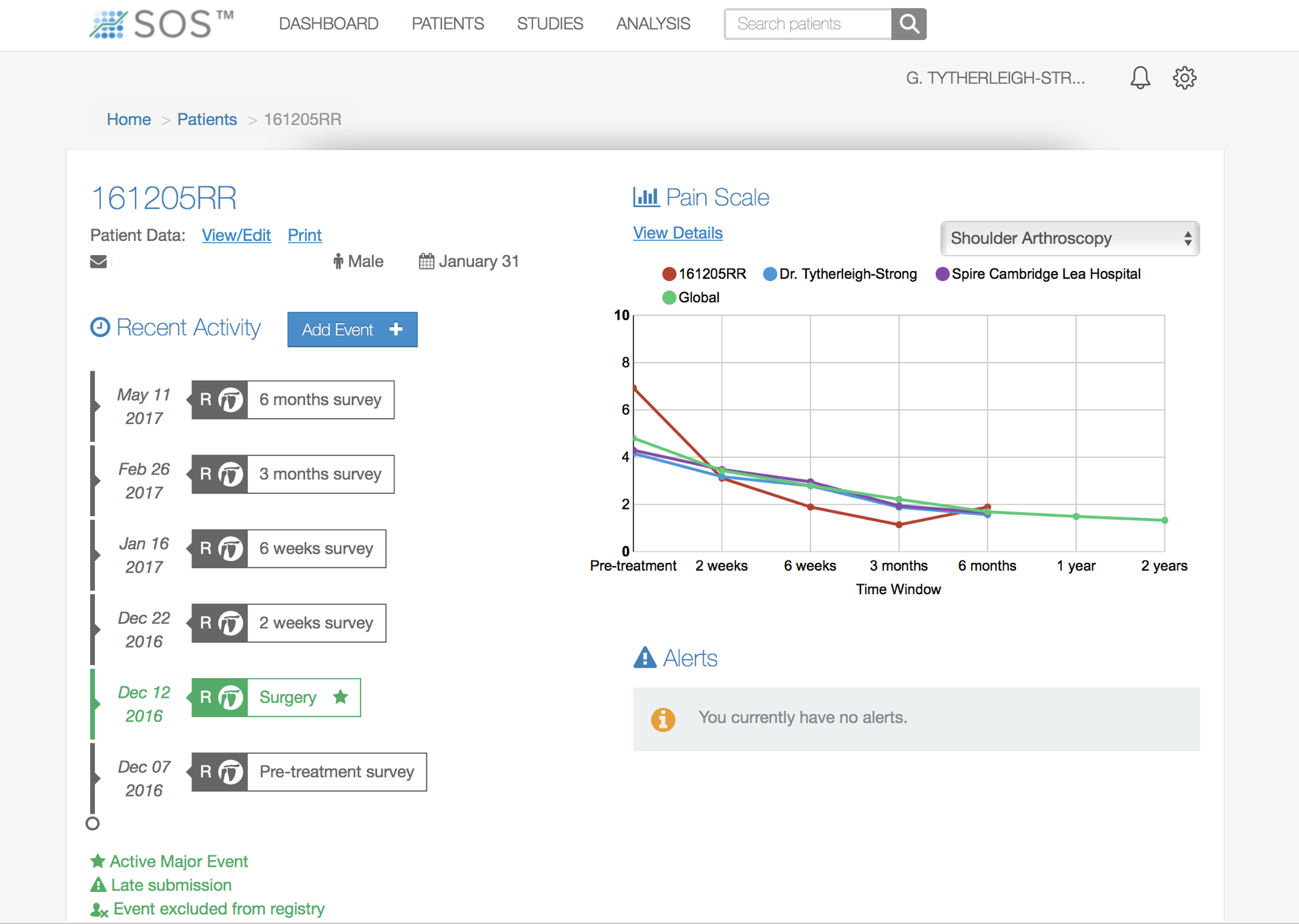
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system …..