The Long Head of Biceps
Anatomy & Function
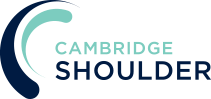
The biceps, or biceps brachii, is a muscle in the upper arm. It has 2 heads, the long head and the short head, that originate from the scapular and converge into a single muscle belly which then inserts into the radius bone in the forearm. Although the muscle spans two joints its main function is as a powerful flexor of the elbow and also a supinator (turning the hand inwards) of the forearm.
- Short Head of Biceps – this originates from the tip of the coracoid process and is blended with coracobrachialis muscle as the conjoint tendon. It converges with the Long Head to form the muscle belly and accounts for 85-90% of the strength of the muscle.
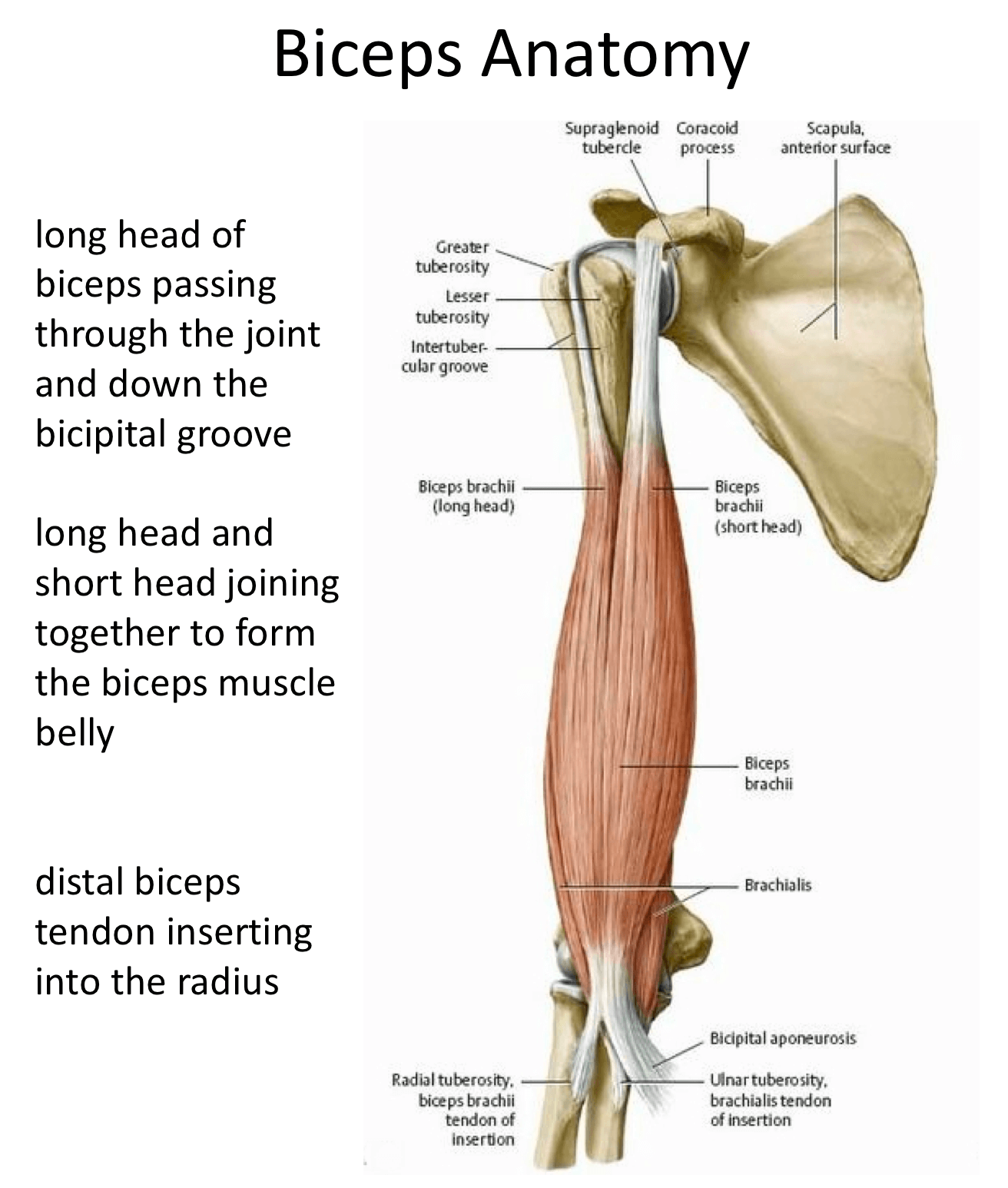
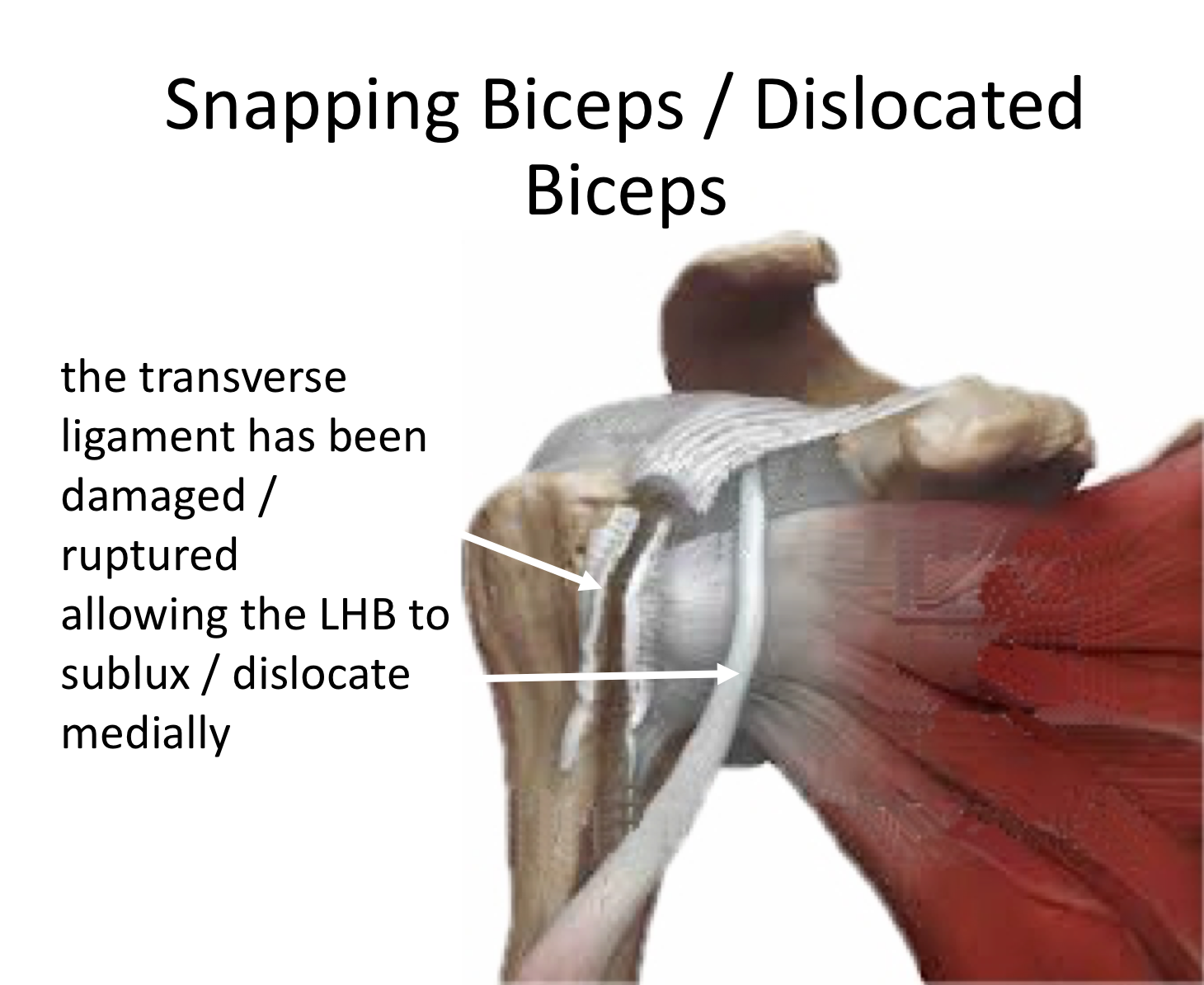
- Long Head of Biceps (LHB) – this originates from the supraglenoid notch at the top of the glenoid and its fibres blend with the superior labrum. The tendon passes through the shoulder joint and exits between the insertion of supraspinatus and subscapularis to run in a tunnel formed by the intertubercular groove (biciptal groove) in the humerus and the intertubercular ligament (transverse ligament). Two pulleys, the medial and lateral biceps pulleys, stabilise the LHB within the groove. The tendon then passes out of the groove and underneath the tendon of pectoralis major to converge with the Short Head, forming the muscle belly. The Long Head of Biceps is 10 – 15 cm in length and accounts for about 10% of the muscle strength.
What problems can occur with the Long Head of Biceps?
The mechanics of the LHB are not ideal! Unlike the Short Head which passes directly to the muscle belly the LHB passes through the shoulder joint, curves into the bicipital groove, passes down a tunnel and then underneath the pectoralis major tendon before inserting into the muscle belly. As a result, the LHB is vulnerable to damage and wear and tear as it passes through the joint to its eventual insertion.
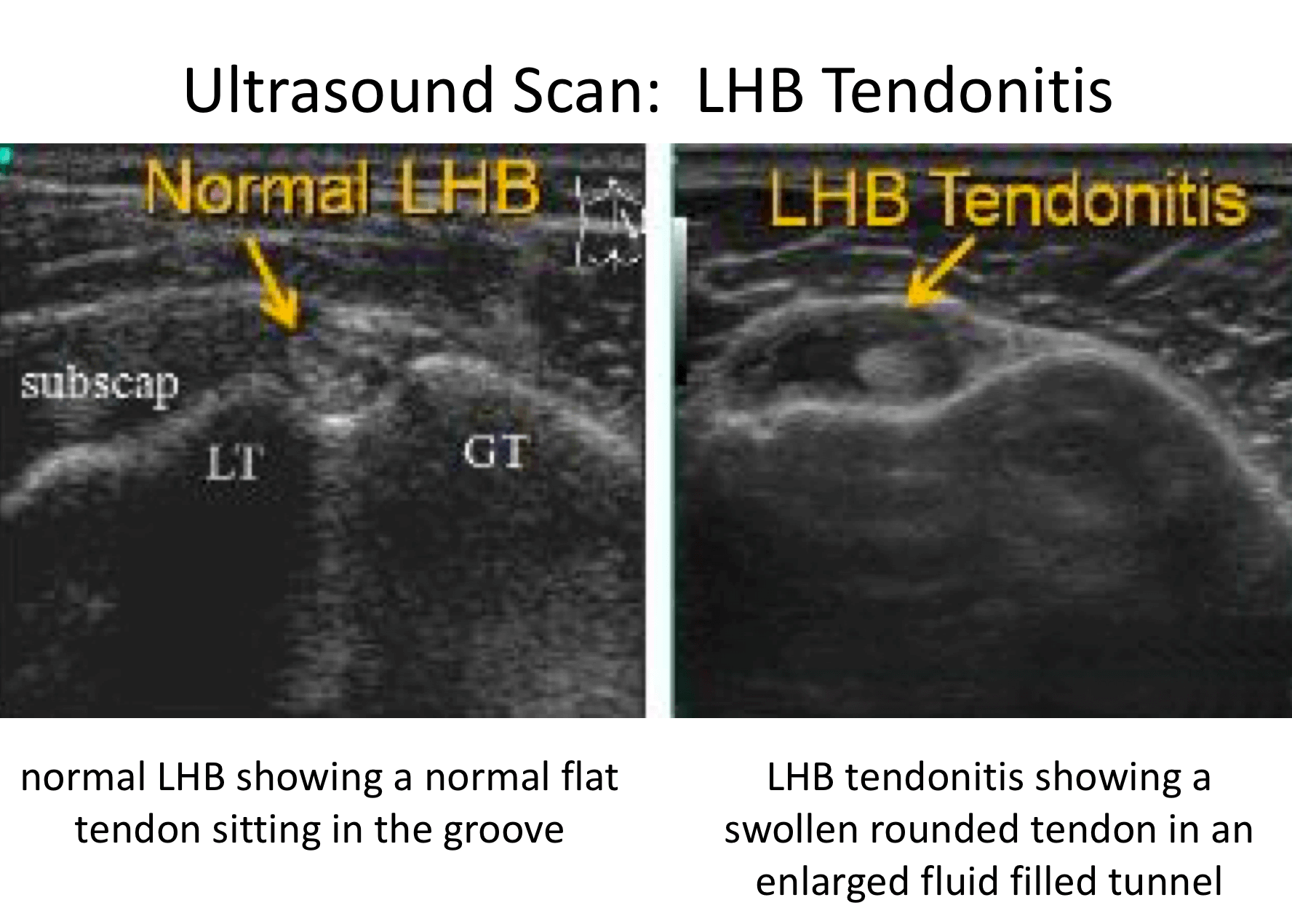
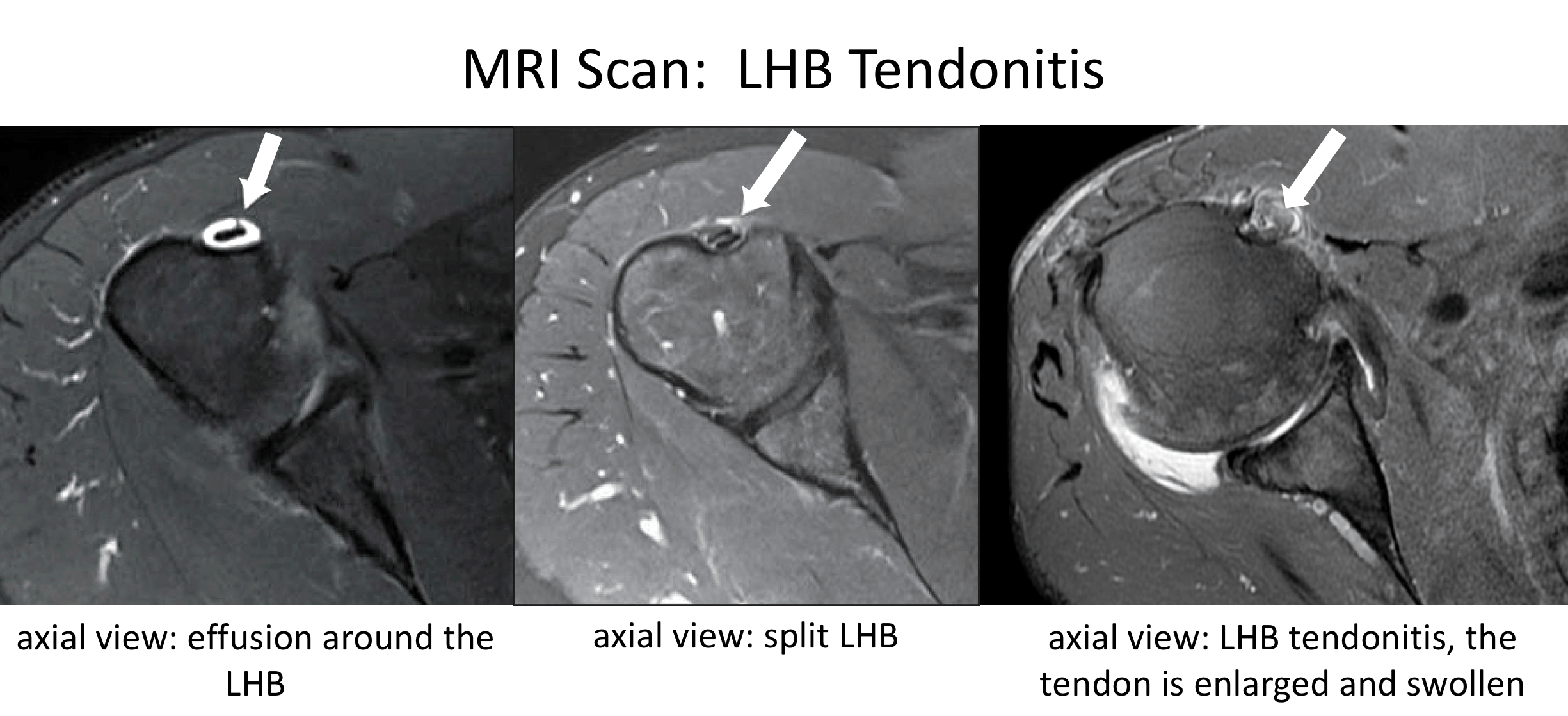
- LHB Tendonitis – like the rotator cuff tendons the LHB can undergo wear and tear damage within the joint and as it also passes through the bicipital groove.
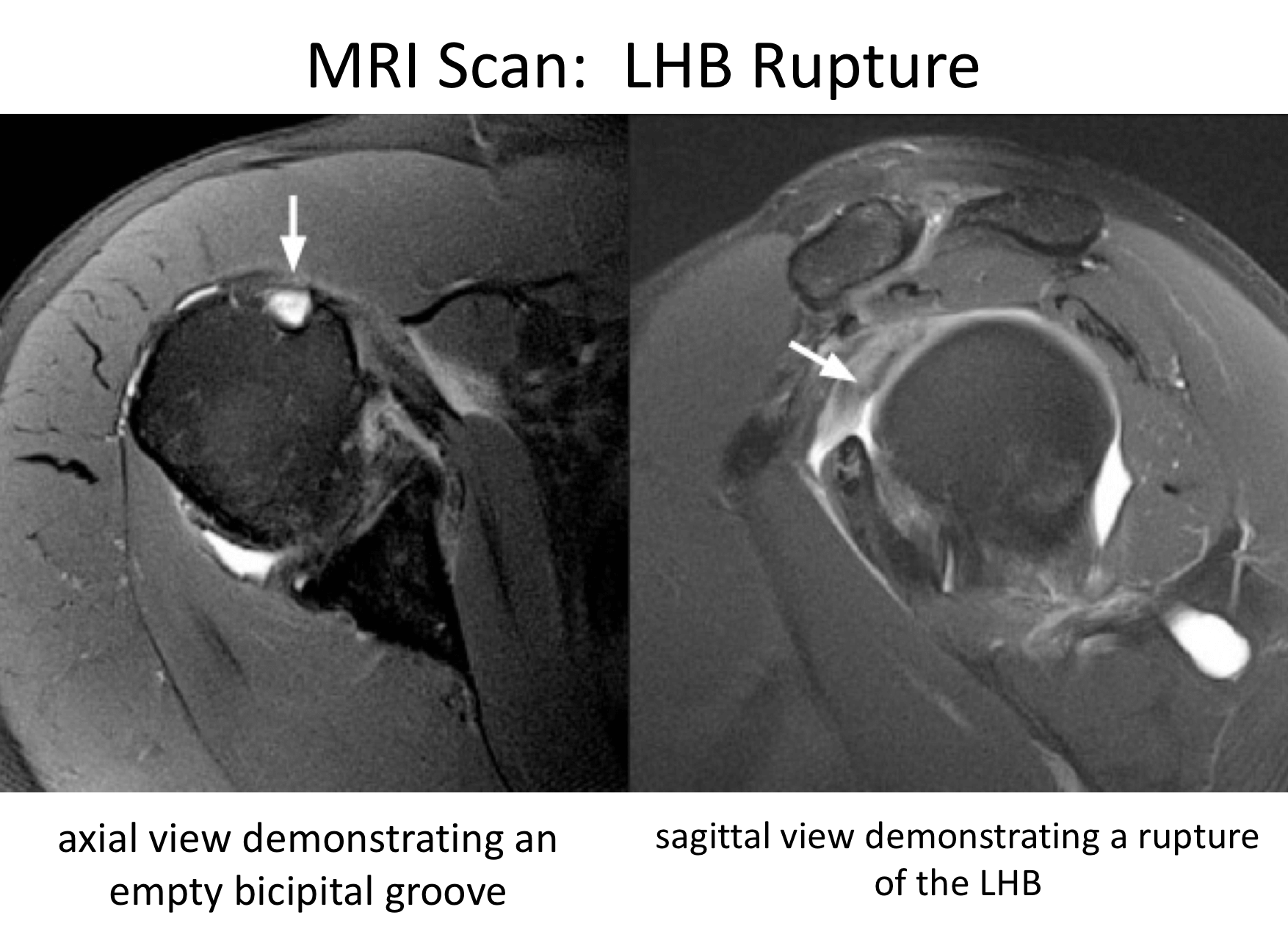
- LHB Rupture – over time, wear and tear changes within the LHB can lead to fraying, partial tearing and eventually rupture of the tendon.
- Snapping LHB – occasionally the medial biceps pulley and the top of the subscapularis tendon can tear allowing the LHB to sublux or dislocate out of the bicipital grove.
- Labral Tears – the origin of the LHB is intimately related to the glenoid labrum. Labral tears (SLAP tears – Superior to Anterior Labral Tears) often affect and can lead to LHB symptoms. Sometimes a labral tear can extend into the LHB
Symptoms & Diagnosis
What are the symptoms of a Long Head of Biceps problem?
- LHB Tendonitis -
- The most common LHB problem is a tendonitis. This is usually the result of wear and tear and, like rotator cuff tendonitis, tends to occur in patients over 40 years of age. The LHB is sometimes known as the ‘5th’ rotator cuff tendon and patients with LHB tendonitis often have associated rotator cuff problems.
- The main symptom of LHB tendonitis is pain over the front of the shoulder, often passing down into the main biceps muscle. This usually comes on gradually over time but can sometimes be the result of a sudden strain. The pain is often made worse when flexing the elbow, particularly against resistance, and sometimes when twisting the forearm, such as screwing something in (on the right) and unscrewing (on the left).
- Younger patients who do a lot of manual work, throwing sports, weight-lifting and body building can develop an isolated LHB tendonitis.
- LHB Rupture –
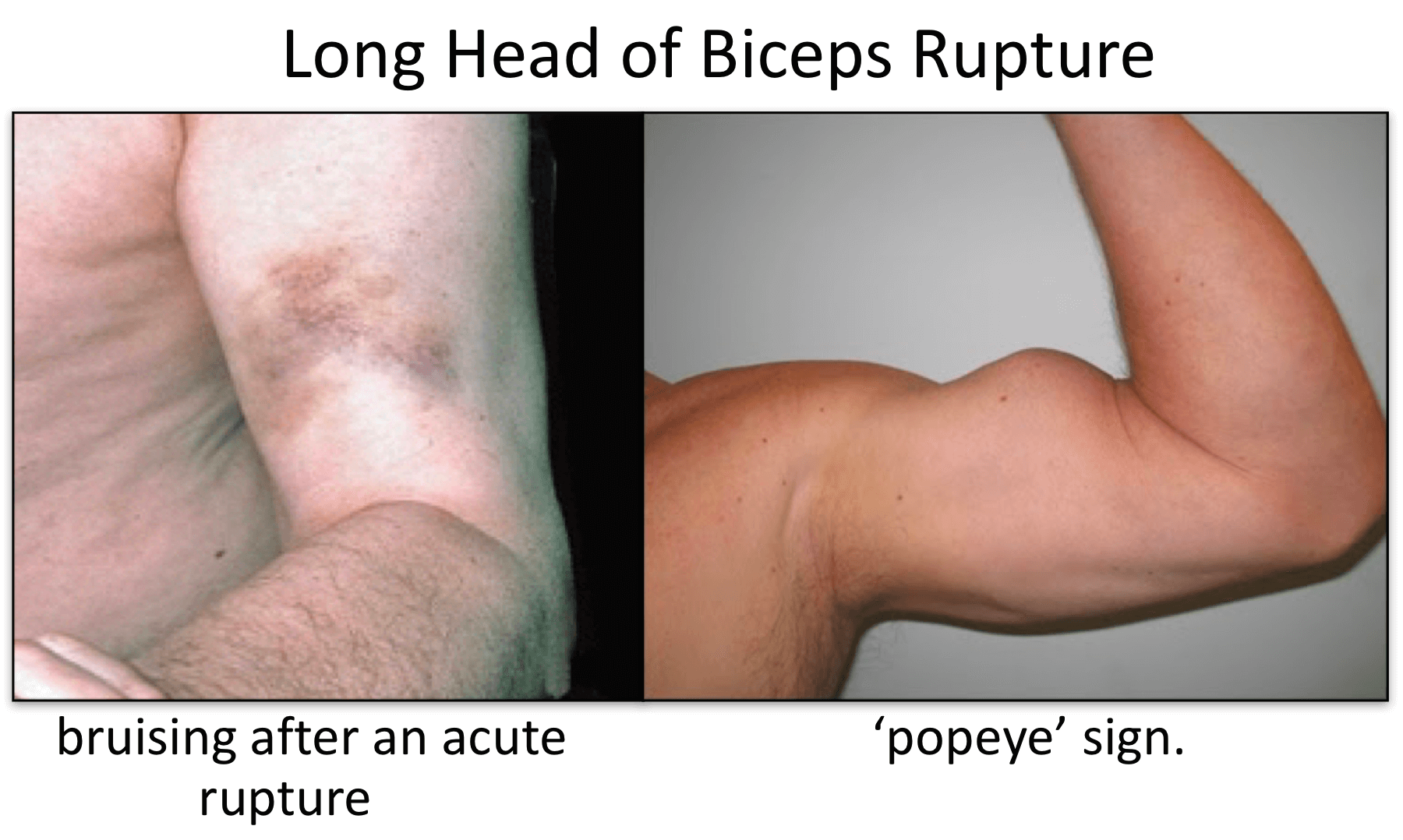
- With advanced wear and tear the LHB is prone to rupture. Often patients have had long standing LHB tendonitis symptoms and then experience a sudden ‘pop’ or ‘tearing’ sensation over the LHB, often associated with severe pain. This often occurs when they put a sudden strain on the biceps, such as lifting a heavy object, but can sometimes occur without a significant precipitating cause.
- An isolated LHB rupture can occur in people who do a lot of manual work, overhead sports, weight-lifting and body building.
- Following an acute rupture there is often significant pain and swelling with associated bruising that tracks down the arm. The top of the muscle tens to ‘ball up’ creating a ‘popeye’ appearance of the biceps. A ‘popeye’ appearance does not always occur as in some people the ruptured tendon gets stuck in the bicipital groove, keeping the tendon suspended, and in others, who have well covered arms, it is not obviously evident.
- o In most people who have an LHB rupture the bruising settles and, over the course of a couple of weeks, the pain subsides and eventually disappears. However, the ‘popeye’ appearance does not change.
- o Most people who have an LHB rupture have no significant symptoms or further problems following the acute injury. However, a small group of patients can experience an aching pain in their upper arm, over the site of the ruptured tendon stump, on activity. The Short Head of Biceps and the muscle are usually able to compensate over time for any strength loss for most people.
- Snapping LHB -
- Symptomatic subluxation, dislocation and snapping of the LHB is fairly unusual. It tends to occur in younger patients who undertake a lot of repetitive overhead or throwing activities. They tend to notice a ‘snapping’ or ‘clicking’ sensation over the front of the shoulder as the externally and internally rotate their shoulder, particularly when their arm is elevated.
- Labral / SLAP Tears -
- The LHB problems can be associated with damage and injuries to the Glenoid Labrum, particularly as patients get older. The symptoms associated with this are covered in the Labral / SLAP tear section.
How do you diagnose an LHB problem?
To diagnose & treat an LHB problem, like any other shoulder condition, requires a history, examination and investigation before deciding on an appropriate treatment. The best treatment for someone with an LHB problem can depend on a number of factors including their age, what activities the do and any associated rotator cuff problems.
History
- LHB tendonitis usually occurs gradually although occasionally they can start after a specific incident. People notice a pain over the front of their shoulder which can pass down into the biceps muscle. This is often brought on or made worse when bending the elbow up against resistance.
- LHB tendonitis is very often associated with rotator cuff problems. Patients also often have symptoms of a supraspinatus or subscapularis tendonitis.
- LHB ruptures usually occurs suddenly, often as a result of flexing the biceps with a sudden load. Patients usually describe a sudden ‘pop’ or ‘tear’ associated with pain and swelling over their upper arm. Over the course of the next few days some bruising may appear over the upper arm.
- The acute pain from an LHB rupture usually settles over a couple of weeks and some patients notice a ‘popeye’ appearance at the top of their biceps. Any pain that they were experiencing before the rupture usually disappears.
- LHB ruptures usually settle down over a few months and most patients become symptom free apart from a residual ‘popeye’ appearance.
- Occasionally patients experience a cramping like pain at the top of their arm over the stump of the ruptured tendon. This is often brought on after activity.
- Most patients do not notice any significant residual weakness following an LHB rupture. However, people who use their arms at the extremes of their strength, such as professional athletes, weight-lifters and body builders, may notice a residual weakness.
Examination
LHB Tendonitis
- Patients with LHB tendonitis often have associated rotator cuff problems and symptoms
find out more about Rotator Cuff problems ….
- Patients often experience pain on direct palpation over the LHB in the bicipital groove
- Resisted flexion or supination at the elbow usually increases the discomfort when pressing over the bicipital groove
LHB Rupture
- Patients with an LHB rupture often have an obvious ‘popeye’ sign which is accentuated by the patient flexing the elbow
- Patients usually do not have any symptoms of pain or weakness with an established LHB rupture
- Occasionally patients have some discomfort over the stump of the ruptured LHB on resisted flexion of the elbow
- Very occasionally patients have a noticeable weakness between the injured and non-injured side ‘Snapping’ LHB
- Most patients with a ‘snapping’ LHB do not have significant pain
- However, they have a palpable snap / flick that can be felt over the bicipital groove as the externally and internally rotate their shoulder in elevation
Investigations
- LHB problems are purely soft-tissue. As a result, a plain X-ray of the shoulder is usually unremarkable unless there are some associated shoulder problems
- USS – this is a very useful investigation to diagnose LHB problems. The bicipital groove, with the LHB running in it, is easily identified on an USS. Due to the dynamic nature of the scan the sonographer can see the LHB, as the patient moves their arm, running in the groove and can see any inflammation, fraying, damage or dislocation. It can also be used to locate the stump of a ruptured tendon.
- MRI – this a very useful investigation to look at the LHB and the other boney and soft-tissue structures around the shoulder. It can give additional information on the state of the glenoid labrum, biceps pulleys and the supraspinatus and subscapularis tendons.
Non-Operative
The vast majority of patients with LHB Tendonitis can be successfully treated non-operatively with a combination of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and Physiotherapy.
- Analgesia/Pain Relief - pain is the most severe problem associated with LHB tendonitis
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
- Nociceptive Analgesics –
- Nociceptive pain killers work on nerve generated pain
- Amitriptyline in lower doses works as a nociceptive pain killer. It has a useful side-effect in that it can make patients drowsy
- in cases of severe pain Amitriptyline can be prescribed at night
- NSAID (Non-Steroidal Anti-Inflammatories) –
- Physiotherapy –
- Physiotherapy and specific Biceps and Rotator Cuff Strengthening exercises are the main-stay of the initial treatment for LHB Tendonitis. By specifically strengthening the Rotator Cuff and Biceps muscles the LHB muscle can sometimes work and contract more efficiently settling the pain and discomfort. If pain is a particular feature a short course of NSAIDs prescribed by a Physician can help.
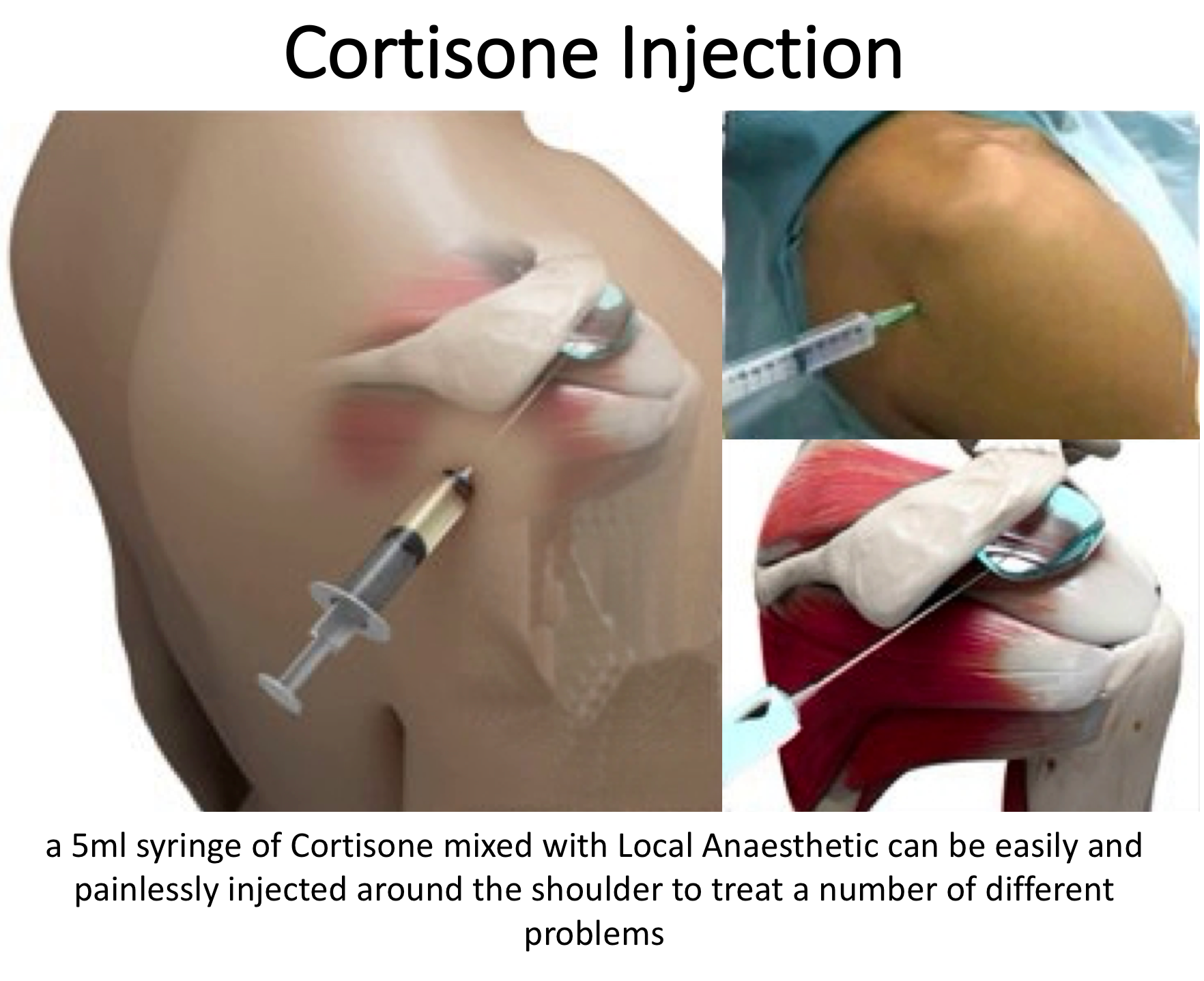
- Cortisone Injection -
- If someone’s LHB Tendonitis has failed to settle, after an adequate course of Physiotherapy, a Cortisone injection can help to settle the symptoms down. Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the Bicipital Groove it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- To gain the optimal benefit from a Cortisone injection it should be injected accurately into the Bicipital Groove. In patients with a lean body habitus this can be easily administered in the Out-Patient Clinic. However, an Ultrasound guided Cortisone injection may be more appropriate in certain circumstances. It is a quick and relatively painless procedure. Afterwards patients can continue with their normal day-to-day activities. Occasionally patients can feel a bit of soreness around their shoulder later that day, but this usually passes fairly quickly.
- It often takes several days before someone notices the benefits following a Cortisone injection and sometimes several weeks. The Cortisone works in the background and there is no specific requirement to particularly rest the shoulder or to do extra exercises. The full benefits of a Cortisone injection are usually felt within a month. In some cases, the Cortisone may not give any benefit, this may be an indication of the severity of the LHB Tendonitis.
- A Cortisone injection only lasts in the body for a few days. Any benefit that someone gets from the Cortisone will be from its acute anti-inflammatory effect allowing the LHB Tendonitis to settle. If the symptoms do return after a while, it is not because the Cortisone has worn off, but because the inflammation has returned
- Infections can occur after any type of injection but are extremely rare (1 in 15,000). If someone feels that they are developing an infection within 48 hours of a Cortisone injection they should seek advice from their Family Practitioner.
- Surgery for LHB Tendonitis –
- In some instances LHB Tendonitis fails to respond, or continues to recur, despite adequate Physiotherapy and Cortisone treatment. In this situation, the only treatment that is likely to settle the symptoms is Surgery.
Long Head of Biceps Surgery
Surgery for LHB Tendonitis
- There are several different surgical procedures that can successfully treat symptomatic LHB Tendonitis. Some are quicker with a shorter rehabilitation and others are more technically involved with a longer rehabilitation time.
- The choice of a particular procedure can depend on a patient’s age, body habitus, profession, sporting aspirations and concerns with regards to cosmetic appearance.
- All of the procedures can deliver a very satisfactory outcome for a particular patient if the patient’s expectations and needs are matched to the correct procedure
find out more about the surgical management of LHB problems ….
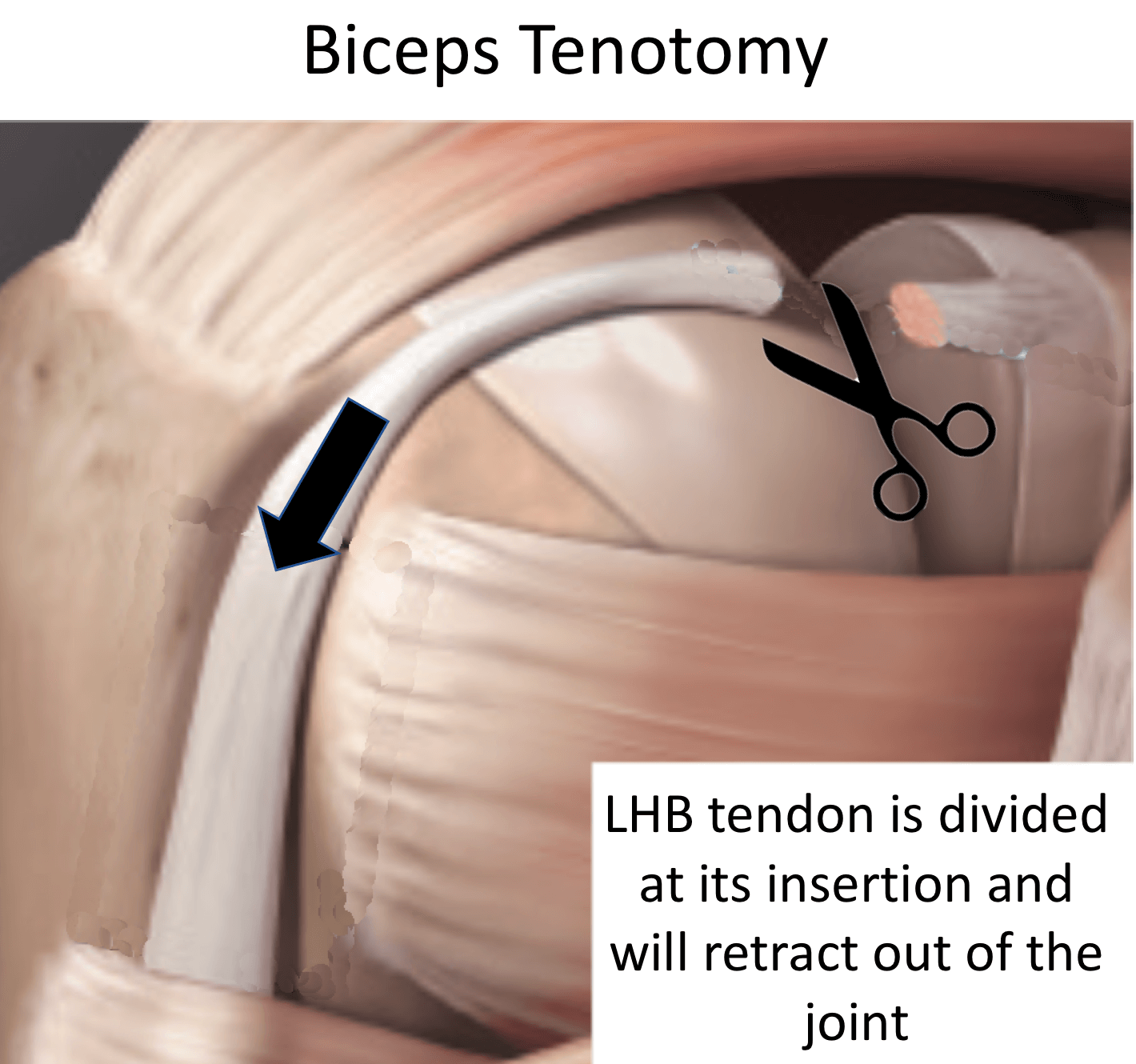
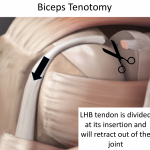
Tenotomy v Tenodesis v Transfer
- Tenotomy: An LHB Tenotomy simply involves detaching the LHB tendon within the shoulder joint at its origin at the top of the glenoid labrum. The LHB tendon then retracts out of the joint towards the muscle. Effectively this has the same effect as rupturing the tendon. Patients get an almost immediate relief of their pain with minimal functional deficit
- However, about 50% of patients end up with a painless ‘popeye’ appearance.
- An LHB Tenotomy is a quick and easy operation and is often incorporated with Rotator Cuff Surgery
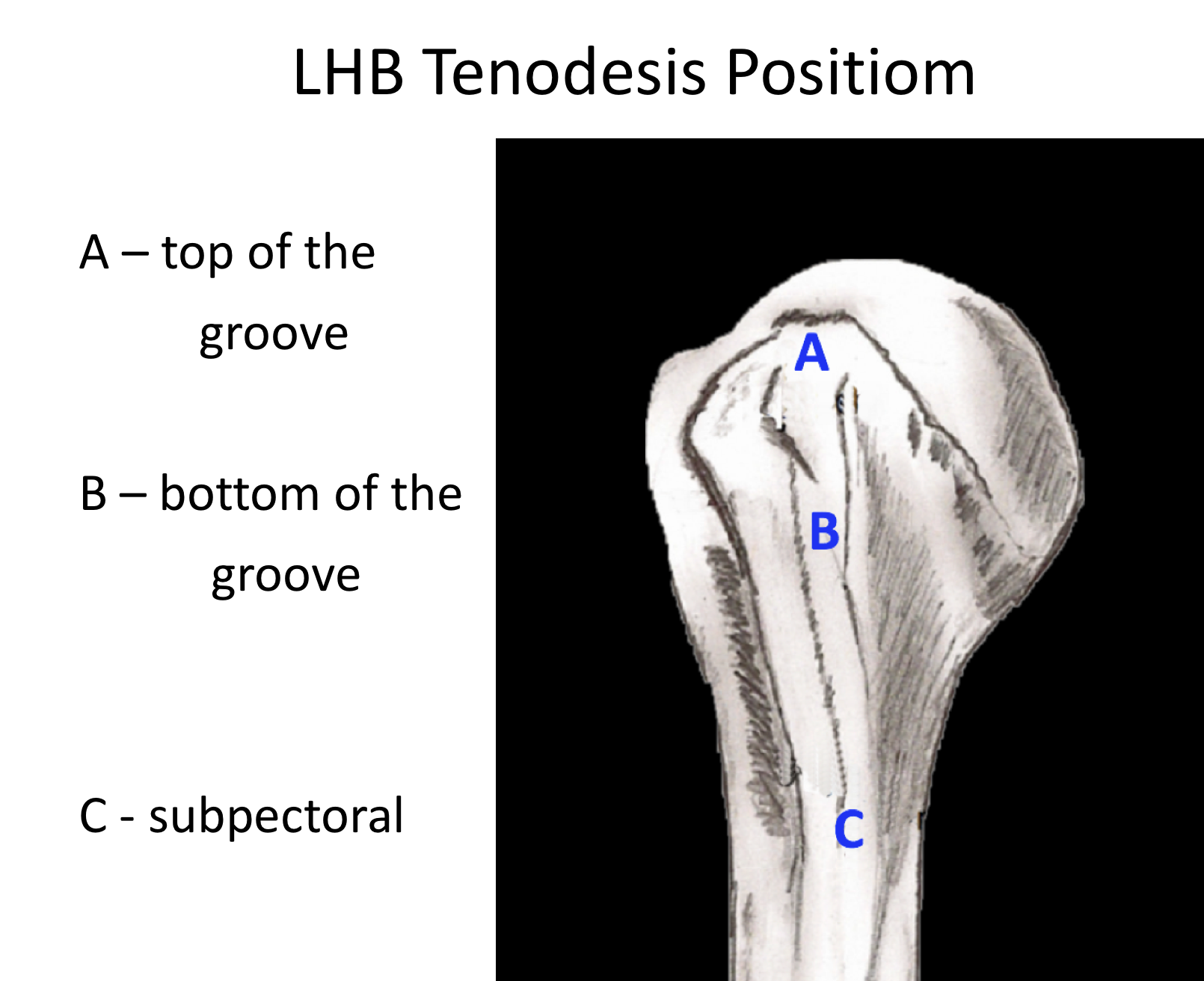
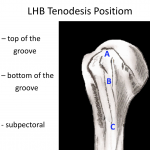
- Tenodesis: An LHB Tenodesis involves detaching the LHB tendon within the shoulder joint and then re-attaching it at some point along the humerus. With a Tenodesis the LHB continues to work as a biceps tendon
- There are a number of different positions and methods of fixation to Tenodese the LHB along the humerus. There are various technical and patient considerations with regards to the choice of which Tenodesis method is most appropriate for a particular patient
- Transfer: A LHB transfer involves detaching the LHB tendon from within the shoulder joint and then completely freeing the tendon out of the bicipital groove in the front of the shoulder right down to its musculotendinous junction
- Once the LHB has been completely mobilized it can be transferred medially to line up with the Short Head of Biceps which forms part of the Conjoint Tendon. The LHB is then sutured to the Conjoint Tendon. The LHB now pulls exactly in the correct biomechanical line of the biceps muscle belly
Arthroscopic Long Head of Biceps Tenotomy
One surgical option for someone with a symptomatic Long Head of Biceps (LHB) Tendonitis or a Snapping Biceps is an Arthroscopic Biceps Tenotomy. This is a relatively quick and easy procedure with a fast recovery. The operation involves an Arthroscopic camera being inserted into the shoulder joint and, under direct vision, the LHB is divided using specialized instruments. Often LHB Tendonitis can be associated with Rotator Cuff problems and a LHB Tenotomy is sometimes undertaken as an additional surgical procedure when operating on the Rotator Cuff.
An Arthroscopic LHB Tenotomy can usually be done as a Day Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to detach the LHB so that it is defunctioned and so alleviating pain. Recovery is usually fairly rapid and within 4 - 6 weeks most patients have gained the full benefits of the procedure. It has a high success rate with around 95% of patients being happy with the result 3 - 6 months after their operation. My routine Arthroscopic LHB Tenotomy Procedure is described below,
Watch a video of an arthroscopic biceps tenotomy….
Find out more about Arthroscopic Surgery….
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….Find out more about an Interscalene Nerve Block….
- A posterior and a single anterior portal are used to view the Gleno-Humeral Joint (Shoulder Joint)
- The Glenohumeral Joint is initially assessed to look for any other problems that might be associated with an LHB tenodonitis, in particular, with the Rotator Cuff
- The LHB is then probed and pulled up into the joint. Often the main area of damage and inflammation is located in the tendon just as it leaves the joint and passes into the Bicipital Groove
- Using an arthroscopioc punch, shaver or radiofrequency probe the LHB tendon is then divided at its base where it joins the glenoid labrum. The tendon then usually retracts out of the joint
- The top of the labrum is then debrided to a neat rim
- Again the Joint is examined to check for any hidden fraying or damage. It is then washed out and the wounds closed with sub-cuticular sutures
find out more about having an operation…
After the Surgery
Post-Operative Care
Following an Arthroscopic Biceps Tenotomy the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after an LHB Tenotomy….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves from using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 2 - 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic Biceps Tenotomy is usually a very successful procedure and most people notice a significant improvement in their pain within 4 weeks. About 50% of the time patients do notice a slight change in the contour of the biceps muscle, but this is usually relatively minor. There is usually no perceptible loss of muscle strength. Very occasionally people can experience an ache or cramping sensation at the top of the muscle, corresponding to the stump of the LHB tendon. This usually settles with time and can be aided by an ultrasound guide cortisone injection.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
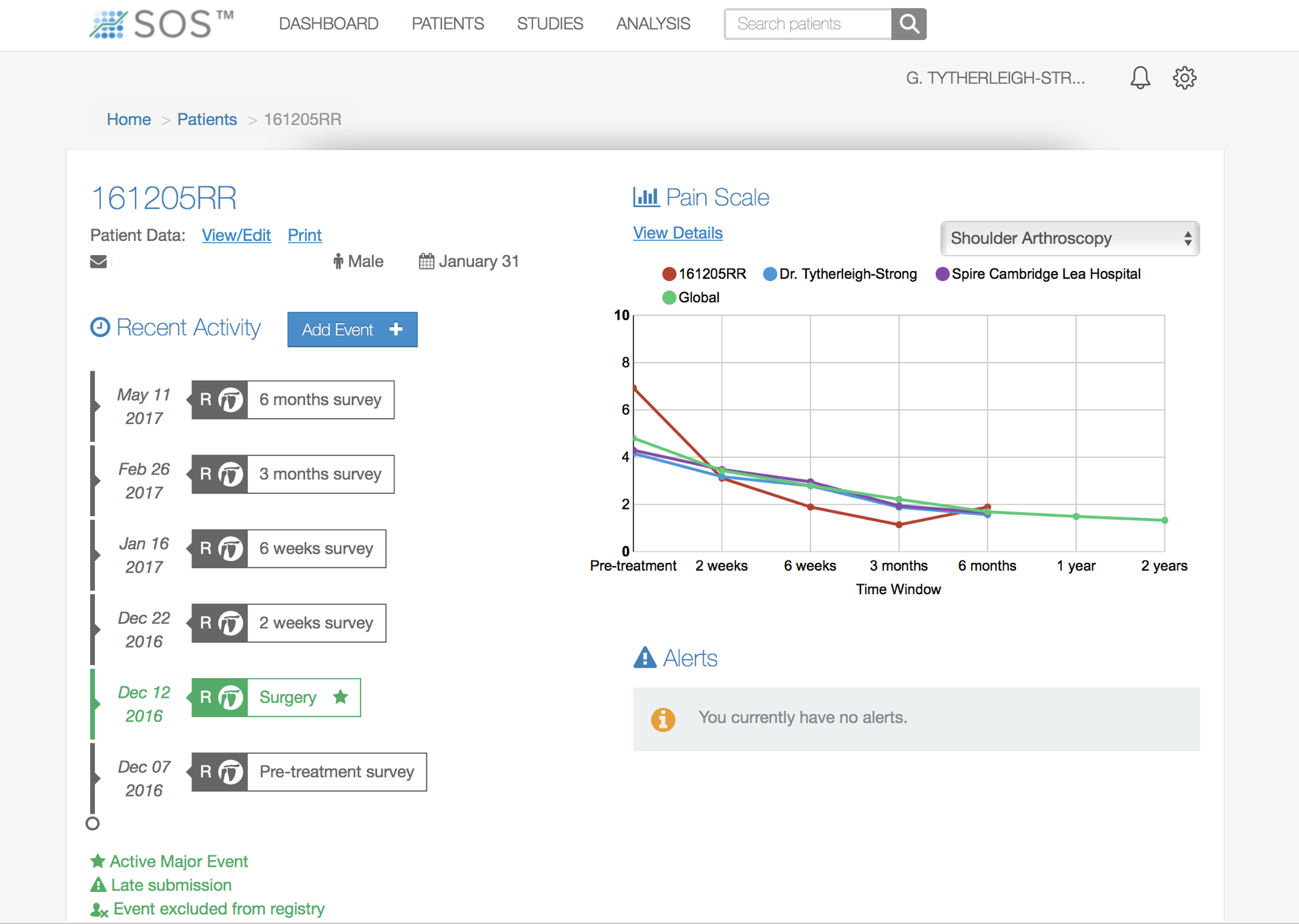
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Arthroscopic Long Head of Biceps Tenodesis
One surgical option for someone with a symptomatic Long Head of Biceps (LHB) Tendonitis or a Snapping Biceps is an Arthroscopic Biceps Tenodesis.
The ‘potential’ advantage of a tenodesis over a tenotomy is that the LHB tendon is ‘re-attached’ to the humerus, along the course of the bicipital groove. This may improve cosmesis, avoiding a post-operative pop-eye sign. For certain high demand individuals, particularly overhead athletes, the functional outcome maybe improved by a tenodesis.
The operation involves an Arthroscopic camera being inserted into the shoulder joint and, under direct vision, the LHB is divided using specialized instruments. The tendon is then re-attached to a ‘prepared’ area along the humerus. Often LHB Tendonitis can be associated with Rotator Cuff problems and a LHB Tenodesis is sometimes undertaken as an additional surgical procedure when operating on the Rotator Cuff.
An Arthroscopic LHB Tenodesis can usually be done as a Day Case procedure and the patient’s shoulder usually needs to be immobilized for 2 weeks afterwards. Recovery is usually fairly rapid and within 4 - 6 weeks most patients have gained the full benefits of the procedure. Although it can take up to 3 months to regain full functional strength. It has a high success rate with around 95% of patients being happy with the result 3 - 6 months after their operation. My routine Arthroscopic LHB Tenodesis Procedures are described below,
Watch a video of an arthroscopic biceps tenotomy….
Find out more about Arthroscopic Surgery….
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….Find out more about an Interscalene Nerve Block….
- A posterior and a single anterior portal are used to view the Gleno-Humeral Joint (Shoulder Joint)
- The Glenohumeral Joint is initially assessed to look for any other problems that might be associated with an LHB tenodonitis, in particular, with the Rotator Cuff
- The LHB is then probed and pulled up into the joint. Often the main area of damage and inflammation is located in the tendon just as it leaves the joint and passes into the Bicipital Groove
- Using an arthroscopioc punch, shaver or radiofrequency probe the LHB tendon is then divided at its base where it joins the glenoid labrum. The tendon then usually retracts out of the joint
- The top of the labrum is then debrided to a neat rim
- Again the Joint is examined to check for any hidden fraying or damage. It is then washed out and the wounds closed with sub-cuticular sutures
find out more about having an operation…
- The Glenohumeral Joint is initially assessed to look for any other problems that might be associated with an LHB tenodonitis, in particular, with the Rotator Cuff
- The LHB is then probed and pulled up into the joint. Often the main area of damage and inflammation is located in the tendon just as it leaves the joint and passes into the Bicipital Groove
- Using an arthroscopioc punch, shaver or radiofrequency probe the LHB tendon is then divided at its base where it joins the glenoid labrum. The tendon then usually retracts out of the joint
- The top of the labrum is then debrided to a neat rim
- Again the Joint is examined to check for any hidden fraying or damage. It is then washed out and the wounds closed with sub-cuticular sutures
find out more about having an operation…
- Using an arthroscopioc punch, shaver or radiofrequency probe the LHB tendon is then divided at its base where it joins the glenoid labrum. The tendon then usually retracts out of the joint
- The top of the labrum is then debrided to a neat rim
- Again the Joint is examined to check for any hidden fraying or damage. It is then washed out and the wounds closed with sub-cuticular sutures
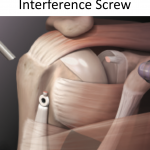
- For a groove tenodesis the anterior compartment of the shoulder is entered arthroscopically
- The top of the transverse ligament is divided to reveal the LHB
- The base of the groove is de-corticated and a 7mm ‘socket’ is drilled into the base
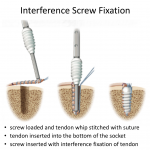
- The LHB tendon is then placed into the bottom of the socket and secured with a Tenodesis Interference Screw
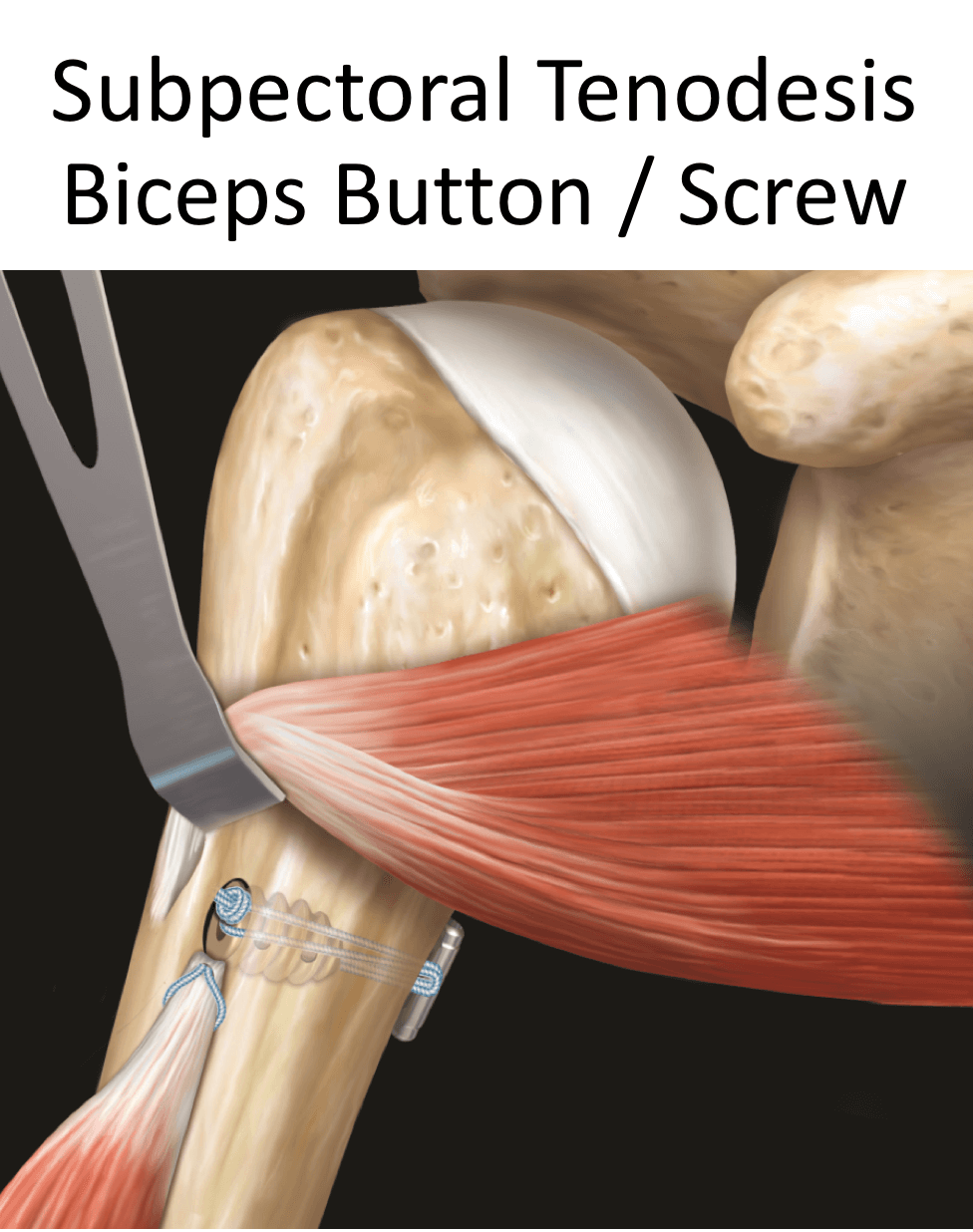
- For a sub-pectoral Tenodesis a 3cm incision is made at the front of the axilla, in the skin crease
- Dissection is taken down on the humerus to locate the LHB as it passes out from below the Pectoralis Major tendon
- The LHB is exteriorised
- A whip-stitch is then sutured from the musculotendinous junction of the biceps about 1.5cm up the tendon. The rest of the redundant tendon is then cut and discarded
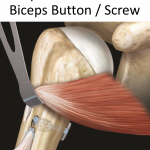
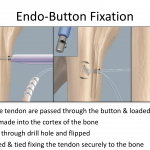
- The suture ends are then passed through the Biceps-Button which is mounted onto an introducer
- The shaft of the humerus is then exposed and a 4mm hole drilled through the cortex just below the pectoralis major
- The loaded Biceps-Button is then inserted through the drill hole in the humeral shaft. The button is then ‘flipped’ within the medullary canal of the bone and the sutures tightened through the button. This brings the end of the tendon onto the bone and the construct is tightened to an appropriate tension
After the Surgery
Post-Operative Care
Following an Arthroscopic Biceps Tenotomy the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy after an LHB Tenotomy….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves from using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 2 - 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic Biceps Tenodesis is usually a very successful procedure and most people notice a significant improvement in their pain within 4 weeks. The Biceps muscle contour will be maintained and it would be expected, after appropriate rehabilitation, that a near full function should be regained.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Treatment for LHB Rupture
- LHB ruptures usually occur suddenly but are usually the result of underlying wear and tear damage and degenerative changes. Often patients have had preceding symptoms of pain and weakens in the front of the shoulder passing down into the biceps muscle.
- When an LHB rupture occurs, there is usually an acute episode of pain and discomfort associated with bruising and swelling. However, in most cases the pain settles very rapidly over a couple of weeks. Following this most patients have no problems with residual pain or weakness, although some are left with a symptomless ‘popeye’ sign. As a result, most patients do not require any specific treatment following an LHB rupture.
- However, there are a small group of patients who continue to have problems and concerns following an LHB rupture. These may be due to strength and function (athletes, weight-lifters etc), cosmetic appearance or stump pain over the end of the ruptured tendon. For this group of patients, a Sub-Pectoral Bicpes Tenodesis is a good treatment option.
Sub-Pectoral Biceps Tenodesis for a Ruptured LHB
- Unlike symptomatic LHB, where the tendon is in continuity, the only position that a Tenodesis can be undertaken following a rupture is at the Sub-Pectoral position
- Prior to undertaking a Sub-Pectoral Tenodesis for a ruptured LHB tendon it is important to undertake and MRI or US scan to identify the exact position where the ruptured tendon has ended up
- For longer standing ruptures an MRI or US scan is required to see whether it is technically possible to undertake the surgery successfully
A Sub-Pectoral LHB Tenodesis can usually be done as a Day Case procedure. The patient’s shoulder does not usually need to be immobilized for any significant time afterwards. The surgery aims to to locate the ruptured tendon, freshen the ends and re-suspend the tendon at the correct tension on the shaft of the humerus, just below the Pectoralis Major tendon. Recovery is usually fairly rapid and within 4 - 6 weeks most patients have gained the full benefits of the procedure. It has a high success rate with around 90% of patients being happy with the result 3 - 6 months after their operation. My routine LHB Tenodesis Procedure for a ruptured LHB tendon is described below,
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….Find out more about an Interscalene Nerve Block….
- The procedure is undertaken as an open operation
- A 3cm longitudinal incision is made in the crease of the axilla and, retracting the Deltoid superiorly, dissection taken down onto the shaft of the humerus
- Occasionally this incision has to be extended depending on the extent and chronicity of the tendon retraction
- The LHB tendon is identified, and having been cut proximally, pulled out of the wound
- A whip-stitch is then sutured from the musculotendinous junction of the biceps about 1.5cm up the tendon. The rest of the redundant tendon is then cut and discarded
- The suture ends are then passed through the Biceps-Button which is mounted onto an introducer
- The shaft of the humerus is then exposed and a 4mm hole drilled through the cortex just below the pectoralis major
- The loaded Biceps-Button is then inserted through the drill hole in the humeral shaft. The button is then ‘flipped’ within the medullary canal of the bone and the sutures tightened through the button. This brings the end of the tendon onto the bone and the construct is tightened to an appropriate tension
Find out more about the biceps button….
find out more about having an operation….
After the Surgery
Post-Operative Care
Following an LHB tenodesis the patient is usually able to go home on the same day as their surgery. However, this may vary if any additional procedures have also been undertaken at the same time. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Shoulder Physiotherapy….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves from using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person. If any additional procedure has been undertaken at the same time, the rehabilitation protocol for that procedure would usually supersede that of the Tenodesis.
| Post op | |
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| 3 Months |
|
| Milestones | |
| Week 2 - 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Weight Training |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An LHB Tenodesis for a ruptured tendon is usually a very successful procedure and most people notice a significant improvement in their pain and cosmesis within 4 weeks. Patients may notice considerable bruising over their biceps muscle if an extensive dissection has been required to mobilise the tendon stump.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection – Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.
Find out more about Outcome Measures and the SOS system ….