Clavicle Anatomy
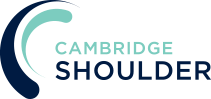
- The clavicle is an S-shaped flat bone that is the only horizontal long bone in the body
- It is located between and connects the sternum (ribcage) and the scapula (shoulder blade)
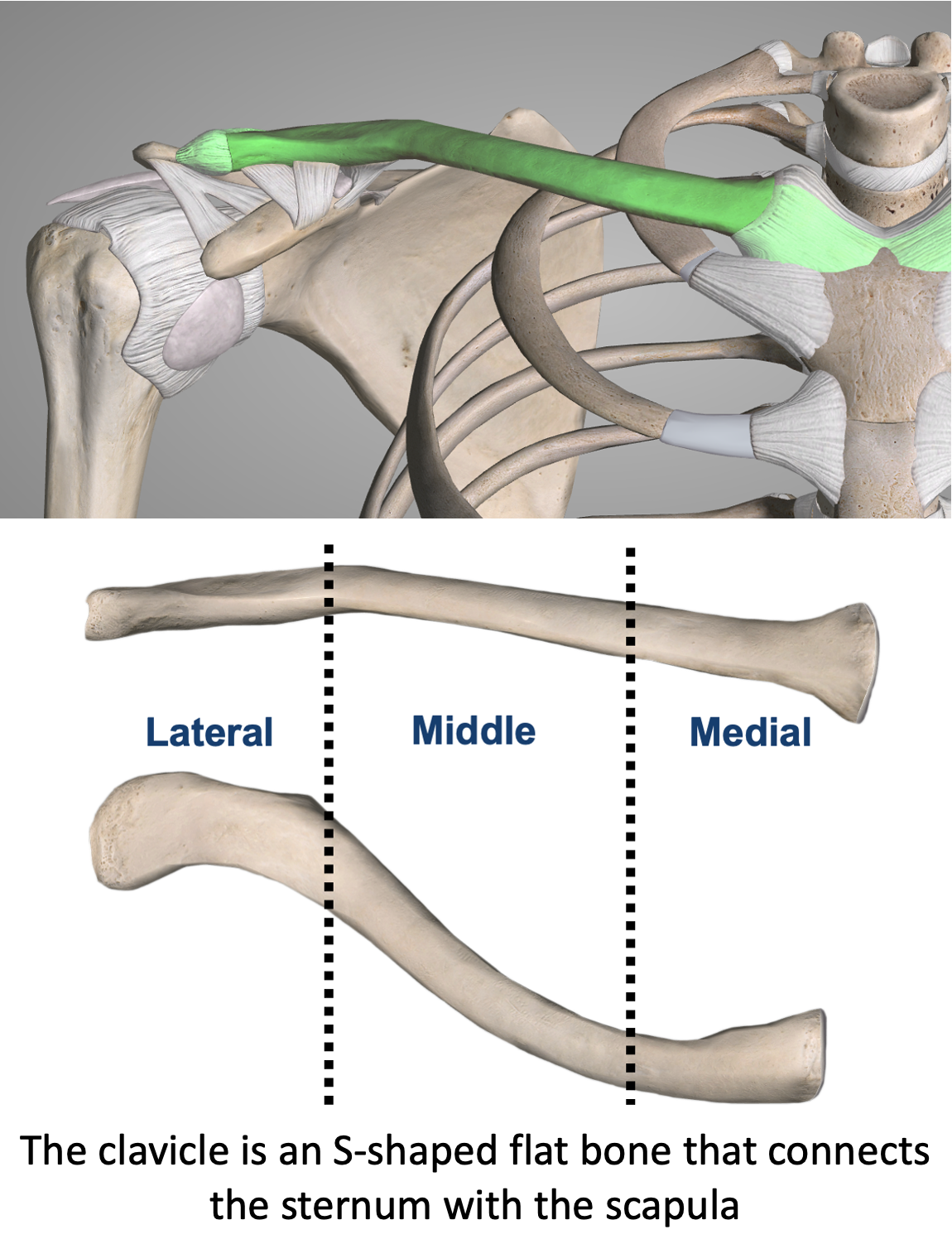
- Not all mammals have a clavicle! Animals that run, swim or graze (such as a lion) do not have clavicles. However, animals that climb and position their arms in space (prehensile animals) such has humans and monkeys have a clavicle
- It is the bone that ‘struts’ out the shoulder and allows the arm to be elevated and ABducted
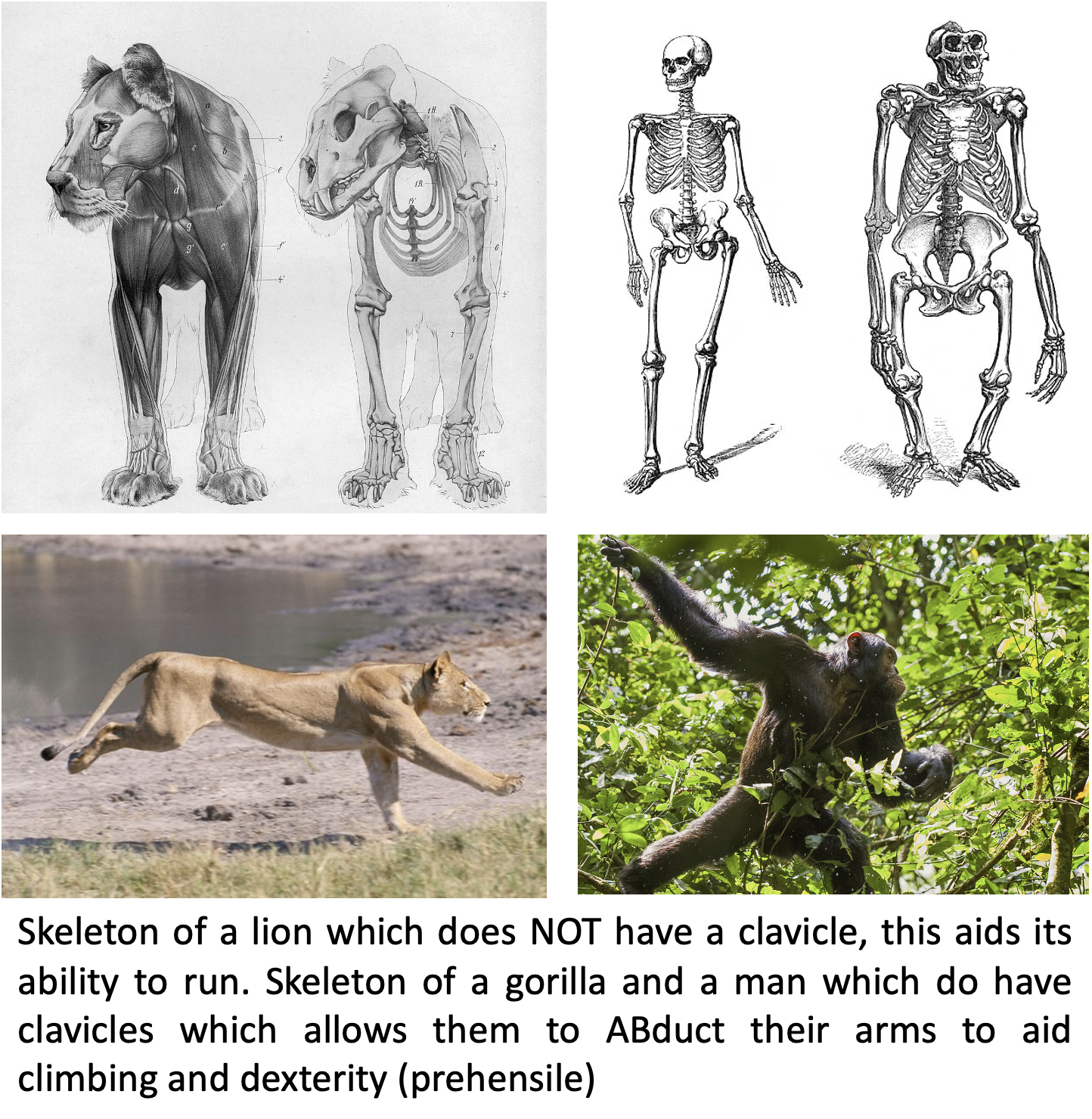
- It is the bone that connects the arm to the body and transmits all of the forces from the upper limb to the axial skeleton
- The sternoclavicular (SCJ) and acromioclavicualar (ACJ) joints connect either end of the clavicle. Due to the small surface area of these joints and the large forces that they transmit, they are particularly prone to osteoartrhritis
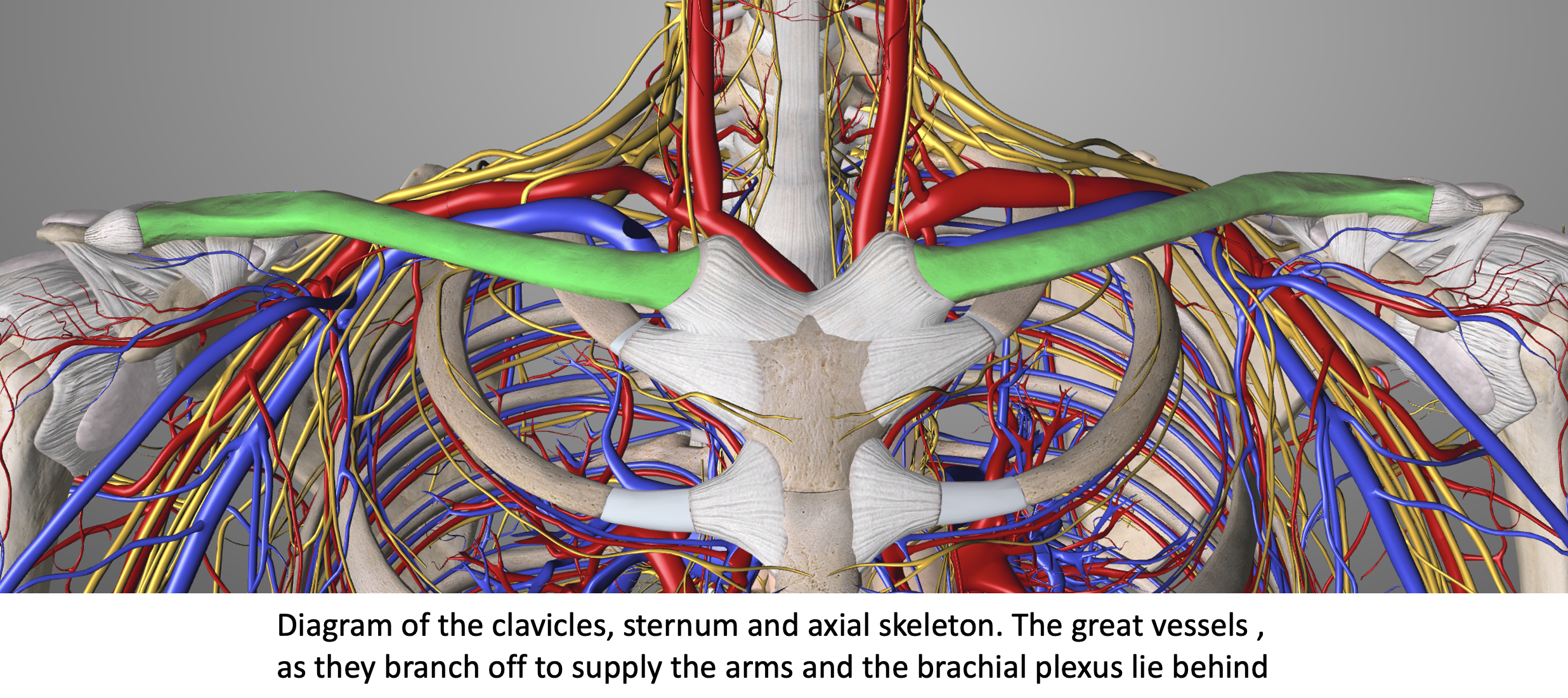
- The clavicle lies above several important arteries, veins and nerves that supply the upper limb
- Although these vital structures are rarely injured when a fracture occurs, it is always important to take them into consideration
Clavicle Fractures (Broken Collarbone)
-
- A clavicle fracture is a break in the collarbone, one of the main bones in the shoulder
- The clavicle is the mostly commonly broken bone around the shoulder and accounts for about 5% of all adult fractures
- A clavicle fracture can be extremely painful making it difficult to move the arm and to lie down flat
- Most clavicle fractures can be treated non-operatively with initial immobilisation in a sling
- However, some clavicle fractures due to either the position of the broken bones, associated injuries or the needs of the patient can be treated with surgical fixation
- Mechanism of Injury (Causes)
- Clavicle fractures can be caused by a,
- direct injury - onto the bone, such as a rugby tackle
- indirect injury - such as fall from a bike or a horse onto the shoulder and the force being transmitted down the clavicle which breaks
Types of Clavicle Fractures
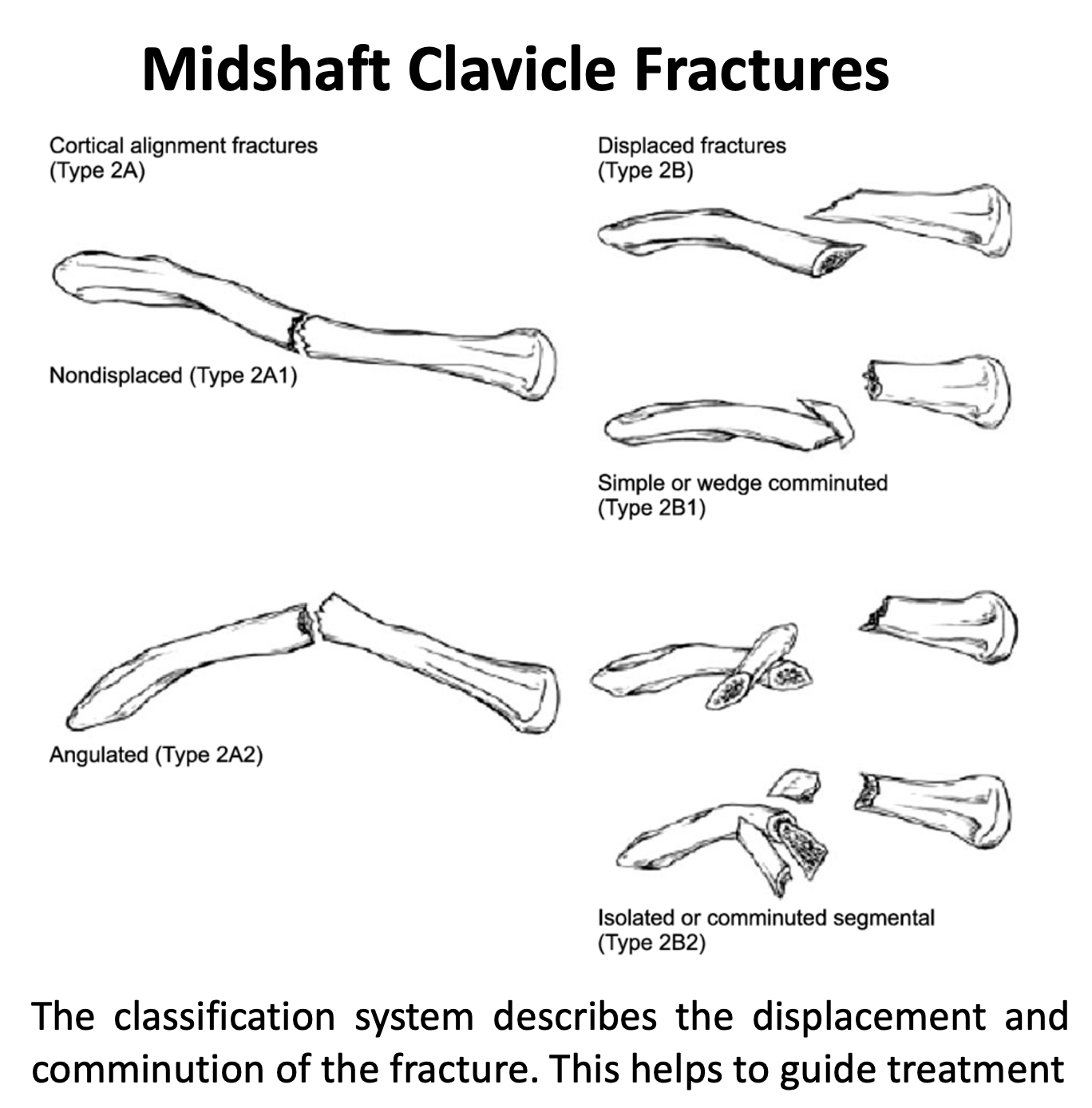
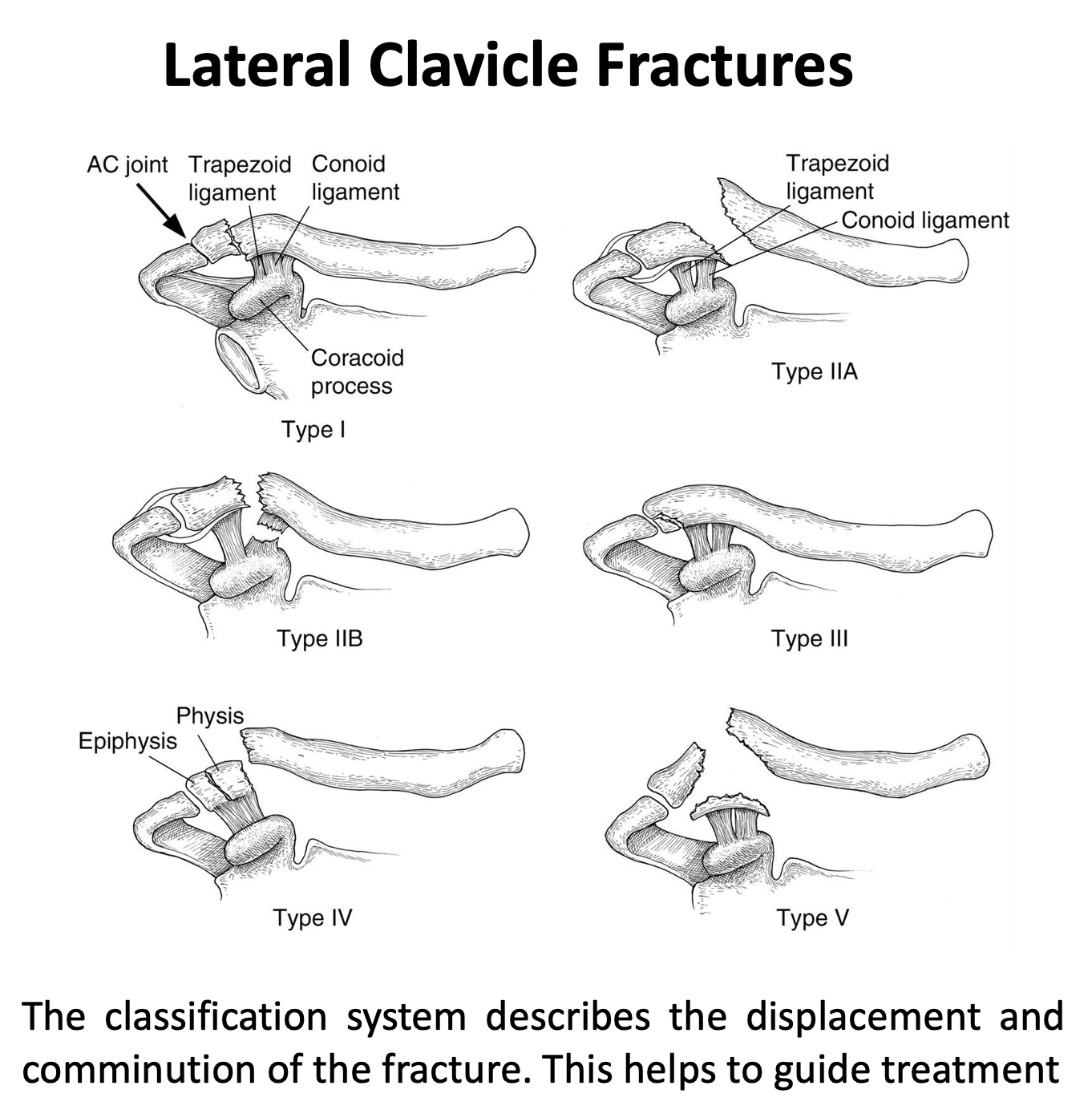
- The purpose of most classification systems is to help guide what is likely to be the outcome of the injury and to guide the best treatment
- Clavicle fractures are classified in a number of different ways
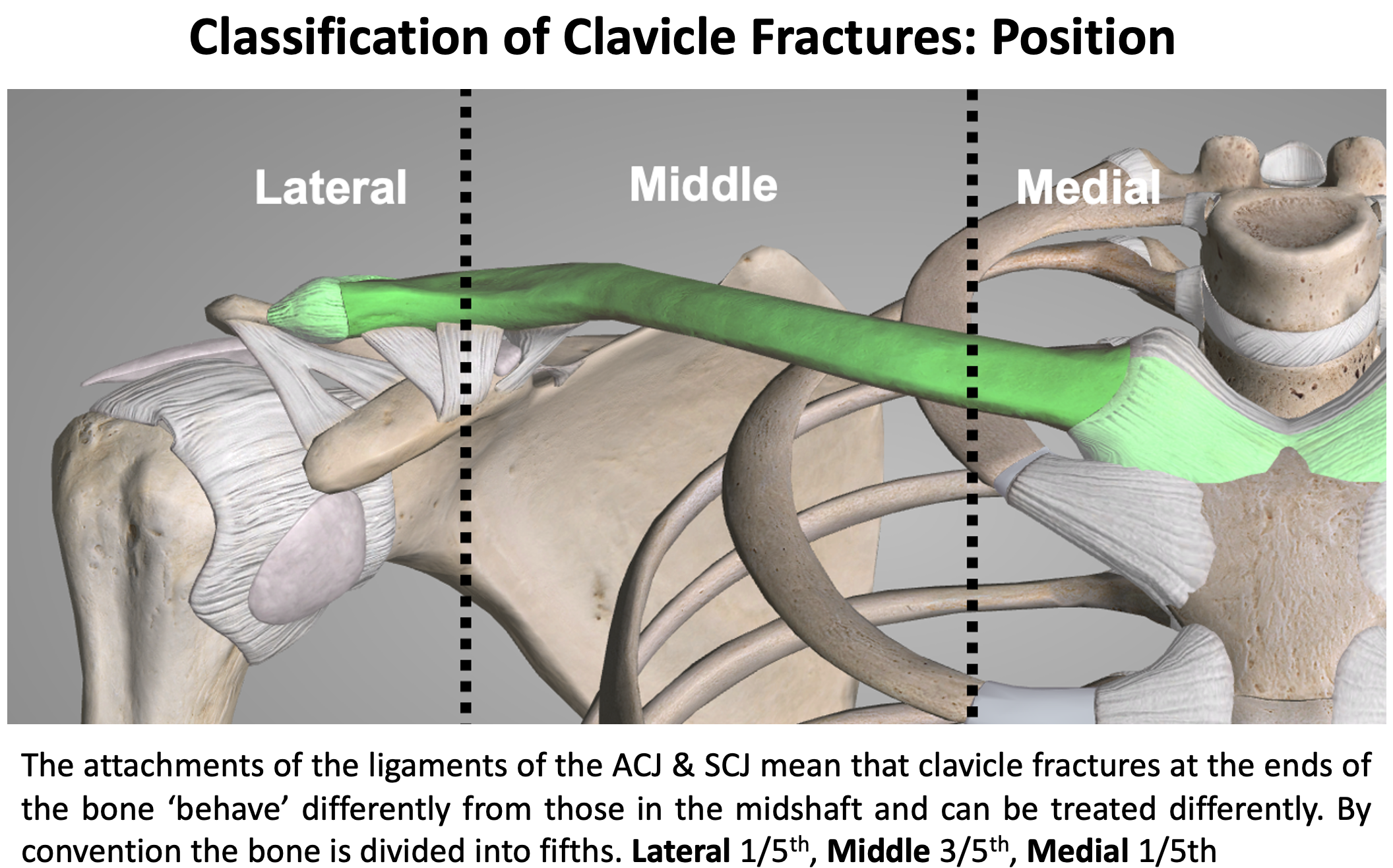
- the location of the fracture along the bone
- anatomically the clavicle is divided into equal thirds
- for the purpose of fracture classification, the clavicle is divided into an outer/lateral 1/5th, a middle 3/5th & an inner/medial 1/5th
- the reason for this is that the attachments of the coracoclavicular ligaments at the ACJ and the costoclavicular ligaments at the SCJ generally mean that fractures in this area are often less displaced but, if the ligaments are involved, need to be treated differently
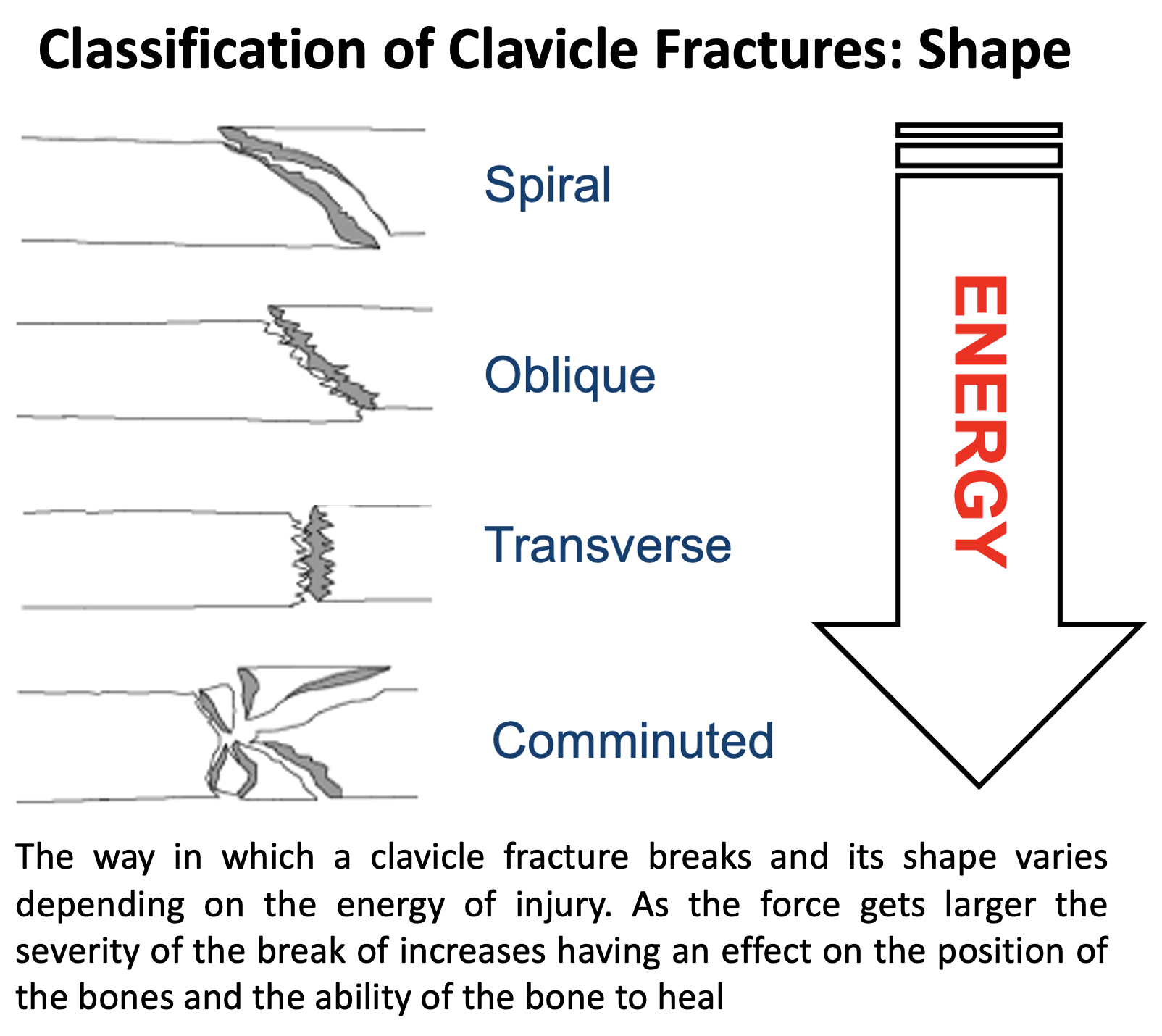
- the shape of the fracture
- the shape of the fracture is an indication of the ‘mechanism of injury’ and the likelihood of how easily the fracture will heal
- a spiral fracture occurs from a twisting force, an oblique fracture occurs from an indirect force, a transverse fracture occurs from a direct force and a comminuted fracture (broken into multiple pieces) occurs from a larger direct force
- these ascending fracture patterns are caused by an increasingly large force. The larger the force the more potential damage can occur to the bone and the surrounding soft tissues
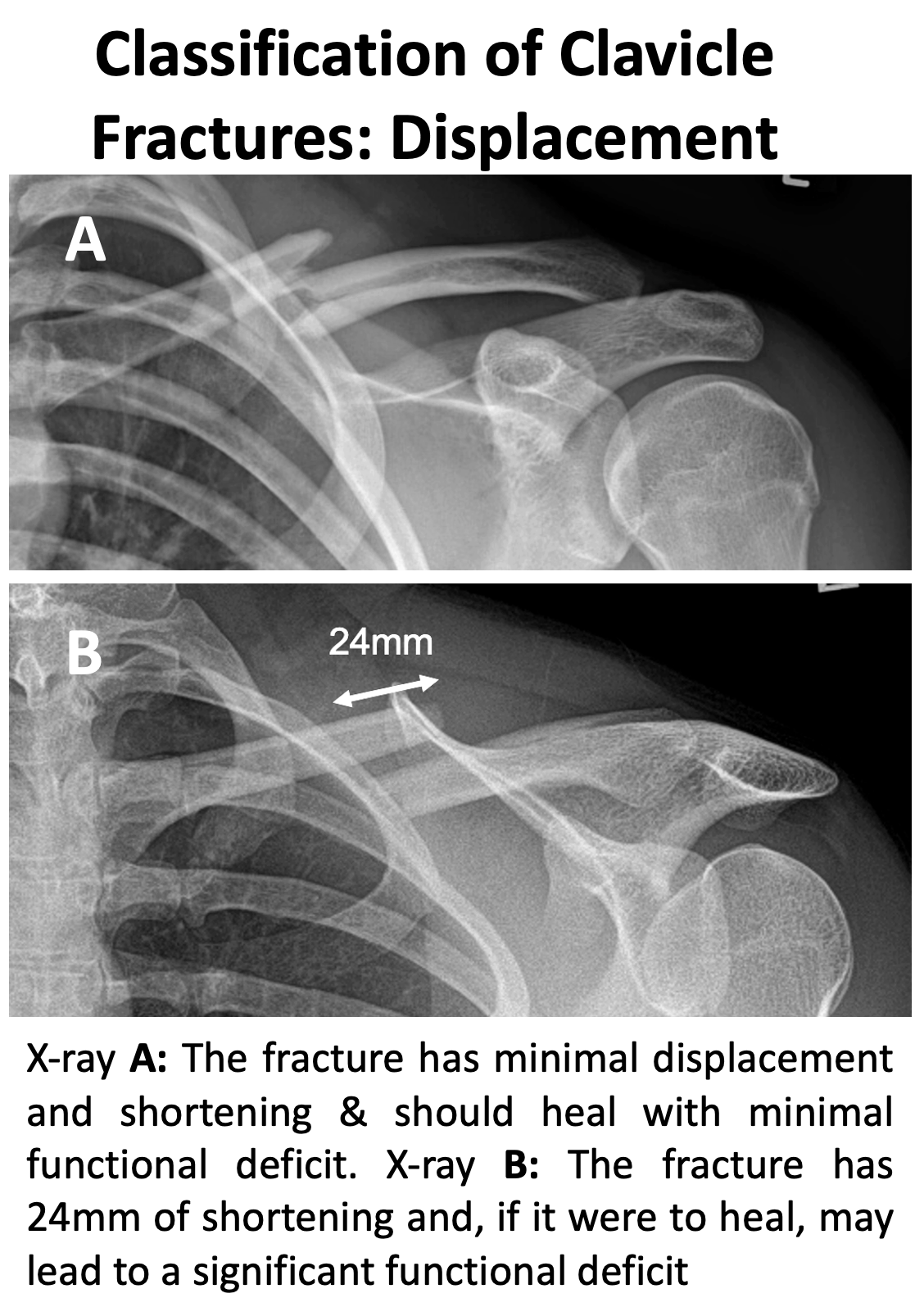
- the displacement of the fracture
- clavicle fractures can be angulated or increasingly displaced
- there is an element of ‘remodelling’ as a clavicle fracture heals, much more so in younger patients, and so some fracture positions can be treated non-operatively
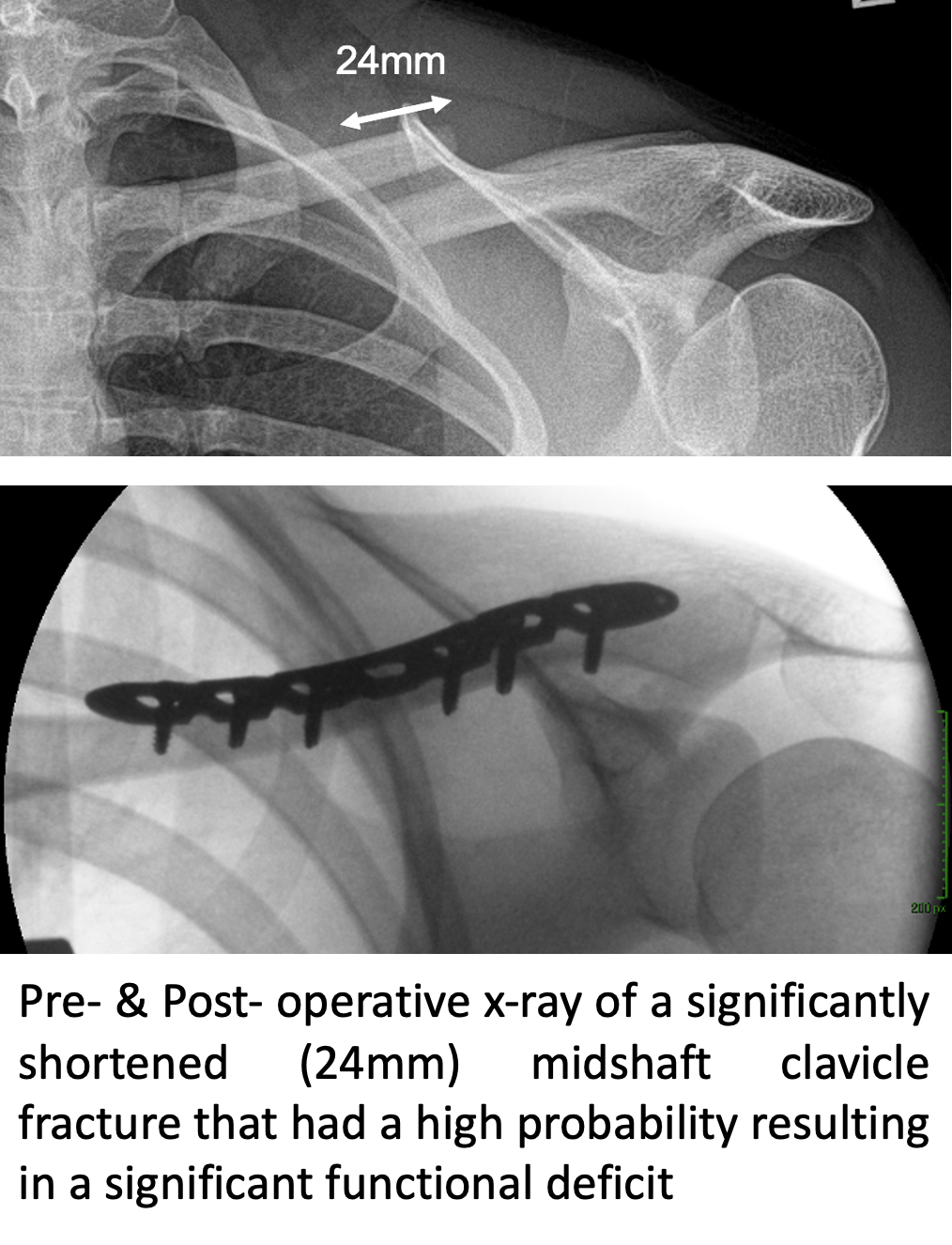
- if there is significant displacement of the fracture ends the fracture may heal as a ‘malunion’ which can, in certain circumstances, cause a significant functional deficit
- the location of the fracture along the bone
- Classification Systems – there are a number of classification systems for mid-shaft, lateral-end and medial-end clavicle fractures that are used to help with the management of clavicle fractures
Clavicle Fracture Healing
- Most simple clavicle fractures will heal
- However, some clavicle fractures can take a long time to heal (Delayed-Union) and some fractures will not heal at all (Non-Union)
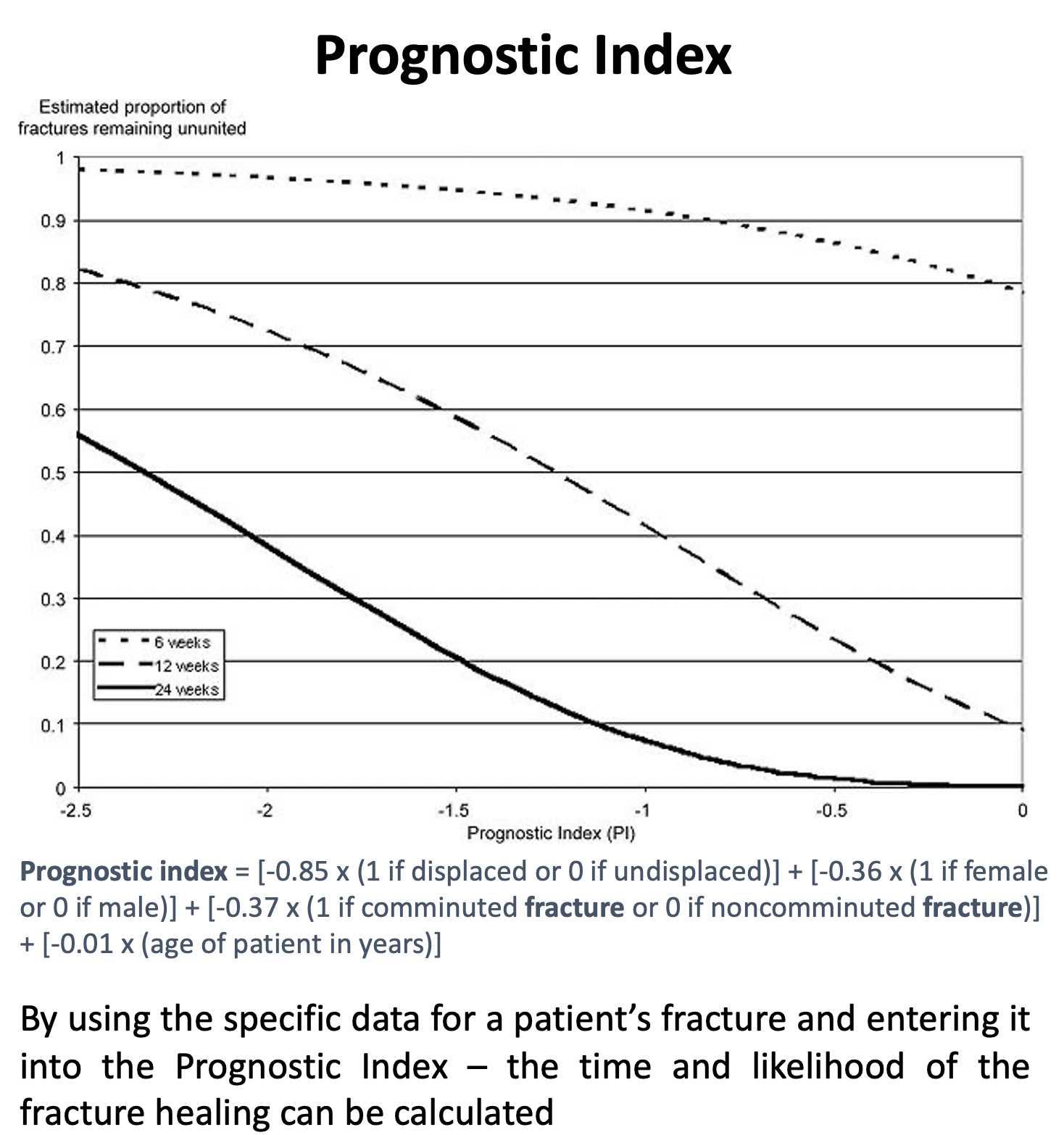
- Based on research looking at a large number of patients with previous clavicle fractures a Prognostic Indicator table has been produced that, taking into account a number of key factors (type & displacement of the fracture, patient age, patient sex & smoking), can predict the likelihood and speed of a particular clavicle fracture healing
Diagnosis of Clavicle Fractures
- To diagnose & treat a clavicle fracture, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. When a clavicle fracture has occurred as part of a major accident the priority is to treat any life-threatening or more major injuries first. The best treatment for a particular patient with a clavicle fracture can depend on the severity of their symptoms and other associated shoulder conditions.
- Clavicle fractures can be caused by a,
History
- In most cases of a clavicle there has been a significant injury where the patient has either landed or been hit on the point of their shoulder
- Following an acute injury, it is initially important to check for any other more significant associated injuries which includes neurological symptoms related to possible damage to the Brachial Plexus
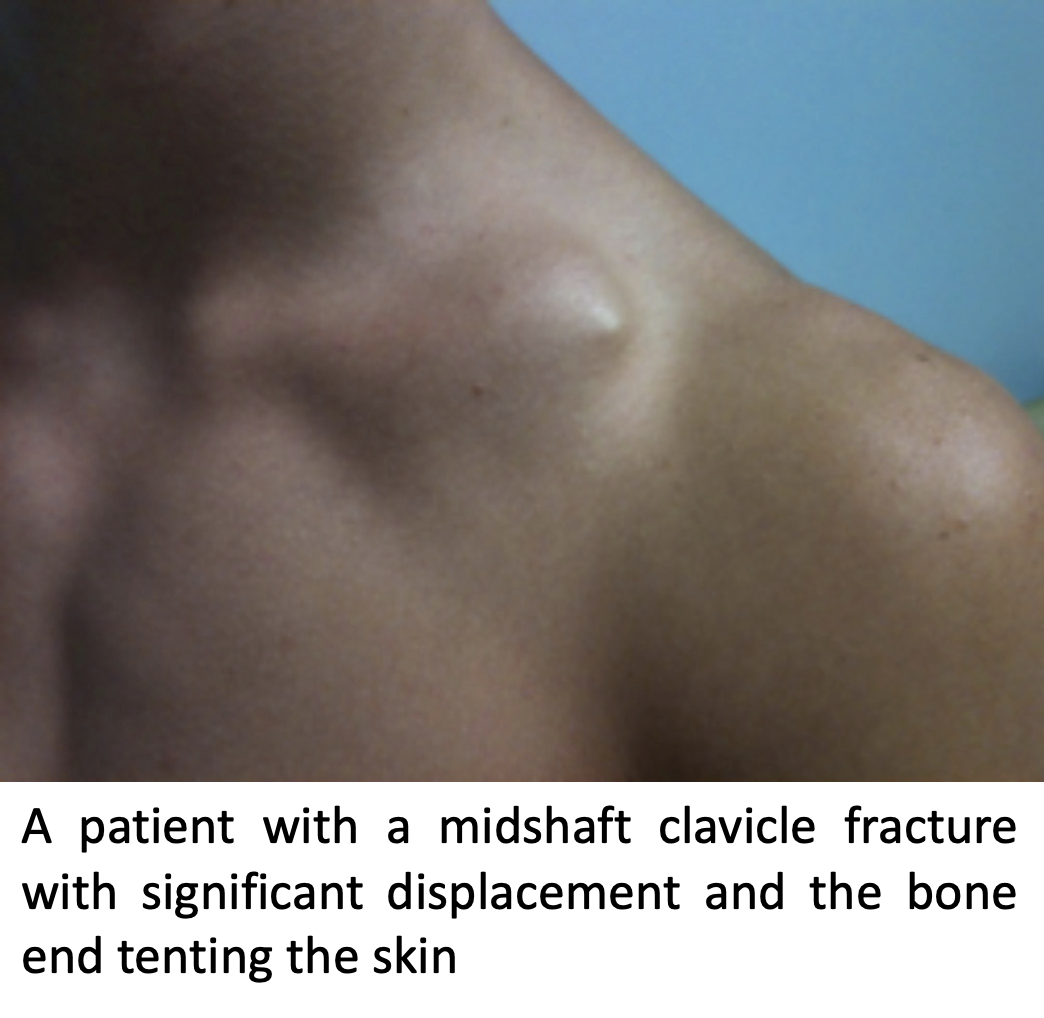
- The main symptom is of pain with an associated prominence of the fracture and tenting of the skin
- In more chronic cases there may also be associated problems with prominence at the fracture and shoulder and scapula (shoulder blade) function due to pain and weakness
Examination
- The patient usually is usually supporting their arm with the shoulder in ADduction
- In acute cases there maybe associated grazing, or even a laceration, over the ends of the fracture
- Bruising, which can spread down the chest, tends to appear after a few days
- In acute cases, due to the severity of the pain, it maybe difficult to assess shoulder and scapula function
- Sometimes, due to displacement and shortening at the fracture site, the glenohumeral joint and scapula can be rotated forward into protraction. This can lead to problems with both glenohumeral and scapulothoracic function (Scapular Dyskinesia)
Investigations
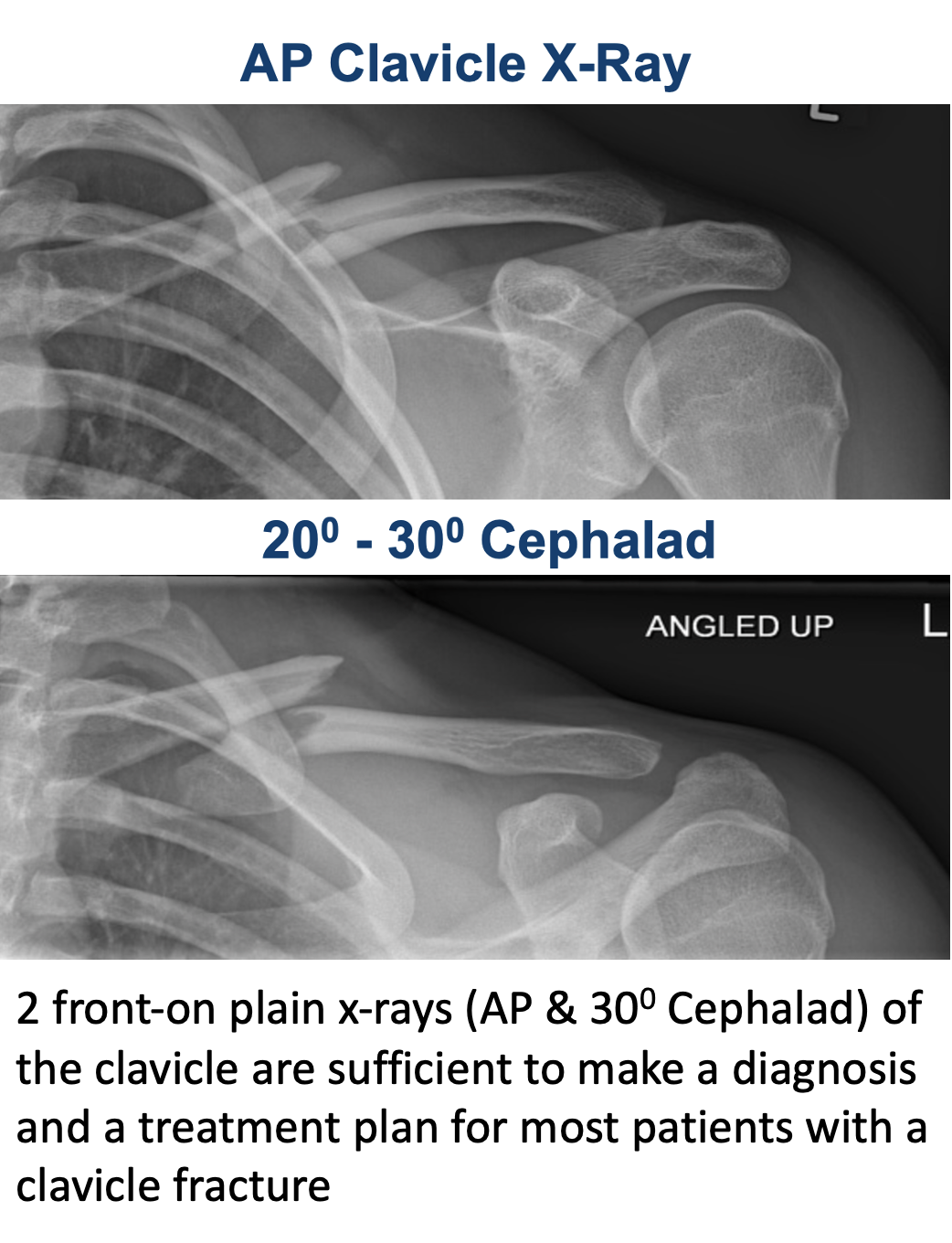
- X-Ray – generally, all the information that is required to diagnose and treat a clavicle fracture can be obtained from an x-ray
- an additional AP view of the clavicle taken at a 300 angle upwards gives a better assessment of the fracture displacement
- serial x-rays can be used to assess the position of the healing of the fracture. However, it can take several months before any evidence of a healing callus can be seen
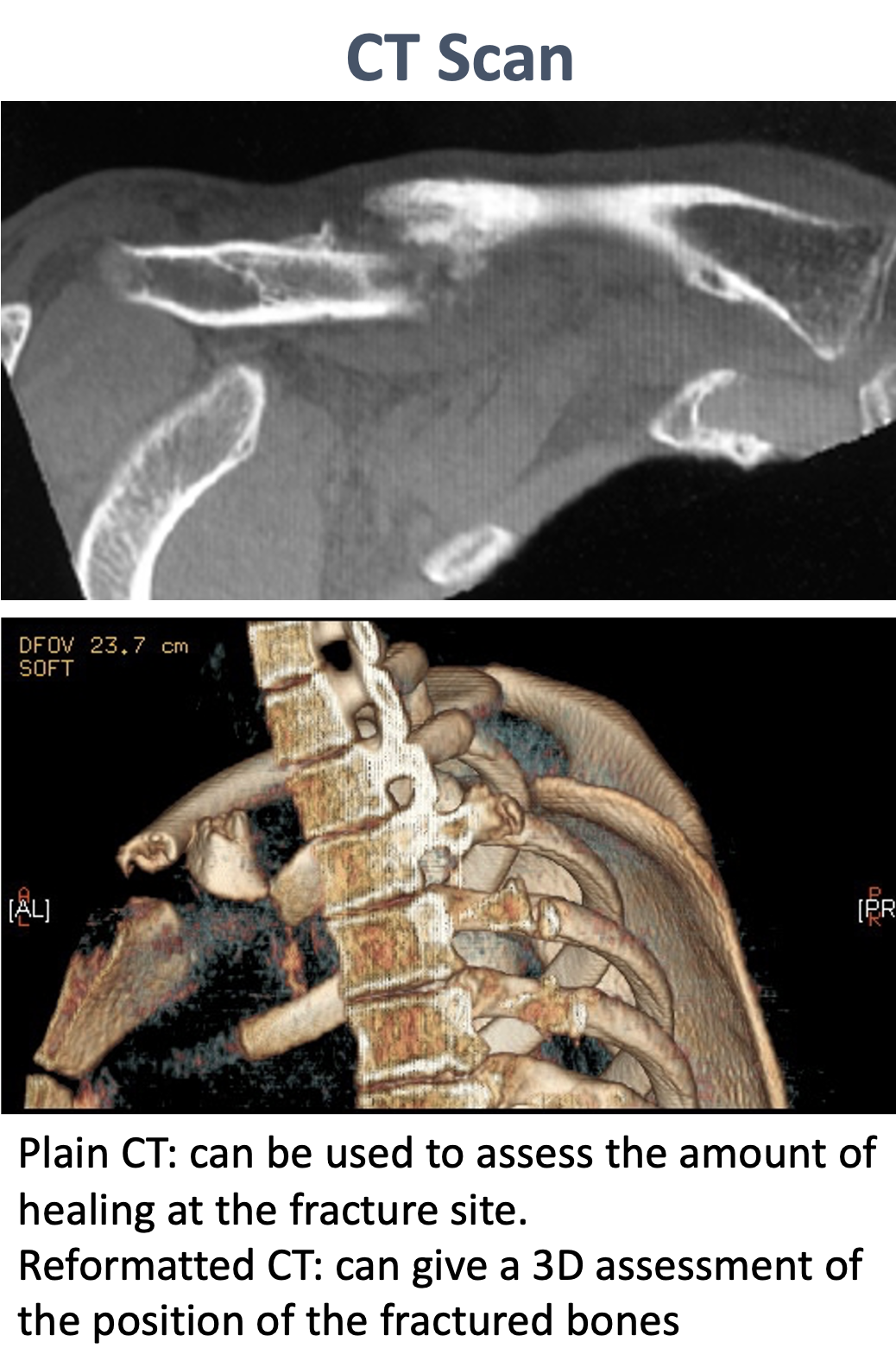
- CT Scan –
- occasionally CT scans are required acutely to assess the position of the fragments in a particularly comminuted fracture
- CT scans are generally used to assess healing at the fracture site, if there is any concern on the serial plain x-rays
Treatment of Clavicle Fractures
- There are a number of factors that need to be taken into consideration when treating a patient with a clavicle fracture
- Firstly, a clavicle fracture is not an immediately life-threatening injury and there is generally a couple of weeks before a delay in ‘definitive’ treatment will have a potential detrimental effect on the final outcome
- Factors that need to be taken into consideration are,
- the position, type and displacement of the fracture
- the likelihood of the fracture NOT healing
- the likelihood of the fracture healing in a position that will potentially have a detrimental effect on shoulder function
- the speed of recovery (how quickly the patient needs to recover to full function)
- cosmesis
- a patient’s associated co-morbidities (whether they have any other medical conditions that might be of influence)
- Whichever way a clavicle fracture is treated there are always risks and benefits. I will always assess each patient on an individual basis and, by taken the various factors into consideration, decide with them what is likely to be the best form of treatment for their fracture
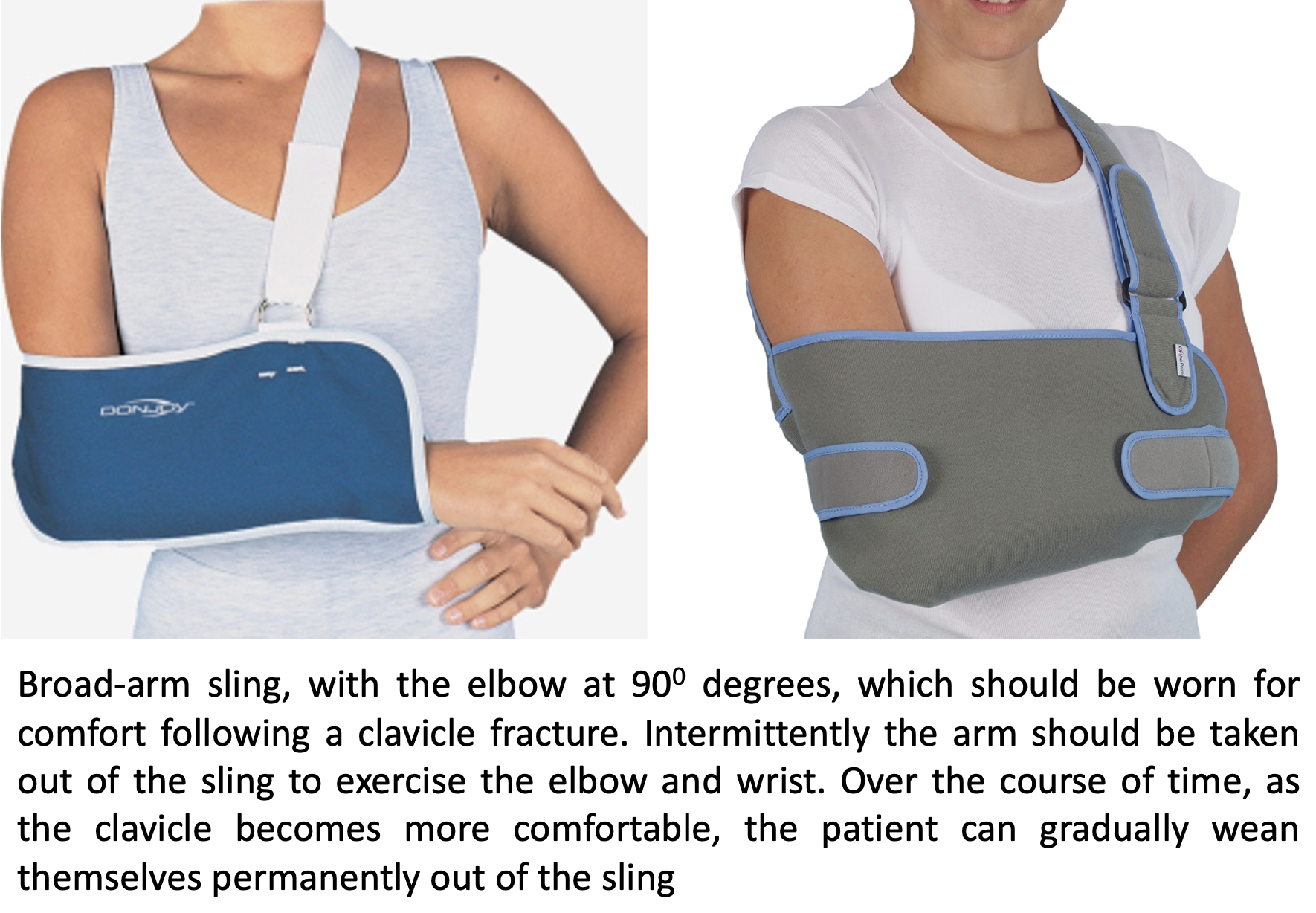
Non-Operative Treatment
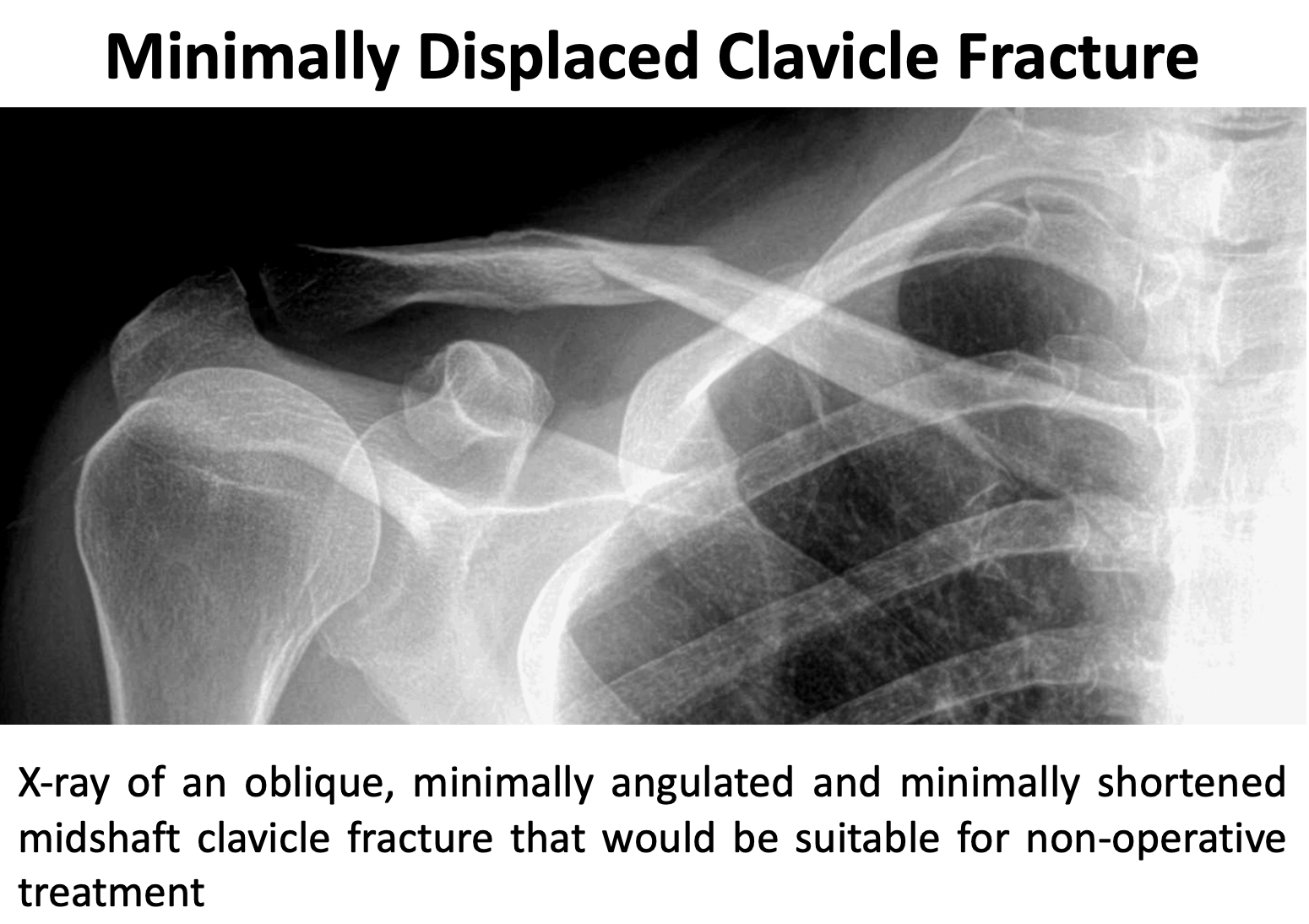
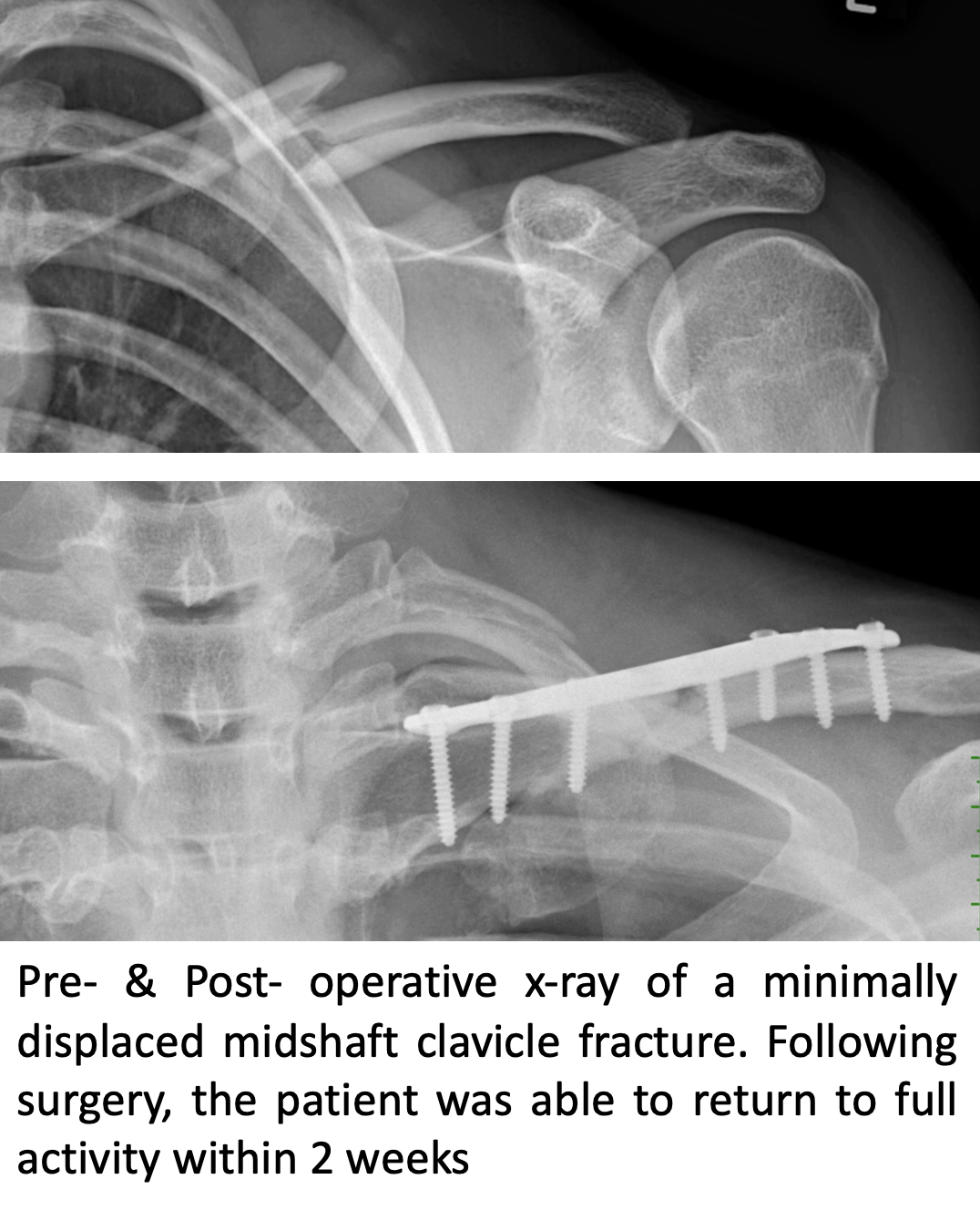
- Minimally displaced fractures or fractures that when healed are unlikely to lead to a significant functional deficit can be treated non-operatively
- Initial treatment is immobilisation in a sling and regular analgesia for comfort
- As the GH joint has not been damaged, most patients will be able to move their shoulder with reasonable comfort almost immediately below shoulder height
- Gentle movements of the shoulder, elbow and wrist are encouraged
- Generally, patients will be reviewed in the clinic at 2 weeks and a check x-ray taken
- The purpose of this x-ray is to check that the fracture position has been maintained
- It usually takes at least a month before any evidence of early healing callus can be seen on an x-ray
- After 2 weeks, patients are encouraged to begin to gently ‘wean’ themselves out of the sling as pain and comfort permits
- At 4 weeks most patients will no longer require a sling and will be getting back to daily functional activity
- It will usually take 3 months + before patients can return to full, unrestricted activities
- It will usually take 9 months + before the fracture appears to be completely united on x-ray
Rehabilitation Protocol
| Non-Op Clavicle Fracture | |
| Immediate |
|
| 2-4 Weeks |
|
| 4 Weeks + |
|
| Milestones | |
| Week 4 | 75% of full ROM, comfortable out of sling |
| Week 12 | Full ROM, 90% to full strength |
Return to Functional Activities
Desk based work 1 – 2 weeks
Driving 2 - 3 weeks
Swimming 6 weeks
Contact Sports 3 months +
Lifting Light - 6 weeks
Heavy - 3 months +
Work Sedentary - 2 - 3 weeks (limited light lifting duties)
Manual - 3 months +
Delayed Recovery
- Occasionally, for whatever reason, the healing of a routine clavicle fracture may be significantly delayed (Delayed-Union) or may not occur (Non-Union)
Find out more about the management of clavicle delayed-union, non-union and mal-union …..
Surgery for Clavicle Fractures
- A clavicle fracture is not an immediately life-threatening injury and there is generally a couple of weeks before a delay in ‘definitive’ treatment will have a potential detrimental effect on the final outcome
- Surgical fixation of a clavicle fracture,
- can restore the anatomy of the clavicle which will allow for an improved functional recovery
- for significantly displaced fractures, it will align the bones into a better position to improve the likelihood of healing
- it will immediately stabilise the fracture and allow for an expedited return to function
- it will align the bones anatomically to prevent a cosmetic asymmetry due to a malunion
- However, surgical fixation of the clavicle has all of the usual risks associated with any operation, cannot always guarantee that the fracture will unite and leaves an incision scar
- The 3 Main indications that I would consider surgical fixation of the clavicle are,
- Likely Non-/Delayed- Union (fractures that have a significant chance of not healing)
- Likely Functional Deficit (fractures where the displacement is likely to have a significant detrimental effect on function)
- To Expedite the Speed of Recovery (for patients who require a quicker return to function (associated other injuries, personal/sport/professional need)
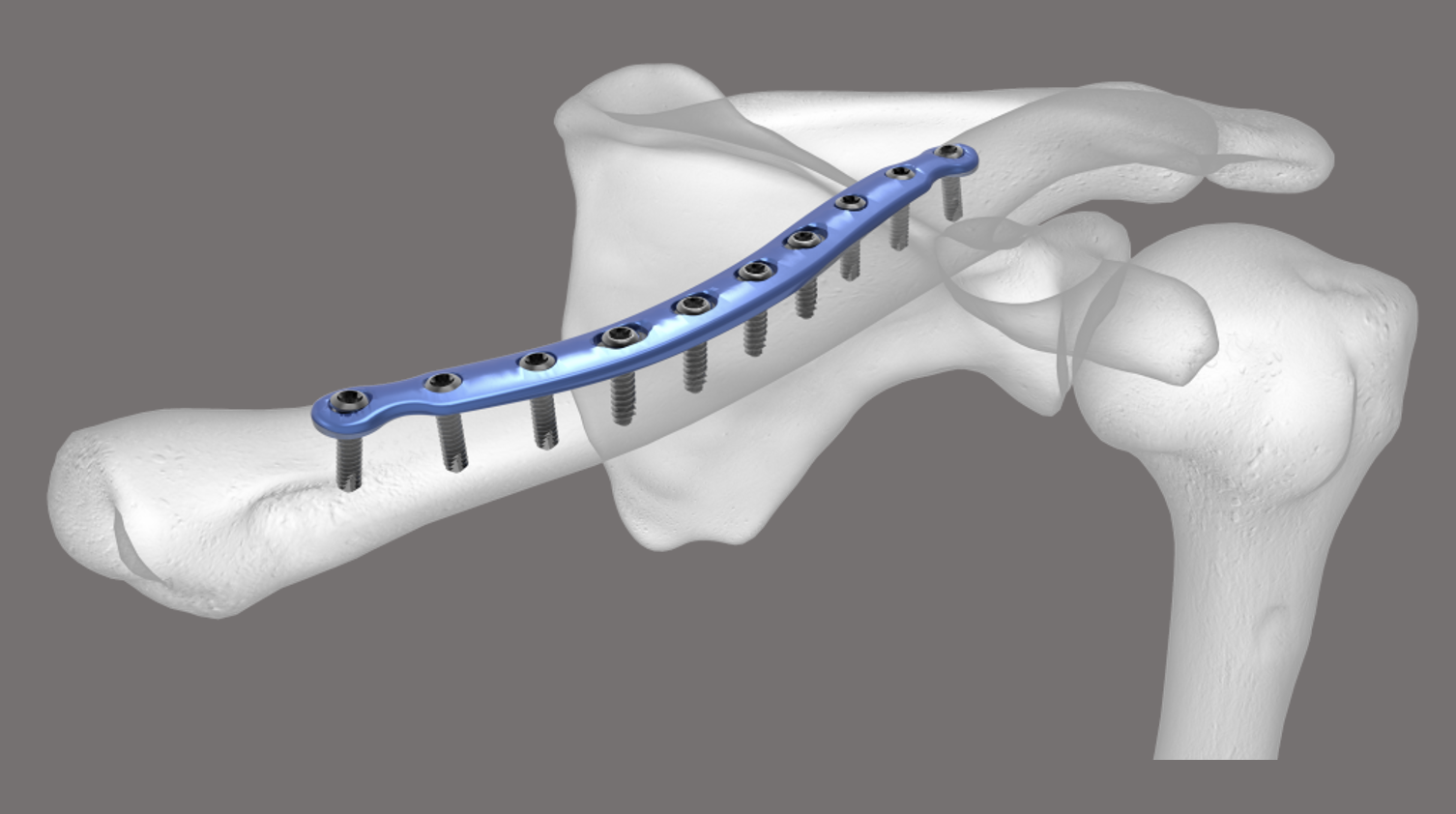
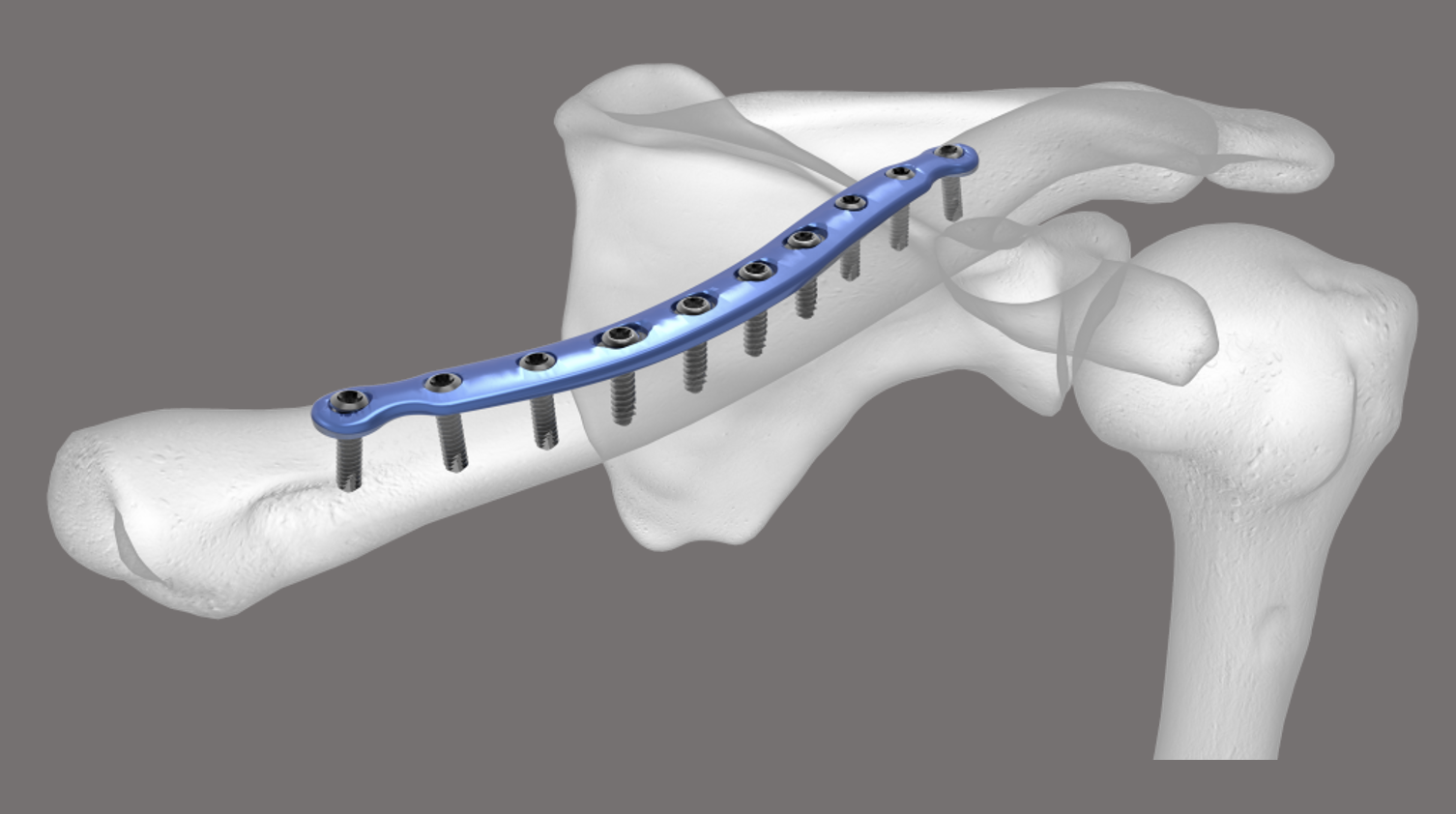
Open Reduction and Internal Fixation (ORIF) for Clavicle Fractures
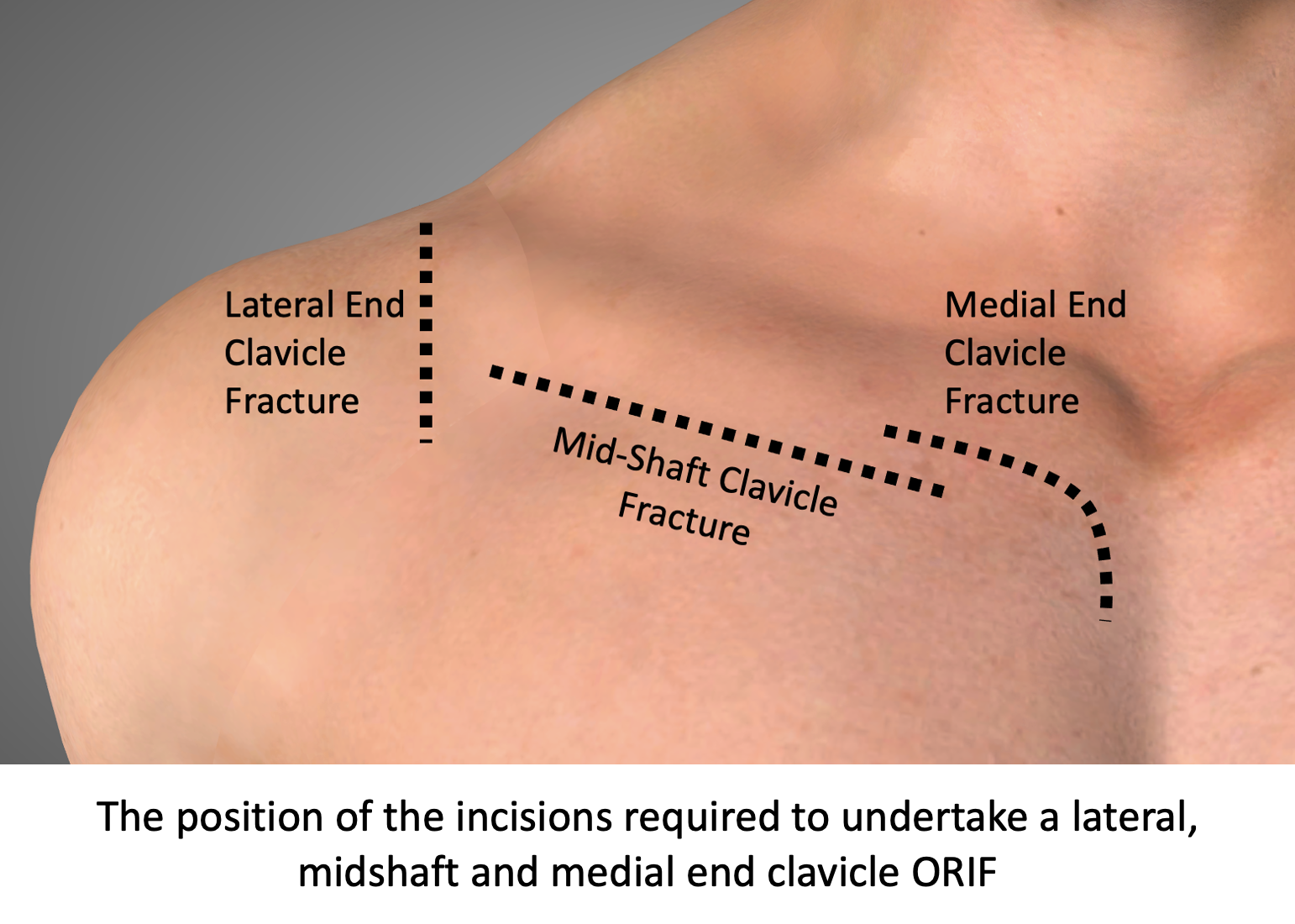
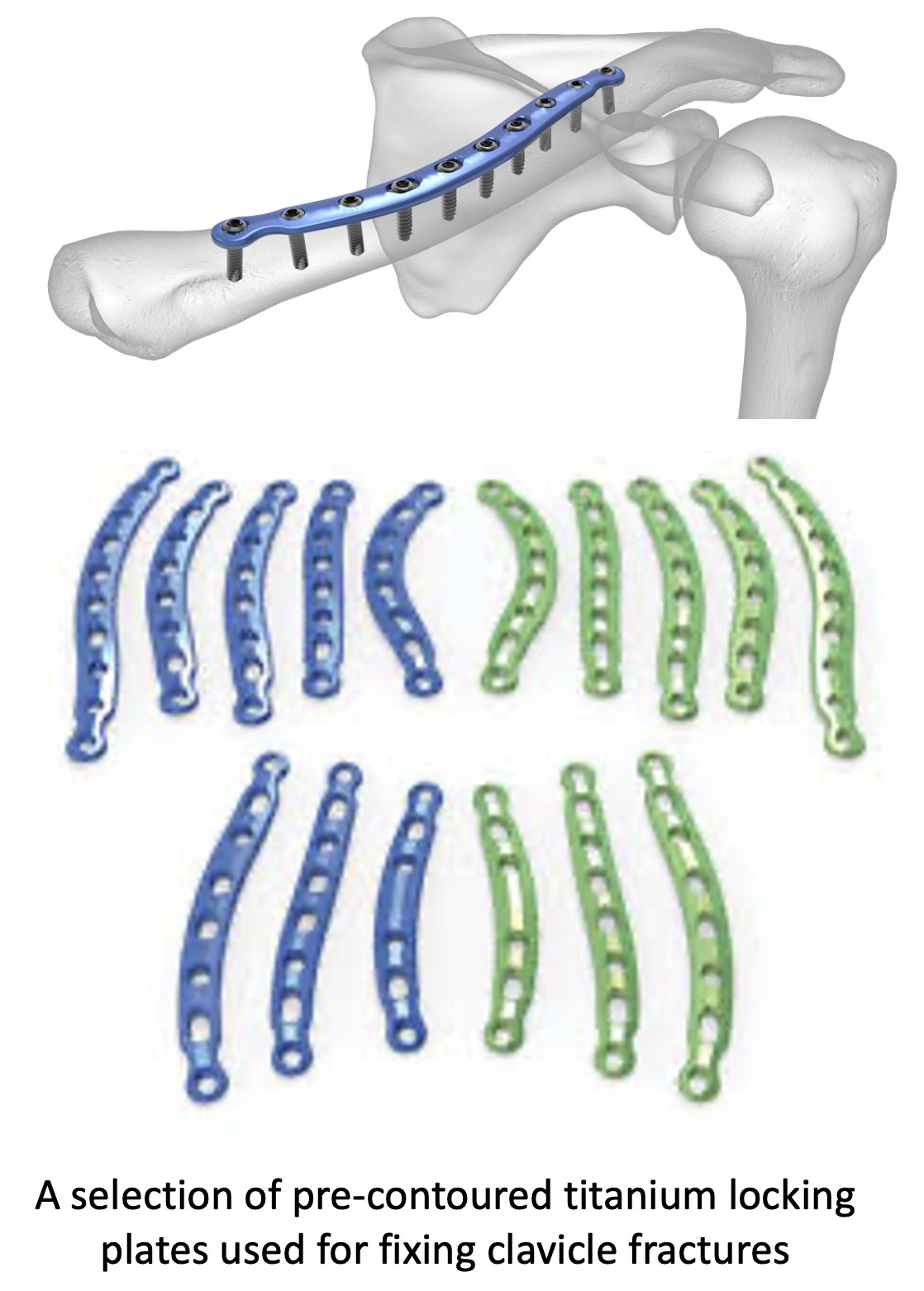
Operative fixation of a clavicle fracture requires an incision just below the clavicle at the site of the fracture. Due to the curved shape of the clavicle, I use specialised pre-contoured titanium plates with locking screws to fix the fracture.
My routine ORIF technique for a clavicle fracture is described below,
- The patient is anaesthetised with a general anaesthetic. For lateral-end clavicle fractures an interscalene nerve block is used
Find out more about having a general anaesthetic…. (Patient Information – Having an Anaesthetic – General Anaesthetic)
Find out more about having an interscalene nerve block…. (Patient Information – Having an Anaesthetic – Interscalene Nerve Block)
- A single intravenous dose of prophylactic broad-spectrum antibiotics is administered
- A longitudinal infraclavicular incision is made in the skin. The length of the incision will depend on the fracture type and the length of plate that is required to fix it
- The Platysma is divided, and the clavicle and fracture site exposed
- Depending on the nature of the fracture and whether it is an acute or delayed case part of the Deltoid & Trapezius muscles may need to be released
- The ends of the fracture and any comminuted fragments are then exposed and mobilised
- The fracture is then ‘reduced’ into its anatomical position
- Large comminuted fragments may sometimes be screwed together, seperately
- Once the fracture has been reduced an appropriately sized contoured plate is then chosen and ‘offered’ up
- Sometimes some additional contouring of the plate is required using plate benders
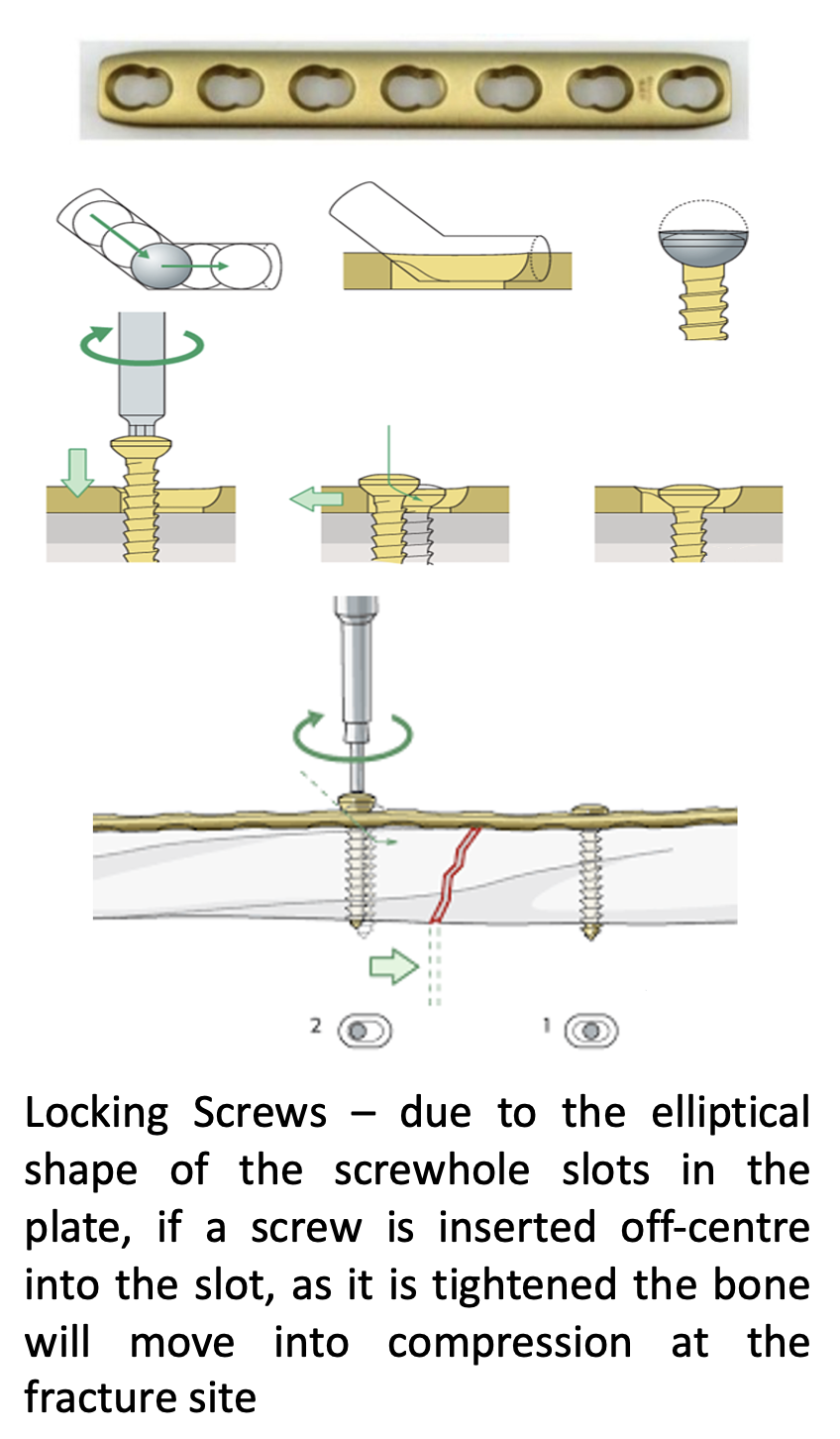
- The plate is then positioned onto the clavicle and screws inserted through the plate screwholes to secure it in place
- The screwholes in the plate are elliptical in shape which allows for some screws on oneside of the fracture to be positioned off centre so. When they are tightened, the underlying bone will slightly move putting the fracture site into compression
- At the end of the procedure an Image Intensifier is used to visualise the fracture site and plate to check the position
- Haemostasis is then obtained and the wounds closed in layers
- For patients that have not had an interscalene nerve block, local anaesthetic is then injected around the surgical site
After the Surgery
Post-Operative Care
Following an ORIF of a clavicle fracture the patient maybe able to go home on the same day as their surgery or may need to stay in the hospital over-night. This decision would depend on various associated factors.
I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder and how to use their Sling. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following Shoulder Surgery…. (Patient Information – Physiotherapy – Shoulder Physiotherapy)
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, the area around the clavicle should be numb from the local anaesthetic. This will usually last for 4-6 hours after the surgery.
The arm will be in a sling but, because the clavicle is now reduced and the fracture is structurally stable, patients will often be able to wean themselves out of the sling fairly rapidly.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Clavicle Fracture ORIF | |
| Immediate to 2 weeks |
|
| 2-4 Weeks |
· Full return to driving · Gradual return to most sports (avoiding contact)
|
| 6 + Weeks |
|
| Milestones | |
| Week 2 - 4 | Full ROM, comfortable out of sling |
| Week 4 - 6 | Full ROM, 90% to full strength |
Return to Functional Activities
Desk based work 1 weeks
Driving 1 – 2 weeks
Swimming 2 – 4 weeks
Contact Sports 2 months +
Lifting Light - 1 – 2 weeks
Heavy - 4 - 6 weeks +
Work Sedentary - 1 - 2 weeks (limited light lifting duties)
Manual - 4 - 6 weeks +
Success of Surgery, Risks & Complications
An ORIF of the clavicle is usually a very successful procedure with regards to alleviating pain and restoring good function. Whilst there is a rapid recovery of function, it can take 3 – 6 months before patients consider that they have completely recovered. However, in can take between 3 – 6 months or longer to achieve.
Removal of the Plate – a clavicle plate holds the bone in position. Once the bone has healed the plate is no longer required. As a general rule I would not routinely recommend removing the plate, it is completely inert and can be left in place indefinitely. Removing the plate requires a further anaesthetic and, because it can take 3 months for bone to grow into the empty screw holes that are left behind, there is a potential chance of refracture for 3 months after removal.
However, due to the subcutaneous position of the plate, sometimes patients can have issues with rubbing (particularly from bra straps and rucksacks). If this is the case then the plate can be removed but this can only be done at least 6 months after the initial surgery.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken
- Failure – About 20% of ACJ reconstructions stretch-out. However, this does NOT always lead to a recurrence of the symptoms
- Infection – Infection following open shoulder surgery is rare and occurs in about 1% of cases
- Non-Union – Although the surgery reduces the fracture, it still has to heal. Very occasionally the fracture will not heal. If this occurs there is a chance that the plate will break
- Neurovascular Injury – Damage to significant neurovascular structures during subcoracoid shoulder surgery is rare < 0.5%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system ….. (Patient Information – Outcome Measures)
Delayed-Union, Non-Union & Malunion of a Clavicle Fracture
Delayed-Union & Non-Union
- Occasionally, a clavicle fracture that is relatively undisplaced or a displaced fracture, where a decision has been made to treat non-operatively, will fail to unite
- By convention, a Delayed-Union is a fracture that has not healed at 6months and a Non-Union is a fracture that has not healed after 9 – 12 months
- Symptoms are usually continued pain and discomfort at the fracture site
- Diagnosis is made by,
- X-Ray – in an obvious non-union an x-ray will show that the bone ends have not healed. They are often rounded off and there is extra callus bone present that has not healed
- CT Scan – in some cases, due to the shape of the clavicle and that an x-ray only gives a 2-D view, it may be difficult to clearly see whether a fracture is healing or not. A CT scan will give a much more accurate assessment
- Treatment
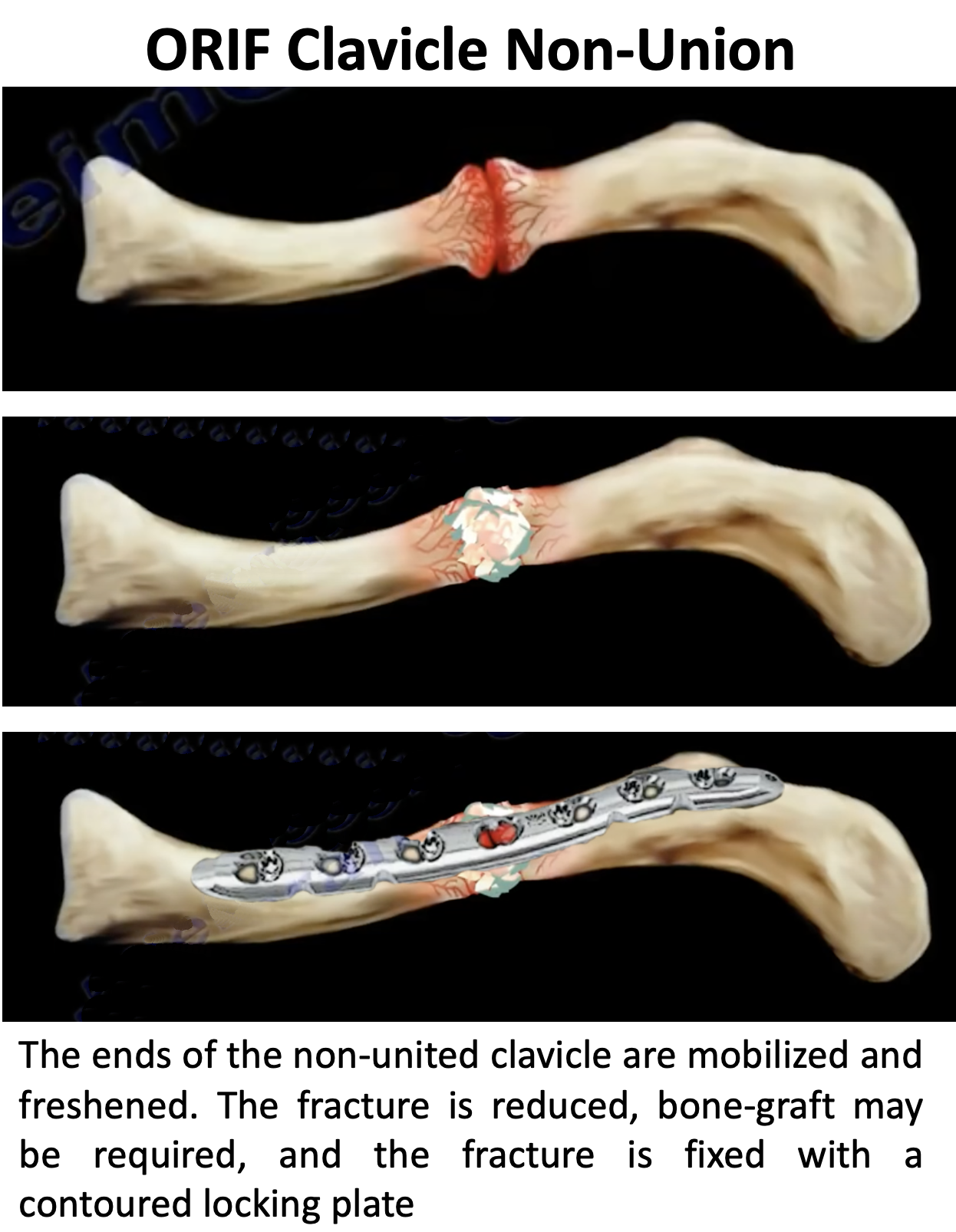
- The treatment for a symptomatic clavicle delayed- or non- union is surgery, an ORIF
- An ORIF for a non-union is exactly the same procedure as for an acute fracture. However, it often requires a more complex exposure of the fracture site and, in some situations, may require additional Bone Graft for the fracture to heal
Malunion
-
- A malunion occurs when a non-operatively treated clavicle fracture heals with the bones in a significantly abnormal position
- ‘Bump’
- The most common malunion is where there appears to be a significant ‘bump’ at the fracture site
- This represents some overlapping of the bones with additional callus formation. Over the course of a year this lump can decrease in size
- As a general rule the bone has healed solidly so patients rarely have any functional symptoms and most patients are happy to leave things as they are
- For patients that are concerned about the appearance or have issues with the ‘bump’ (bra-strap or rucksack) it is possible to do a ‘cheilectomy’ or taking the fracture down and undertaking an ‘ORIF’
- Cheilectomy – this is a procedure where an incision is made near the bump. The bump represents overlapping of the bones and it is possible to shave off some of the prominent bone without weakening the clavicle
- This procedure will generally decrease the size of the bump but will not completely correct it
- ORIF – this procedure requires taking the fracture down and then fixing it with a plate and screws. The bone does not usually require a bone graft or a lengthening osteotomy.
- Functional Malunion
- This is a very unusual situation where the clavicle fracture has healed with so much shortening and/or angulation that it has a significant effect on shoulder girdle function
- The best way to assess functional malunion is with a comparative CT scan where the malunited clavicle can be compared with the normal side
- If there is a significant functional malunion which the patient is unable to tolerate the only treatment option that is likely to improve the situation is a ‘surgical corrective osteotomy’
- Surgical Corrective Osteotomy – this involve undertaking a 3-D planned cut of the clavicle at the fracture site and re-positioning the bones in a more corrected position and then fixing them with a plate
- This is a far more complex procedure than a standard Clavicle ORIF with significant additional risks and complications with an increased chance of the fracture not healing
- ‘Bump’
- A malunion occurs when a non-operatively treated clavicle fracture heals with the bones in a significantly abnormal position
Click for more info (Fig 18)
Click for more info (Fig 19)
Click for more info (Fig 20)

Click for more info (Fig 21)

Click for more info (Fig 22)
Click for more info (Fig 23)

Click for more info (Fig 24)
Click for more info (Fig 25)
Click for more info (Fig 26)

Click for more info (Fig 27)
Click for more info (Fig 28)
Click for more info (Fig 29)
Click for more info (Fig 30)

Click for more info (Fig 31)

Click for more info (Fig 32)

Click for more info (Fig 33)
Click for more info (Fig 34)

Click for more info (Fig 35)
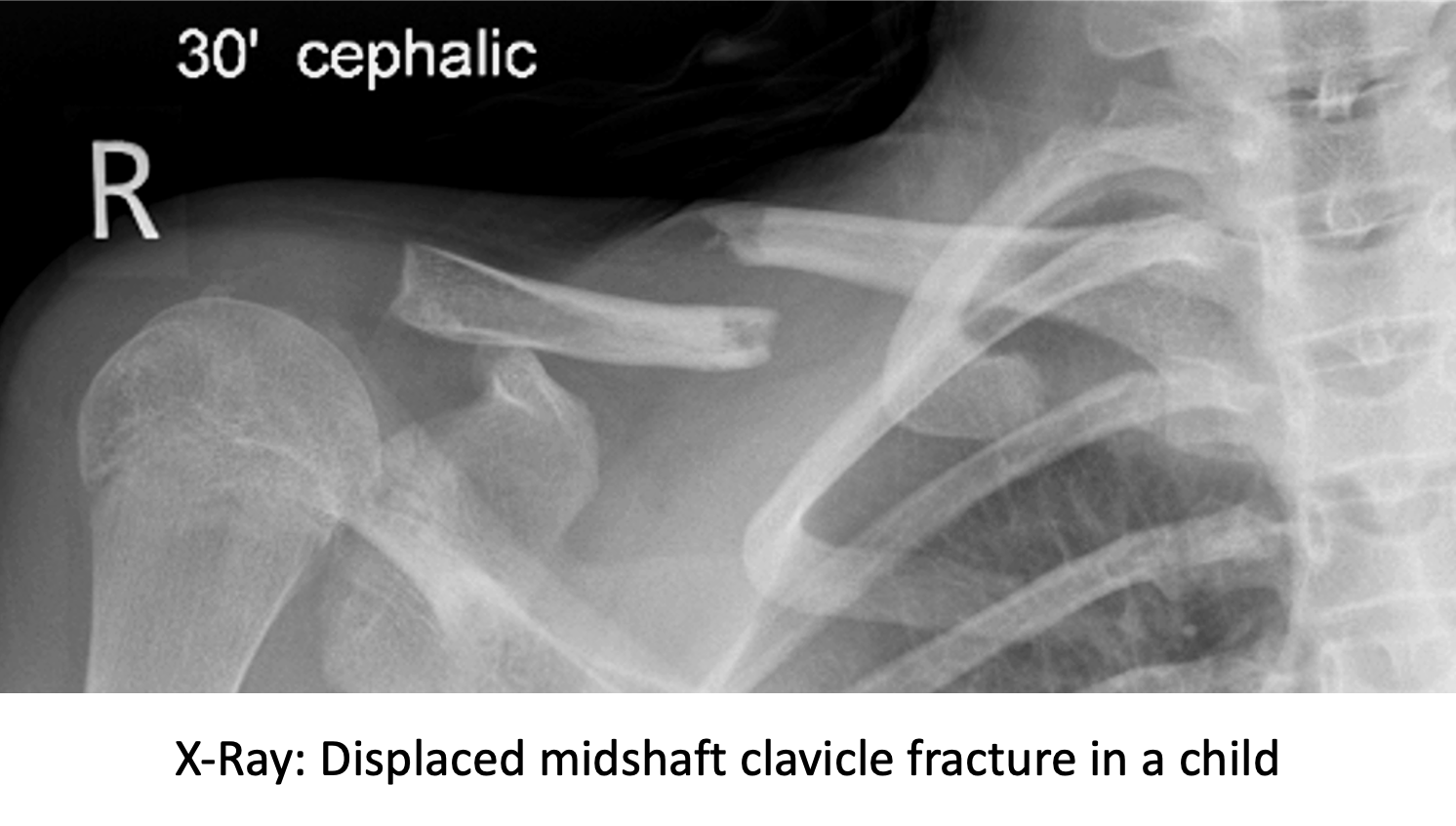
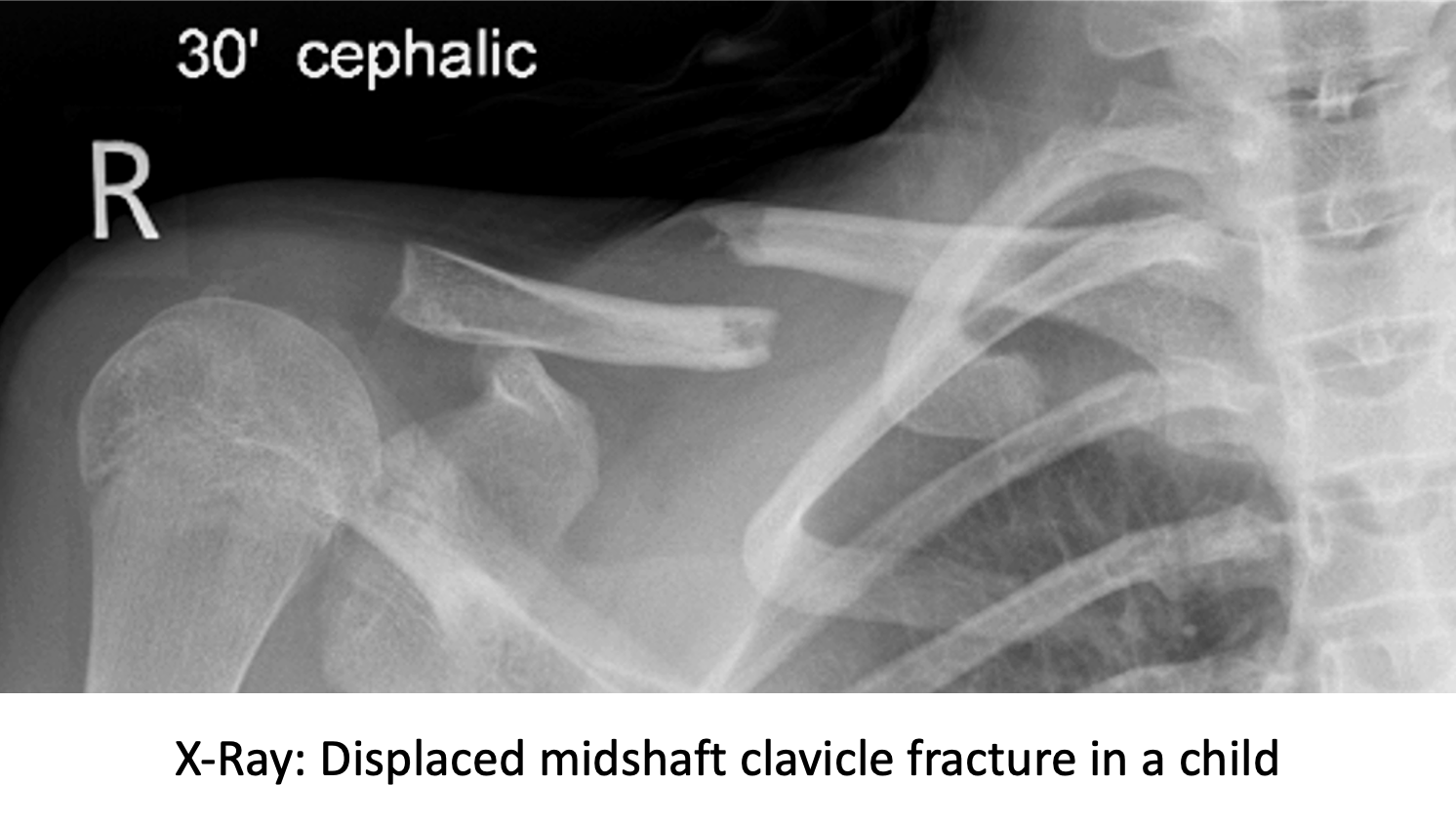
Children’s/Paediatric Clavicle Fractures
- Clavicle fractures in children can almost always be treated non-operatively
- Growing bones in children heal more quickly and can re-model in shape as they grow
- As a result, unlike adults, almost any amount of fracture displacement can usually be treated without surgery
- The bones will heal, and the residual deformity will improve over time with growth
- The younger the patient the quicker the fracture will heal and the greater the correction of the deformity
- On the very rare occasion that surgery is considered, a much less invasive operative procedure than is required for an adult can be undertaken
Mechanism of Injury (cause)
- Clavicle fractures can be caused by a,
- direct injury - onto the bone, such as a rugby tackle
- indirect injury - such as fall from a bike or a horse onto the shoulder and the force being transmitted down the clavicle which breaks
Diagnosis of Clavicle Fractures
- To diagnose & treat a clavicle fracture, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. When a clavicle fracture has occurred as part of a major accident the priority is to treat any life-threatening or more major injuries first. The best treatment for a particular patient with a clavicle fracture can depend on the severity of their symptoms and other associated shoulder conditions.
History
- In most cases of a clavicle there has been a significant injury where the patient has either landed or been hit on the point of their shoulder
- Following an acute injury, it is initially important to check for any other more significant associated injuries which includes neurological symptoms related to possible damage to the Brachial Plexus
- The main symptom is of pain with an associated prominence of the fracture and tenting of the skin
Examination
- The patient usually is usually supporting their arm with the shoulder in ADduction
- In acute cases there maybe associated grazing, or even a laceration, over the ends of the fracture
- Bruising, which can spread down the chest, tends to appear after a few days
- In acute cases, due to the severity of the pain, it maybe difficult to assess shoulder and scapula function
- Sometimes, due to displacement and shortening at the fracture site, the glenohumeral joint and scapula can be rotated forward into protraction. This can lead to problems with both glenohumeral and scapulothoracic function (Scapular Dyskinesia)
Investigations
- X-Ray – generally, all the information that is required to diagnose and treat a clavicle fracture can be obtained from an x-ray
- an additional AP view of the clavicle taken at a 300 angle upwards gives a better assessment of the fracture displacement
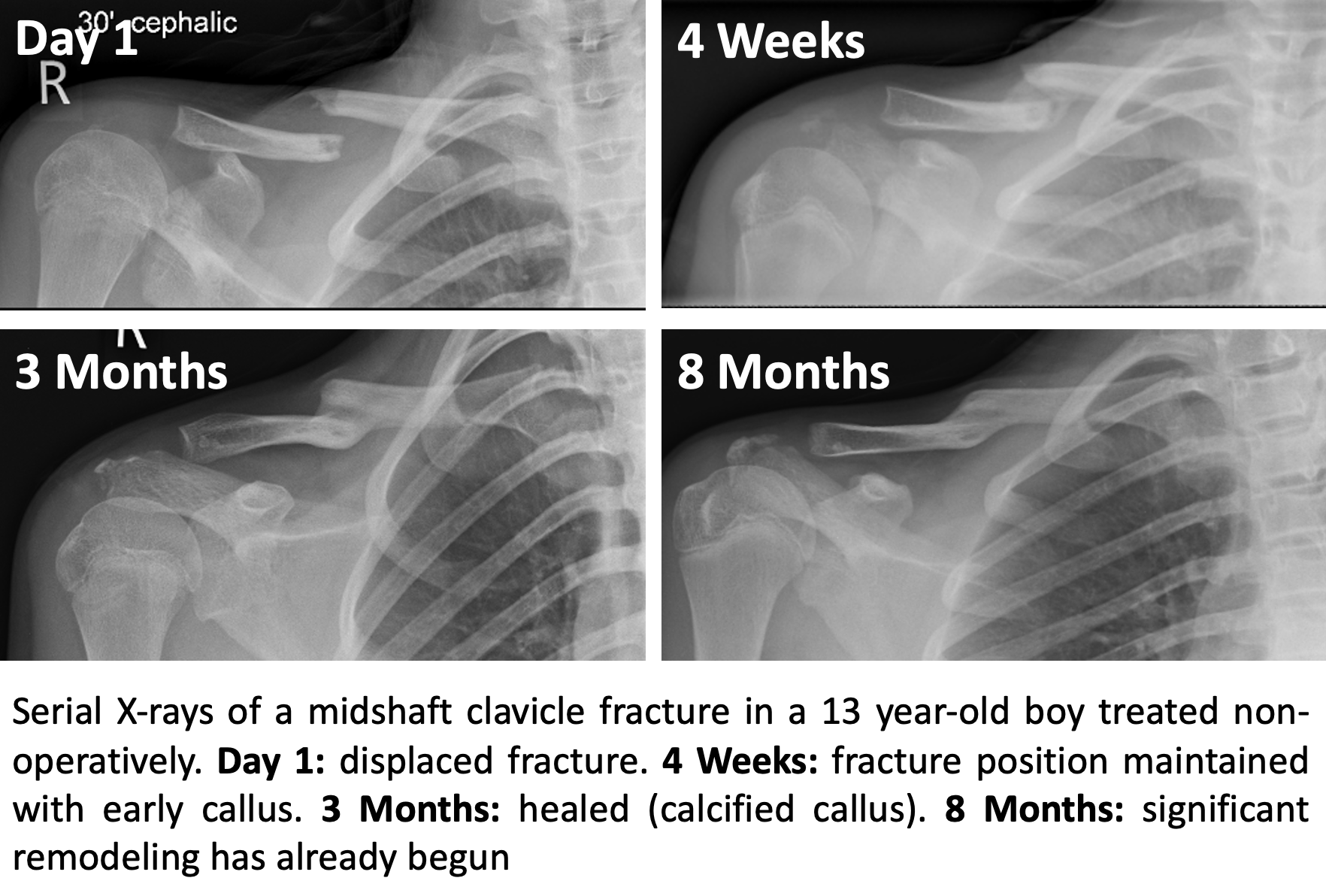
- serial x-rays can be used to assess the position of the healing of the fracture. However, it can take several months before any evidence of a healing callus can be seen
Treatment of Clavicle Fractures
- children’s clavicle fractures heal much more quickly than those of skeletally mature adults and
- due to growth and the increased speed and ability to heal, displaced clavicle fractures in children in children have the ability to remodel and correct
- the younger the child the quicker the speed of healing and the greater the ability to remodel
Non-Operative Treatment
- due to the ability to remodel almost every clavicle fracture in a child can be treated non-operatively, regardless of the amount of displacement
- Initial treatment is immobilisation in a sling and regular analgesia for comfort
- As the GH joint has not been damaged, most patients will be able to move their shoulder with reasonable comfort almost immediately below shoulder height
- Gentle movements of the shoulder, elbow and wrist are encouraged
- After 1 - 2 weeks, patients are encouraged to begin to gently ‘wean’ themselves out of the sling as pain and comfort permits
- The younger the patient the quicker the recovery
- In certain cases, physiotherapy can help with regaining a quicker functional recovery
- I recommend taking a clinic x-ray at 2 – 4 weeks to check that the fracture position has been maintained
- In many patients there will already be evidence of early healing (in the form of callus) present
- Many patients will be regaining good function after weeks
- By 2 – 3 months most patients will have made a full functional recovery
- Serial x-rays will demonstrate progressive calcification and healing of the callus
- However, it can take 6 months + before the fracture appears to be completely united on x-ray
Surgery for Clavicle Fractures
- As children get older the ability for fractures to remodel decreases
- Very occasionally surgical fixation for a clavicle fracture may be indicated
- This will usually be in the case of older children (14+ years) with significant displacement of the clavicle where the likely remodelling may not be sufficient to correct the deformity
- Operative Procedure - Depending on the ‘size’ and skeletal maturity of the patient there 2 potential operative options
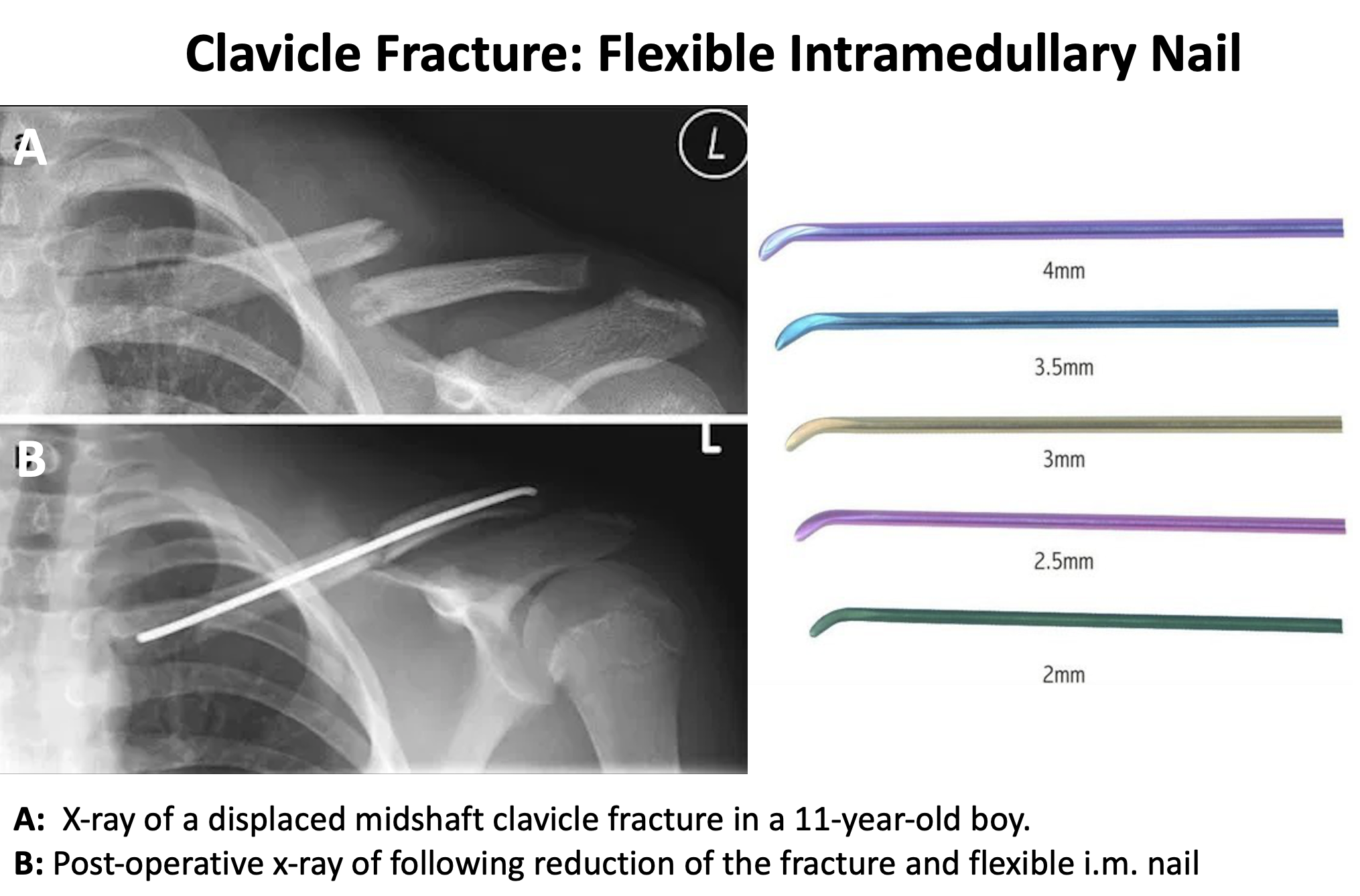
- Flexible Intramedullary Nail
- This is more appropriate for younger patients
- It only requires a small incision and does not need to hold the fracture in ‘perfect’ alignment, as the healing will remodel
- A flexible titanium nail is inserted into the medullary canal (the centre of the bone) of the lateral aspect of the fractured clavicle
- The bone ends are then reduced, and the nail is then passed across the fracture site into the medial part of the fractured clavicle
- The nail usually needs to be removed once the fracture has healed (6+ months)
- Open Reduction & Internal Fixation
- This is the same procedure, with a custom locking plate, that is used to fix adult clavicle fractures
- Flexible Intramedullary Nail
Find out more about Clavicle ORIF…. (Shoulder – Clavicle Fractures – Treatment of Clavicle Fractures)