Supraspinatus Tendonitis – Treatment
Management of Supraspinatus Tendonitis (Impingement)
The vast majority of patients with a Supraspinatus Tendonitis can be successfully treated non-operatively with a combination of NSAIDs (Non-Steroidal Anti-Inflammatory Drugs) and Physiotherapy.
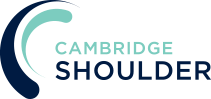
- Physiotherapy – Physiotherapy and specific Rotator Cuff Strengthening exercises are the main-stay of the initial treatment for Supraspinatus Tendonitis. By specifically strengthening the Supraspinatus muscle it can work and contract more efficiently pulling the humeral head downwards and allowing the tendon to move more freely. If pain is a particular feature a short course of NSAIDs prescribed by a Physician can help.
find out more about Rotator Cuff Strengthening Exercises….
- Analgesia/Pain Relief
- NSAID (Non-Steroidal Anti-Inflammatories) –
- NSAIDs work be reducing the painful inflammatory response, they are useful at all Stages of Frozen Shoulder
- NSAIDs can damage the stomach lining and affect the kidneys. It is important that a patient’s Family Doctor prescribes this medication if it is going to be used for a longer term
- Codeine based Analgesics –
- Codeine based analgesics are pain killers and affect a patient’s perception of pain. As a result, they can have some effect on consciousness depending on their strength
- Codeine based analgesics can lead to constipation if taken for a longer time. Having a high-fibre diet or even taking laxatives might need to be considered
- Nociceptive Analgesics –
- Nociceptive pain killers work on nerve generated pain
- Amitriptyline in lower doses works as a nociceptive pain killer. It has a useful side-effect in that it can make patients drowsy
- in cases of severe pain Amitriptyline can be prescribed at night
Subacromial Cortisone Injection –
- If someone’s Supraspinatus Tendonitis has failed to settle, after an adequate course of Physiotherapy, a Subacromial Cortisone injection can help to settle the symptoms down. Cortisone is a corticosteroid that is naturally produced by the body’s Adrenal Gland. Injectable Cortisone is synthetically produced and has a very powerful ant-inflammatory action. When injected into the Subacromial space it has the potential of settling severe inflammation, allowing the patient to undertake their rehabilitation exercises.
- A Subacromial Cortisone can be easily administered in the Out-Patient Clinic. It is a quick and relatively painless procedure. Afterwards patients can continue with their normal day-to-day activities. Occasionally patients can feel a bit of soreness around their shoulder later that day, but this usually passes fairly quickly.
- It often takes several days before someone notices the benefits following a Cortisone injection and sometimes several weeks. The Cortisone works in the background and there is no specific requirement to particularly rest the shoulder or to do extra exercises. The full benefits of a Cortisone injection are usually felt within a month. In some cases, the Cortisone may not give any benefit, this may be an indication of the severity of the Supraspinatus Tendonitis.
- A Cortisone injection only lasts in the body for a few days. Any benefit that someone gets from the Cortisone will be from its acute anti-inflammatory effect allowing the Supraspinatus Tendonitis to settle. If the symptoms do return after a while, it is not because the Cortisone has worn off, but because the inflammation has returned.
- Infections can occur after any type of injection but are extremely rare (1 in 15,000). If someone feels that they are developing an infection within 48 hours of a Cortisone injection they should seek advice from their Family Practitioner.
- Surgery for Supraspinatus Tendonitis – In some instances a Supraspinatus Tendonitis fails to respond, or continues to recur, despite adequate Physiotherapy and Cortisone treatment. In this situation the only treatment that is likely to settle the symptoms is Surgery.
Arthroscopic Subacromial Decompression
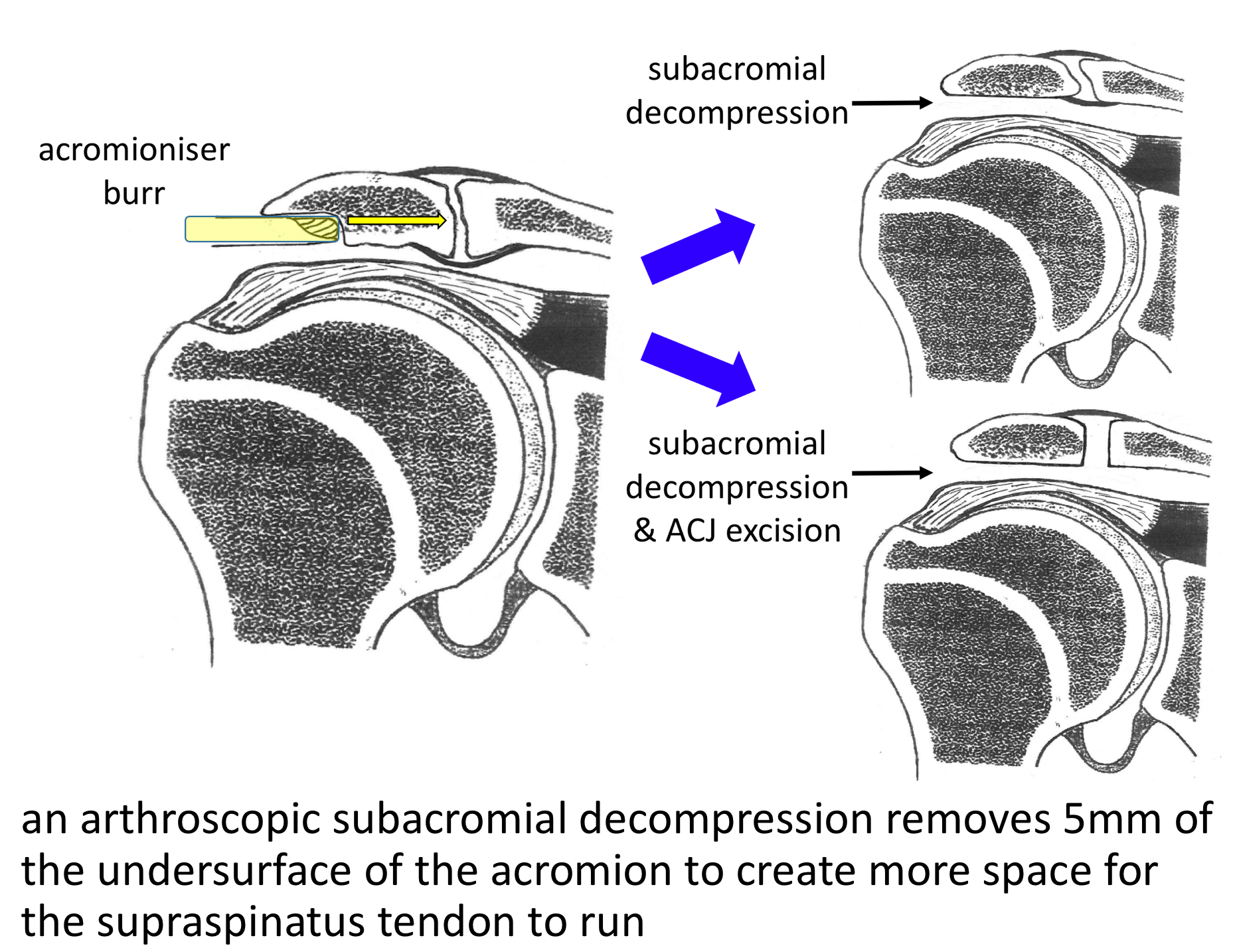
The best operation for someone with a Supraspinatus Tendonitis, that is refractory to treatment, is an Arthroscopic Subacromial Decompression. This is an operation where an Arthroscopic camera is positioned inside the Subacromial Space and, by using specialized instruments, the undersurface of the front of the acromion is burred away. This creates more space for the Supraspinatus Tendon to run underneath the Acromion stopping the Impingement.
An Arthroscopic Subacromial Decompression can usually be done as a Day Case procedure and the patient’s shoulder does not need to be immobilized for anytime afterwards. The surgery aims to remove the part of the Acromion that has been causing the Impingement. It does not specifically deal with the underlying tendonitis. However, by enabling the Supraspinatus Tendon to run freely it allows for the Tendonitis to settle down. As a result it usually takes between 3 – 6 months to gain the full benefits of the procedure. It has a high success rate with around 95% of patients being happy with the result 6 months after their operation. My routine Arthroscopic Subacromial Decompression Procedure is described below,
Watch a video of an Arthroscopic Subacromial Decompression…
Find out more about arthroscopic shoulder surgery….
- The patient is anaesthetised with a general anaesthetic and interscaelane nerve block
Find out more about having an anaesthetic….
Find out more about an Interscalene Nerve Block….
- A posterior and a single lateral portal are used for to view the Gleno-Humeral Joint (Shoulder Joint) and Subacromial spaces
- The Glenohumeral Joint is initially assessed to look for any other problems that might be associated with a Supraspinatus Tendonitis and, in particular, the Rotator Cuff and the Long Head of Biceps
- The Subacromial Space is then entered and the undersurface of the Acromion identified.
- A lateral portal is then created
- Using a combination of a powered shaver and radiofrequency probe the coracoacromial ligament is released, revealing the Subacromial Spur.
- A powered burr is then used to resect about 5mm of bone from the undersurface of the acromion
- The Decompression is then assessed to check that sufficient bone has been resected to alleviate the Impingment
- Again the Rotator Cuff is examined to check for any hidden fraying or damage
- If any significant damage is found to the Rotator Cuff this will be then also be repaired
- The Subacromial Space is then washed out and the wounds closed with sub-cuticular sutures
find out more about having an operation…
After the Surgery
Post-Operative Care
Following an Arthroscopic Subacromial Decompression the patient is usually able to go home on the same day as their surgery. I would see the patient after the surgery to discuss how the procedure has gone and arrange for further Follow-Up. The patient will be seen by the In-Patient Physiotherapy team, who will instruct them on the initial Rehabilitation Protocol for their shoulder. Further Out-Patient physiotherapy will then be organised.
Find out more about Physiotherapy following an ASD….
I would usually review patients in the clinic 1 month and 3 months after their procedure to assess their progress and recovery.
Rehabilitation Protocol
Immediately after the surgery, when the patient has woken up from their general anaesthetic, their shoulder and arm will be numb from the interscalaene nerve block. This will usually last for 18 – 24 hours after the surgery. For this period, we advise patients to keep their arm in a sling, purely for protection. After the nerve block has worn off the arm can begin to be taken out of the sling. I encourage patients to wean themselves off of using the sling as quickly as possible, within the limits of discomfort.
My standard rehabilitation protocol is outlined below. The information and time to recovery are a general estimation and may vary from person to person.
|
Post op |
|
| Immediate |
|
| Day 1-3
Weeks |
|
| 3-6 Weeks |
|
| Milestones | |
| Week 3 | Full passive range of movement |
| Week 6 | Full active range of movement, good scapular control |
|
Return to Functional Activities |
|
| Driving |
|
| Swimming |
|
| Golf |
|
| Racquet Sports/Repeated |
|
| Overhead Activities | |
| Lifting | As able |
| Work | Sedentary - As able |
| Manual - 6 weeks, may need to modify activity for 3 months | |
Success of Surgery, Risks & Complications
An Arthroscopic Subacromial Decompression is usually a very successful procedure but, because the surgery is only aimed at removing the spur of bone that has been impinging on the Supraspinatus Tendon, it usually takes between 3 – 6 months for the Tendonitis to settle and for the Shoulder to return to normal. For a standard Arthroscopic Subacromial Decompression>95% of patients’ will be happy with their shoulders after 6 months.
There are always risks and complications associated with any operation.
- Anaesthetic - The risks of having a General Anaesthetic and an Interscalaene Nerve Block are very low, but will always need to be assessed on an individual basis by an Anaesthetist. Suffice it to say, that whilst a Shoulder Operation can in no way be considered a ‘life-saving’ procedure, an Anaesthetist would not consider undertaking an anaesthetic if they had any concerns that an undue risk was being taken.
- Infection –Infection following arthroscopic surgery is rare < 0.2%
- Neurovascular Injury – Damage tosignificant neurovascular structures during arthroscopic shoulder surgery is rare < 0.2%
- CRPS Type 1 – A Chronic Pain Syndrome following arthroscopic shoulder surgery is rare < 0.2%
Outcome Measures
Assessing patient outcomes following surgery, using validated scoring systems, is a very important and useful exercise.